Procedure
Year
Author
Country
Route
Number
Operation time (min)
Complications
Cholecystectomy
2008
Rao et al
India
Transvaginal
3
NA
None
2009
Palanivelu et al
India
Transvaginal
8
148
1 subhepatic collection
Combination of a flexible endoscope and a 3-mm trocar for retracting the gall bladder. Two conversions to laparoscopic cholecystectomy
2009
Rudiman et al
Indonesia
Transvaginal
1
128
None
Transvaginal endoscope and two trocars (5 and 2 mm)
2010
Sohn et al
Korea
Transvaginal
1
86
None
Use of a wound retractor with a glove for vaginal access
2011
Niu et al
China
Transvaginal
43
87
None
Transvaginal endoscope and a 5-mm umbilical trocar
Appendectomy
2008
Rao et al
India
Transgastric
10
NA
1 ileus
Two conversions to laparoscopic appendectomy
2008
Palanivelu et al
India
Transvaginal
6
103
None
Three conversions to laparoscopic appendectomy
2010
Shin et al
Korea
Transvaginal
1
60
None
Transvaginal endoscope and a 5-mm umbilical trocar
Peritoneoscopy
2008
Kitano et al
Japan
Transgastric
1
NA
None
Transgastric submucosal endoscopy
2013
Lee et al
Korea
Transgastric
5
33
None
Transgastric submucosal endoscopy
2013
Chen et al
China
Transgastric
7
30
None
1-cm-long full-thickness gastric incision
Local resection of the stomach
2009
Nakajima et al
Japan
Transvaginal
2
365, 170
None
Transvaginal endoscope and two trocars
2009
Abe et al
Japan
Transoral
4
201
None
Endoscopic full-thickness resection with laparoscopic assistance
2011
Mori et al
Japan
Transoral
6
288
None
Endoscopic full-thickness resection with laparoscopic assistance
2011
Cho et al
Korea
Transoral
14
143
1 gastric stasis
Endoscopic full-thickness resection with laparoscopic assistance and laparoscopic regional lymph node dissection. Five conversions to gastrectomy
2013
Lee et al
Korea
Transgastric
5
33
None
Transgastric submucosal endoscopy
Peroral endoscopic myotomy
Specimen extraction after colectomy
2010
Inoue et al
Japan
Transesophageal
17
126
None
Transesophageal submucosal endoscopy
2013
Lee et al
Korea
Transesophageal
13
NA
None
Transesophageal submucosal endoscopy
2013
Minami et al
Japan
Transesophageal
28
99
None
Transesophageal submucosal endoscopy
2013
Li et al
China
Transesophageal
103 vs 131
41 vs 48
1 vs 1
Full-thickness myotomy vs circular muscle myotomy
2008
Palanivelu et al
India
Transvaginal
7
222
1 ileus, 1 pouchitis, 1 deep vein thrombosis
Laparoscopic proctocolectomy
2012
Cheung et al
China
Transrectal
1
NA
None
Laparoscopic right colectomy
Adrenalectomy
2011
Zou et al
China
Transvaginal
11
102
None
Transvaginal laparoscope and two trocars (10 and 5 mm). One conversion to open surgery
Thyroidectomy
2013
Nakajo et al
Japan
Transoral
8
208
8 sensory disorders around the chin, 1 laryngeal nerve palsy
Trans-oral video-assisted neck surgery
Cholecystectomy
The most reported NOTES procedure is cholecystectomy. Five different authors have published their experiences with transvaginal cholecystectomy [9–13]. The largest NOTES cholecystectomy series in Asia was reported by Niu et al. from China [13]. They retrospectively compared the clinical results of 43 transvaginal cholecystectomies with those of 48 conventional laparoscopic cholecystectomies. Transvaginal cholecystectomy was performed with a transvaginal flexible endoscope, a 5 mm laparoscopic grasper introduced through the vagina for retraction of the gallbladder, and a single umbilical trocar. The cystic duct and artery were clipped with laparoscopic clips through the umbilical trocar. Transvaginal cholecystectomies were successfully completed in all patients without conversion to conventional laparoscopic surgery, and there were no intra- or postoperative complications in any patients. The operation time for the NOTES cholecystectomies was longer than that of conventional laparoscopic cholecystectomies (87 vs. 60 min, P < 0.05). However, postoperative pain, hospital stay, and the cost of hospitalization with NOTES were less than those with the conventional laparoscopic operation. Sohn et al. from Korea applied a single-port access system with a wound retractor and a surgical glove at the vaginal port to improve operation efficiency [12]. Their mean operation time was 86 min.
