Chapter 34 Endoscopic Management of Upper Gastrointestinal Familial Adenomatous Polyposis Syndrome and Ampullary Tumors
Introduction
Classic familial adenomatous polyposis (FAP) is an autosomal dominant condition caused by mutation in the adenomatous polyposis coli (APC) gene that results in profuse adenomatous polyposis of the gastrointestinal (GI) tract, most marked in the colon. Attenuated FAP is associated with a smaller number of polyps in the colon and upper GI tract. The MUTYH mutation causes a recessively inherited polyposis condition, MUTYH-associated polyposis, which is characterized by a slightly increased risk of developing colon cancer and adenomas in both the upper and the lower GI tract. Patients with FAP and its variants generally undergo prophylactic colectomy during adolescence or early adult life. After colectomy, the proximal duodenum is the most common site of malignancy in FAP subjects.1 The periampullary region is especially prone to adenomatous change, presumably related partly to the trophic effects of bile on the mucosa.2–5 Duodenal adenomas develop in 40% to 100% of FAP patients. Less commonly, periampullary adenomas are sporadic (arising in non-FAP patients).
Familial Adenomatous Polyposis Syndrome
FAP is an autosomal dominant condition with virtually complete penetrance, affecting approximately 1 in 8000 in the United States.6 Mutation of the APC gene on the long arm of chromosome 5 is responsible for most cases of FAP.7 The condition is classically characterized by the development of hundreds to thousands of adenomatous polyps in the colon with the inevitable progression of one or more of these adenomas to carcinoma. It is increasingly apparent, however, that an attenuated form of FAP exists. These patients generally present with fewer colorectal polyps developing later in life compared with classic FAP and often distributed more proximally in the colon. These patients develop upper GI disease, and the upper GI findings may be more marked in some patients than the findings in the colon.8,9 Mutations in particular regions of the APC gene account for the attenuated forms of FAP.8,10,11
Extracolonic disease is common in classic FAP but varies in severity from family to family and between individuals within families. At one extreme is Gardner’s syndrome, characterized by GI adenomatous polyps with other benign neoplasms, such as desmoid tumors, osteomas, and fibromas.12 Gardner’s syndrome also results from germline APC mutations and is best regarded as part of the spectrum of FAP. Turcot’s syndrome is characterized by central nervous system tumors, often glioblastomas or medulloblastomas,12 and colonic polyposis. The inheritance of this disorder has been difficult to determine12 because the association of central nervous system tumors and polyposis may arise through germline mutation of more than one gene.13 Germline APC mutations have been identified in some patients with Turcot’s syndrome, particularly patients with cerebellar medulloblastomas and profuse colonic polyposis.13 For the purposes of this chapter, the term FAP incorporates Gardner’s syndrome and cases of Turcot’s syndrome attributable to APC mutations.
The colonic manifestations of FAP are cured by colectomy (although a risk of rectal cancer remains after ileorectal anastomosis or in any residual rectal mucosa after restorative proctocolectomy). After colectomy, extracolonic manifestations of FAP assume greater importance. The entire upper GI tract seems to be at risk of malignancy in FAP.1 The duodenum is the most common site of malignancy in patients after colectomy. Duodenal cancer develops in 4.5% to 8.5% of these patients.14,15 Adenomas and carcinomas have also been encountered in the distal ileal segment and within ileoanal pouches 5 to 10 years after proctocolectomy.16
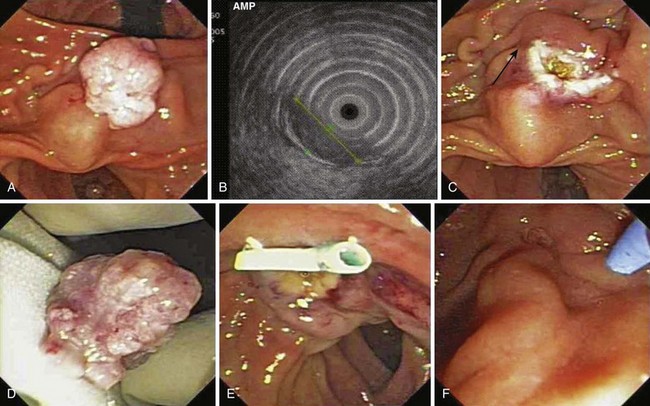
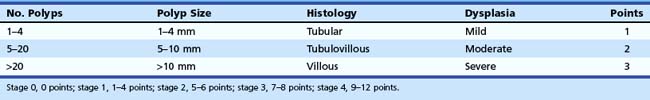
Gastric polyps are a common finding in FAP. Multiple 3- to 5-mm fundic polypoid lesions are seen in at least 50% of patients (Fig. 34.1).17 These fundic gland or fundic cystic gland polyps are hamartomatous lesions and were previously regarded as having no malignant potential. Histologic examination of fundic gland polyps reveals cystic dilation of fundic glands with generally no epithelial dysplasia.18 However, Bianchi and colleagues19 reported a series of 75 FAP patients undergoing upper endoscopic screening for adenomas. Fundic gland polyps, detected in 88% of patients and sampled by mucosal biopsy, showed dysplasia in 41% (3% with high-grade dysplasia). On multivariate analysis, the investigators found larger fundic gland polyps (>1 cm), higher Spigelman stage (Table 34.1), and antral gastritis were associated with fundic gland dysplasia. Fundic gland polyps with size greater than 1 cm had almost 16 times greater odds for dysplasia compared with polyps 1 to 4 mm in size. Acid suppressive medication use was found to be associated with a marked decrease in dysplastic fundic gland polyps.
