Ideal SFC solution characteristics
Cost
Inexpensive
Clarity
Transparent enough to help identify submucosal structures
Local and systemic toxicity
Non-toxic
Availability
Readily in bulk
Storage
At room temperature and no need for refrigeration while in transport
Handling
Does not require mixing with other solutions other than dilution, can be sterilized without degrading
Viscosity
Fluid outside of the body
Ease of injection
Easily injected through a standard sclerotherapy needle
Length of stay in the submucosal space
Entire duration of the EMR/ESD, or long enough to keep the number of re-injections low
Electroconductivity
Almost impenetrable, does not conduct electricity well
Additional ideal local tissue effects
Promotes ulcer healing, hemostatic, ability to separate tissue planes, softens connective tissue to facilitate blunt dissection, no char artifact after electrocauterization
The Mayo Clinic Developmental Endoscopy Unit (DEU) has been active in SFC research. Initial efforts at testing solutions resulted in the recognition that the ex vivo animal model was unreliable to assess solution performance. The ex vivo model can often be useful for preliminary testing of concepts, materials and methods, but fluid performances in unperfused tissue cannot be reliably translated to clinical application. Conio, Rajan et al., in 2002 [6], compared five injection solutions in an in vivo porcine model. The fluids compared were: saline, saline with 1:10,000 epinephrine, 50 % dextrose (D50), rooster comb-derived hyaluronic acid, and 10 % glycerin. Glyceol, at that time, was only commercially available in Japan (Chugai Pharmaceutical Co.) and consisted of 10 % glycerin and 5 % fructose in normal saline. All the test solutions had indigo carmine dye added and were injected into the distal esophagus at room temperature. The elapsed time for the subcutaneous bleb to disappear was measured. The disappearance time for normal saline (median of 2.4 min) was significantly shorter than the other solutions, except normal saline with epinephrine, which correlates with clinical observations. D50 and 10 % glycerin dissipated 2 min later than normal saline. Hyaluronic acid had a median of 22.1 min, making it significantly longer lasting than all the other solutions. Long before ESD was conceptualized, this paper was intended to identify the most suitable SFC solution for EMR and piecemeal polypectomy. As a result of this study, D50 became the SFC solution of choice in our clinical practice in Rochester, Minnesota until the next discovery.
Later that same year, Feitoza, Gostout et al. [7], published a report on the use of another submucosal fluid cushion for EMR, hydroxypropyl methylcellulose (HPMC). The group already saw the value of a long-lasting SFC to facilitate lengthy EMR and polypectomy procedures. The prohibitive cost, lack of availability, and lack of regulatory approval of hyaluronic acid prompted them to look for an alternative SFC injectate [8]. One day in the DEU animal lab, a surgical lubricant was tried in an injectable dilute form and proved to offer an astounding SFC. Unfortunately, all the commercially available formulations of surgical lubricants are made of multiple ingredients and not approved for injection. The most significant component of these was identified as methylcellulose. HPMC is commonly used as an ophthalmic solution during anterior chamber operations. This formulation of methylcellulose was chosen due to its viscoelastic properties and approved for injection. In contrast to HA, HPMC was inexpensive and readily available in a generic 2.5 % solution commonly sold as eye drops. This feasibility study was done to observe the safety, durability and tissue response to submucosally injected HPMC. Results showed that HPMC stayed in the submucosal space up to 45 min and induced minimal tissue reaction on histopathology. A diluted solution of 0.83 % of HPMC can be easily injected into the esophageal wall to create a long-lasting SFC at low cost.
By the year 2004, Rajan and most of the Apollo 8 group published a report on Widespread EMR (WEMR) of the distal esophagus in a porcine model [9]. The SFC used was 0.83 % HPMC. There was no procedure-related complication. It emphasized the importance of a long-lasting protective SFC in prolonged procedures. The SFC fluid duration was approximately 35 min.
In 2007, Sumiyama and Gostout published on novel techniques for WEMR and ESD [10]. It was noted that in the Mayo Clinic, HPMC had replaced D50 and was clinically used as the SFC solution of choice, in contrast to HA, due to cost effectiveness and ease of storage and handling. ESD was just being described in Japan during this period and the SFC solution of choice used in Japan was hyaluronic acid.
