Chapter 51 EPIDEMIOLOGY OF PELVIC ORGAN PROLAPSE
EPIDEMIOLOGY
Although pelvic organ prolapse (POP) is one of the most common indications for gynecologic surgery, little is known about the epidemiology of the condition.1 Caring for women with pelvic floor disorders has become an increasingly important component of women’s health. An analysis of U.S. procedure codes for prolapse surgery estimates that more than a half-million procedures are performed annually accounting for more than 1 billion US health care dollars.2 It is estimated that women have an 11% lifetime risk of undergoing a single operation for POP and urinary incontinence by age 80 years.3 Studies have shown that 50% of parous women lose pelvic floor support, with resulting prolapse.3 Yet, of these women, only 10% to 20% seek medical care. The Oxford Family Planning Association study monitored more than 17,000 women aged 25 to 39 years for 26 years.4 Whereas the annual incidence of hospital admission for the diagnosis of prolapse was 0.204%, the annual incidence of surgery for prolapse was only 0.162%.4 This highlights the fact that only a fraction of women with POP seek medical attention. Therefore, incidence and prevalence rates based on surgical intervention significantly underestimate the magnitude of POP.
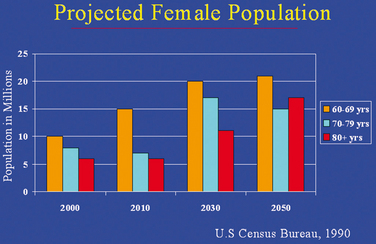
Given the difficulties in determining the number of women affected by POP, there has been little agreement on the resources needed to serve this population. It is estimated that the proportion of the U.S. population between the ages of 30 and 89 years will grow by 22% over the next 30 years (Fig. 51-1).5,6 One of the most dramatic features of this population change is the large increase in the number of Americans older than 50 years of age. The population of women aged 50 years and older is expected to increase by 72%. Luber and colleagues found that women aged 60 years and older are far more likely to seek medical care for pelvic floor disorders than their younger cohorts.6 They estimated that, over the next 30 years, the demand for services to care for female pelvic floor disorders will increase at twice the rate of growth of the general population (Fig. 51-2). Therefore, at a time when the general population is projected to increase by 22%, there will be a 45% increase in the demand for care for pelvic floor disorders.6
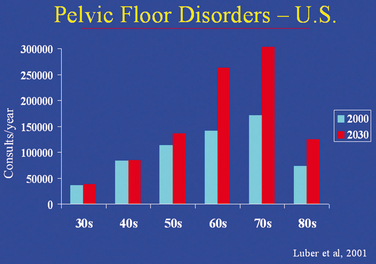
Figure 51-2 Estimated increase in pelvic floor disorders among women aged 30 to 80 years.
(From Luber KM, Boero S, Choe JY: The demographics of pelvic floor disorders: Current observations and future projections. Am J Obstet Gynecol 184:1496, 2001.)
One of the reasons that the demographics of POP are so poorly understood is that its prevalence varies widely in different populations, ranging from 30% to 93%. Differences in prevalence and incidence rates may be explained by varying diagnostic criteria, different examination techniques, and the sensitivity of these techniques. Before 1995, one of the main problems in studying the epidemiology of POP was the absence of a standardized tool for evaluating the degree or stage of POP. In 1996, an international committee comprised of members from the International Continence Society (ICS), the American Urogynecologic Society, and the Society of Gynecologic Surgeons met to develop an objective, site-specific system to describe, quantify, and stage female POP.7 The result was the Pelvic Organ Prolapse Quantification system (POPQ). The creation of this classification system was a major advance in the study of POP, allowing researchers to report findings in a standardized fashion. The POPQ has demonstrated good reliability as well as intraexaminer and inter-examiner reproducibility.8
A second reason for lack of understanding of the epidemiology of POP is that there have been no epidemiologic studies of POP in community-based populations.9 Instead, most studies are based on small, mainly white clinical populations or surgical databases. An additional limitation in understanding the epidemiology of POP is inherent to the condition itself. Studies on POP are wrought with difficulties. Complying with the ICS definition of POP requires an invasive examination that limits the feasibility of large community-based studies. Furthermore, symptoms associated with POP have not been shown to correspond to the severity of prolapse. This inconsistency limits the use of symptoms in the epidemiologic definition of prolapse.
Finally, lack of understanding of the distribution of normal versus abnormal female pelvic organ mobility and support remains another limitation. In a study of young nulligravid women, Dietz and coworkers found a wide range of pelvic organ mobility, concluding that the “range of ‘normality’ in pelvic organ mobility is wider than previously assumed.”10 In 2000, Swift performed an observational study on the distribution of pelvic organ support of women seen at outpatient gynecology clinics for routine gynecologic care. The distribution of POP was a bell-shaped curve, with most subjects having stage 1 or 2 prolapse.11 The overall distribution was as follows: stage 0, 6.4%; stage 1, 43.3%; stage 2, 47.7%; and stage 3, 2.6%.11 The Pelvic Organ Support Study (POSST), a multicenter, cross-sectional observational study of 1004 women undergoing annual gynecologic examinations, found a similar distribution. The prevalence of POP quantification stages was as follows: stage 0, 24%; stage 1, 38%; stage 2, 35%; and stage 3, 2%.12
PREVALENCE
The prevalence of a disease refers to the number of affected persons present in the population at a specific time divided by the number of persons in the population at that time.13 Prevalence also describes the probability of experiencing a symptom or having a condition or a disease within a defined population at a defined time.9 This is important in establishing the distribution of a condition in the population and projecting the need for future health and medical services.