All other series were performed in a hybrid fashion using laparoscopic assistance with one or two trocars, and no serious complications were reported. The additional trocar seems to be an optimal way to perform NOTES cholecystectomy safely and easily at the present time with the current lack of availability of NOTES-specific devices.
Appendectomy
Rao and Reddy from India were the first in the world to perform a transgastric appendectomy [9]. Appendectomies were completed using a double-channel endoscopes without laparoscopic assistance. Transgastric access was achieved with a needle knife and balloon dilation. The mesoappendix was dissected using a hot biopsy forceps with monopolar coagulation current. The appendix was secured with an endoloop and then transected using a polypectomy snare. The gastric access site was closed with multiple endoscopic clips. Two out of ten cases required conversion to conventional laparoscopic operation. Postoperative ileus was noted in one patient and needle knife injury to the abdominal wall in one other.
Palanivelu et al. from India reported 6 attempts at pure NOTES appendectomy with two patients requiring laparoscopic assistance and three requiring conversion to conventional laparoscopic operation [14]. There were no complications, and the hospital stay averaged 1–2 days.
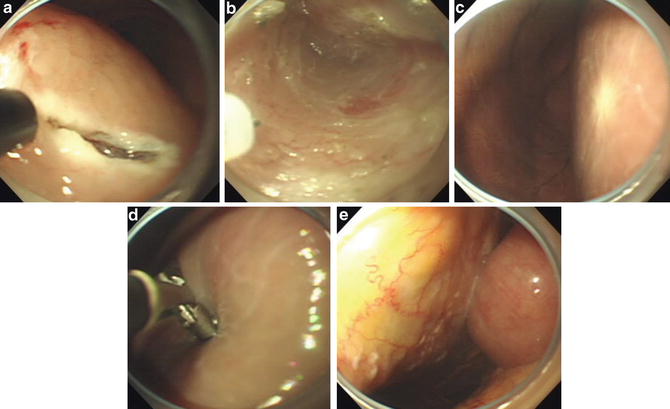
Peritoneoscopy
Kitano, Yasuda et al. performed transgastric peritoneoscopy for preoperative staging in a pancreatic cancer patient in 2008 [16]. This was the first case of NOTES performed in Japan. The submucosal tunneling technique was used in combination with ESD methods, after confirming the safety and feasibility of this technique in experimental studies [31–34]. After injection of normal saline solution into the gastric submucosal layer, a 2 cm incision of the mucosa into the submucosal cushion was created (Fig. 22.1a). Dissection of the submucosal layer was then carried out with an ESD knife to make a narrow longitudinal submucosal tunnel approximately 5 cm long (Fig. 22.1b). A small incision of the seromuscular layer was made at the end of the submucosal tunnel, and the opening was enlarged with an endoscopic dilation balloon. The endoscope was then advanced into the peritoneal cavity through the tunnel, which provided an excellent view. After we confirmed no hepatic or peritoneal metastasis, the patient underwent a standard open operation without complications. We have performed 14 cases of transgastric submucosal peritoneoscopy. In some cases, peritoneal or liver metastasis was able to be diagnosed with transgastric peritoneoscopy before operation (Fig. 22.1c–e).