The DEU also originally reported the concept of using the submucosa as a working space for endoscopic intervention. Converting the submucosa into a tunnel can offer safe entry into sterile spaces such as the peritoneal cavity and mediastinum. Off-set entry from the lumen, passage through a submucosal space or tunnel, and a myotomy distal exit prevents peritoneal soiling, by allowing the overlying mucosa to serve as a sealant flap (submucosal endoscopy with mucosal flap or SEMF). Early experience used high pressure carbon dioxide injection supplemented with careful electrosurgical dissection to tunnel relatively easily. The concept of submucosal endoscopy, originally referred to as the Submucosal Inside Out Project (SIOP) [10], was actually initiated to simplify mucosal resection as a more expedient alternative to EMR and ESD that might enable more endoscopists to perform widespread mucosal resection (Fig. 8.1). With this approach, mucosal disease is first undermined by a submucosal free space. The endoscope and endoscopic devices within this space are directed toward the lumen away from the muscularis propria, thereby reducing full thickness injury by this reversed direction of intervention. Submucosal endoscopy with mucosal flap (SEMF) and submucosal endoscopy with mucosal resection (SEMR) have evolved into many practical uses, specifically in natural orifice transluminal endoscopic surgery (NOTES), per-oral endoscopic myotomy (POEM) and endoscopic full thickness resection (EFTR). Both submucosal techniques fundamentally require a reliable SFC for initiation [11].
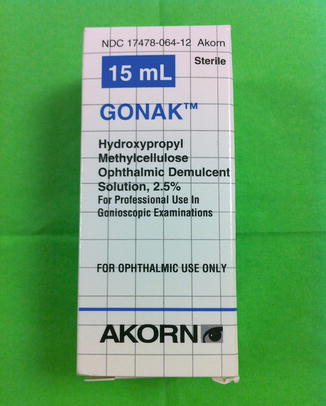
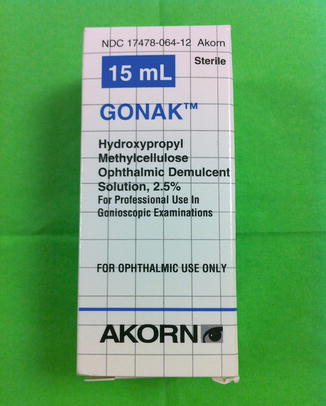
Fig. 8.3
Gonak ophthalmic solution, undiluted, prior to preparation
Whether one is performing traditional EMR, or ESD, or SEMF or SEMR, the SFC is critical. Work in the DEU was directed at trying to identify an adjunctive material to the SFC solution that could further facilitate all these procedures. Sumiyama, Gostout, and Rajan published a report on chemically assisted endoscopic submucosal dissection using mesna [12]. Mesna is a thiol compound, sodium-2-mercaptoethanesulfonate, originally developed to define surgical planes. Mesna is a mucolytic solution whose action is to disrupt disulfide bonds, making mucus less viscous and connective tissues weaker. Mesna significantly (p > 0.05) reduced tissue resistance to balloon-catheter insertion in submucosal dissection. Mesna was added to 0.83 % HPMC and was compared to HPMC alone.
En bloc resection may be of more value in North America to remove advanced colorectal polyps, especially large sessile or laterally spreading lesions. The most common procedure in sessile polyps >2 cm is piecemeal resection which carries a significant risk of residual adenoma and repetitive endoscopies. Traditional ESD is more challenging in the colon, with a greater risk of bleeding and perforation compared to piecemeal resection. ESD is time-consuming, sub-optimally reimbursed, and requires advanced endoscopic skills. SEMR allows large diameter resections; in the rectum of a porcine model, up to 8 cm. This hybrid ESD procedure is heavily reliant on a robust submucosal fluid cushion to allow isolation of the mucosal disease and facilitate the balloon dissection unique to this method. In the initial reported animal study, the combination of HPMC 0.83 % and mesna was used. The SEMR method was compared to traditional ESD performed by a Japanese expert in ESD, and was found to be less technically demanding than the traditional ESD procedure with a shorter learning curve. SEMR or hybrid ESD could open the opportunity for more endoscopists to perform en bloc resection of ESD proportions.
In 2013, an off shoot of SIOP, primary mechanical submucosal balloon dissection, was advanced by Dobashi, Sumiyama and colleagues. An engineered balloon dissector or the SuMO (Apollo Endosurgery, Austin TX, USA) was used to cleave submucosal fibrosis in an ulcerated lesion in a porcine model (Fig. 8.2). Submucosal fibrosis clinically presents a situation which frustrates the ability to create an effective SFC [13].
Fig. 8.1




Submucosal inside out project (SIOP)—concept of submucosal endoscopy: (a) A submucosal tunnel can allow safe access to body cavities. (b) Submucosal tunneling can undermine overlying mucosal disease for en bloc excision. (c) Submucosal endoscopy is dependent on the SFC. (d) Hybrid ESD can be performed using blunt balloon dissection in lieu of conventional electrosurgical cutting. (e) Blunt balloon tunneling undermines overlying mucosal disease completely. (f) Blunt balloon dissection is extended beyond the tunnel to completely undermine overlying mucosal disease and is dependent on an isolating circumferential excision. (g) In hybrid ESD, conventional electrosurgical excision is combined with balloon dissection. (h) In hybrid ESD, the combination of balloon dissection and electrosurgical excision is carried out to the excised margins of the lesion for an en bloc removal
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