The data on prevalence of POP is limited and highly variable. Many estimates of the prevalence of POP define prolapse based on symptoms alone or a nonvalidated genital examination, not on the POPQ. To date, only two studies have used the ICS definition of POP. The first, done by Swift in 2000, found that 94% of women aged 18 to 82 years had stage 1 POP or greater; when only women with stage 2 or greater were considered, the prevalence fell to 51%.11 A second study, also done by Swift and colleagues, found that 22% of women aged 18 to 83 years seeking routine gynecologic care had POP, which was detected on routine examination.12
Two other studies have looked at the prevalence of POP using physical examination; however, these studies used nonvalidated genital examination classification systems. Hendrix and associates looked at the prevalence of POP in women aged 50 to 79 years who were enrolled in the Women’s Health Initiative Hormone Replacement Therapy Clinical Trial. Forty-one percent of women with a uterus had some form of prolapse (34.3% cystocele, 14.2% uterine prolapse, 18.6% rectocele), compared to 38% of the women without a uterus (32.9% cystocele, 18.3% rectocele).14 In the second study, Samuelsson and colleagues examined Swedish women aged 20 to 59 years and found the overall prevalence of genital prolapse to be 30.8%.15 In comparison, the prevalence studies of POP based on symptoms alone tend to report lower rates of POP, ranging from 7% to 25%.16–18 This discrepancy in prevalence rates highlights the lack of correlation between POPQ and prolapse symptoms.
INCIDENCE
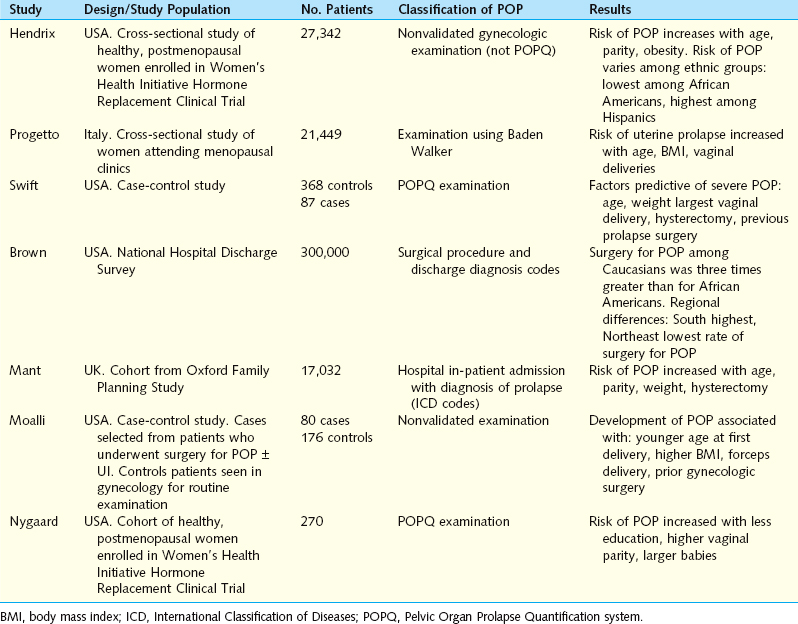
The incidence of a disease is the number of new cases of a disease that occur during a specified period of time in a population at risk of developing the disease or the probability of developing the condition under study during a defined time period.13 Studies of the incidence of POP come primarily from surgical databases (Table 51-1). Cases are identified by the International Classification of Diseases (ICD) diagnosis and procedures codes. In the United States, the annual incidence of surgery for POP ranges from 1.5 to 4.9 cases per 1000 women.3,19,20 Olsen and coworkers looked at the incidence of POP surgery in a managed care setting. They found that the age-specific incidence of surgically managed POP increased with age (Fig. 51-3); with the overall lifetime risk of a woman’s undergoing at least one operation for POP being 11.1%.3
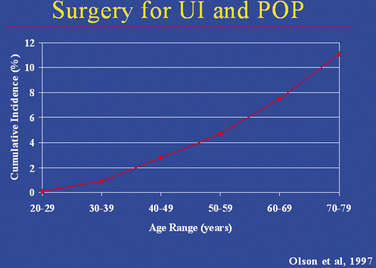
Figure 51-3 Lifetime risk of undergoing surgery for urinary incontinence (UI) and pelvic organ prolapse (POP).
(From Olsen AL, Smith VJ, Bergstrom JO, et al: Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501, 1997.)
In 1997, Brown and associates20 calculated the incidence of surgery for POP from the National Hospital Discharge Survey and National Census records of 225,964 women to be 22.7 per 10,000 women. The rate of prolapse surgery increased with age, peaking at age 60 to 69 years with a rate of 42.1 per 10,000 women. Interestingly, rates for surgery varied significantly by region. Women living in the South had the highest overall rate of surgery for POP (29.3 per 10,000), whereas women living in the Northeast had the lowest overall rate of surgical intervention (16.1 per 10,000; see Fig. 51-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree