Fig. 11.1
(a) IT knife, (b) IT knife 2, and (c) IT knife nano
Preparation
Informed Consent
Informed consent should be obtained from patients only after they have received an explanation about the nature of their cancerous disease, the indications and need for treatment, surgical techniques, other treatment modalities, potential procedural complications and their frequency, and the option to voluntary withdraw their consent. Patients with expanded-indication lesions must be told that surgical resection is currently regarded as standard therapy, and a meeting with the surgeon is desirable.
Preoperative Endoscopic Examination
This examination is essential for determining the extent of the lesion, invasion depth, and histological type. Preoperative endoscopy should be done to ensure that ESD is performed to treat the indicated lesions appropriately and to avoid residual disease and recurrence. The basic idea is to perform normal, white-light endoscopy and chromoendoscopy to determine the extent of resection preoperatively. If the extent is unclear, biopsies are taken from various points outside the cancer margin that are believed to be normal tissue. Defining the non-cancerous region and correctly determining the line of incision are important goals of the preoperative endoscopic examination. Magnifying endoscopy and narrow band imaging-magnifying endoscopy (NBI-ME) are also useful to define the lesion.
Preoperative Examination
Interview on Medical History and History of Present Illness
Patients must be interviewed in detail about their history of drug allergies, the presence of a cardiac pacemaker, cardiovascular disease, glaucoma, hypertensive disease, cerebrovascular disease, and prostatic hypertrophy. When asking about drugs that are taken on a daily basis, patients should be asked specifically about oral anticoagulants (e.g., warfarin) and various anti-platelet agents.
Blood Biochemistry and Physiological Examination
Blood type, presence of infectious diseases (e.g., HBV, HCV, HIV, and syphilis), general blood biochemistry, prothrombin time, and activated partial thromboplastin time should be checked. Cardiopulmonary screening must be conducted by performing electrocardiography (ECG), chest X-ray, and lung function tests.
Instruments
Electrosurgical Unit (ESU; Power Generator)
The high-frequency electric current in cauterization devices provides an incision wave, a coagulation wave, or a mixed wave, and, depending on the device, a mode to change the rate and timing of incision and coagulation.
The ICC-200, ICC-300, VIO300D (ERBE, Tubingen, Germany), and ESG100 (Olympus Medical Systems, Tokyo, Japan) are widely used. The Endocut mode has become standard following the emergence of these ESUs, and it is now possible to perform incisions and dissections with less frequent immediate hemorrhage. This has helped facilitate the widespread use of ESD.
Regardless of which ESU or mode is used, the optimal settings depend on the target lesion and the type of local injection solution used. It is important, therefore, for the endoscopist to choose the proper output mode. For reference, the authors use the following settings for the stomach. With the VIO300D, incision is made using Endocut, Effect 2, Cut duration 2, and Cut interval 2, and submucosal dissection is performed using Swift coagulation and Effect 4 or 5 at 100 W.
Endoscopes
Standard Endoscopes for ESD
Most ESD procedures can be performed under direct visualization using a normal single-channel scope. However, it may be preferable in some cases to use a 2-channel scope.
Scopes Equipped with an Auxiliary Water Jet (Fig. 11.2a)
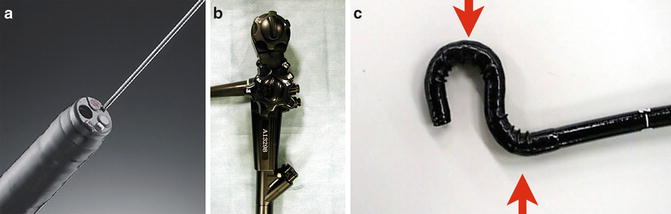
Fig. 11.2
(a) Endoscope with an auxiliary water jet function. (b) A multibending scope with two independently curving segments
An auxiliary water jet helps to maintain a clear view during ESD by flushing water from a nozzle at the tip of the endoscope into the immediate operative field during hemorrhage. This feature can even be used with the device for incision or hemostasis still being within the accessary channel, and so helps to prevent perforation or mucosal incision by flushing a surgical field when obscured by blood. It is also extremely useful for pinpointing and confirming petechiae (a potential source of bleeding). Water-jet enabled scopes allow ESD to be performed safely and quickly.
Multi-Bending Scope (Fig. 11.2b)
To secure the position of a normal scope in difficult-to-operate sites, such as the lesser curvature in the lower gastric body and the anterior wall in the upper body, the multi-bending scope is provided with an additional flexure in front of the normal flexure. It is advisable to prepare the use of one of these multi-bending scopes when performing ESD if available.
Incision and Dissection Devices
IT Knife (Insulation-Tipped Diathermic Knife)
A ceramic ball is attached to the tip for insulation, and the knife is used for incision and dissection with the blade placed in a horizontal orientation.
These Other Knives Are Classified as So-Called Tip Knives
Examples include: Hook knife, Dual knife, Flush knife, and Hybrid knife.
Intraprocedural Monitoring
Intraprocedural monitoring is essential during ESD. At a minimum, blood pressure, degree of oxygen saturation, ECG, and pulse should be monitored.
ESD Procedure
The ESD procedure, as a rule, involves a circumferential incision being made around the lesion and submucosal dissection. The actual process may differ depending on the devices used and required experience.
When using IT knife, the basic movement is from distal to proximal direction (Fig. 11.3).