Similar findings were noted in a series of 24 pediatric patients undergoing screening endoscopy with 51% showing fundic gland polyps with dysplasia in 42%.20 The investigators found that APC mutations between codons 1225 and 1694 may be associated with more aggressive gastroduodenal involvement in FAP. Several case reports also describe gastric adenocarcinoma arising from fundic gland polyps in patients with FAP and attenuated FAP.21–24 Although a smaller series (n = 29)21 revealed polyps (predominantly fundic gland) in 35% of patients in which all were hyperplastic without dysplasia, it is important to perform a thorough examination of the fundus to obtain a biopsy specimen or remove large fundic gland polyps (>1 cm or enlarging lesions on serial surveillance examinations) or polyps with atypical endoscopic appearances.
Gastric adenomatous polyps (predominantly in the gastric antrum) have been reported in 5% of patients with FAP in a British cohort1 and 25% in a Japanese series.25 The risk of gastric malignancy has been estimated to be 3.4 times that of controls.26 However, this report was from Japan, where the epidemiology of gastric malignancy differs from that of Western societies. In a British study of 1255 subjects with FAP and mean follow-up of 22 years, only 7 developed gastric malignancy.1 Nevertheless, just as adenomas are treated in other parts of the GI tract, if screening upper endoscopy is performed to assess for duodenal adenomas, inspection and biopsy or removal of suspected adenomas in the stomach should also be planned. Surveillance strategies of the upper GI tract for FAP patients are discussed subsequently.
Incidence of Sporadic and Familial Adenomatous Polyposis–Related Periampullary Adenomas
An understanding of the natural history of duodenal neoplasia in patients with FAP is essential to the development of surveillance strategies and decisions regarding management in this condition. Periampullary tumors represent 5% of GI tumors and 36% of resectable pancreaticoduodenal tumors.27 A periampullary adenoma is an uncommon lesion in clinical practice, although not as rare as previously thought. An early review at the Mayo Clinic by Baggenstoss28 found 25 of these lesions in 4000 consecutive autopsies (0.62%), suggesting that the lesion may be subclinical. A review of the case notes in this study suggested that only 6 (24%) of these 25 lesions might have been symptomatic.
Asymptomatic adenomatous change of the ampulla is extremely common in FAP patients, occurring in a high proportion of patients with one series showing adenoma in all of the patients studied.29 The incidence of FAP-related duodenal and periampullary adenomas depends on the diligence of screening (see section on Diagnosis later). A review of the Johns Hopkins FAP registry indicated that the relative risk of duodenal adenocarcinoma in FAP compared with the general population was 330, and the relative risk of ampullary cancer was 123.30 However, the combined absolute risk of duodenal cancer in FAP patients was only 1 per 1698 years. Because follow-up was incomplete and most cancers occurred later in life, the risk of malignancy may be underestimated. A study from the United Kingdom reported development of malignancy in 3 of 70 patients followed over 40 months.31 Although adenomatous change in the duodenum may be almost universal in FAP, only a few patients apparently develop cancer. Several studies have indicated that the median age at onset of periampullary malignancy complicating FAP is in the 6th decade.15,30,32 The literature on this subject often has inadequately differentiated sporadic from FAP-related periampullary adenomas.
Pathogenesis of Periampullary Adenoma
As an autosomal dominant condition, all nucleated cells in FAP patients contain one normal and one abnormal APC gene (a germline mutation). In the colon, a somatic mutation in the previously normal (wild-type) APC allele is generally an early event in carcinogenesis. Accumulation of other somatic mutations (in genes such as TP53 and K-ras) drives the progression toward malignancy.33 The situation with respect to periampullary malignancy seems to be similar except that somatic APC mutations may be relatively less frequent and K-ras mutations relatively more frequent.34 Another study has shown TP53 mutations associated with high-grade malignant change in periampullary tumors.27 There may be other familial factors, possibly unidentified modifier genes, that influence the development of periampullary adenomas in FAP kindreds, partly explaining the familial segregation of periampullary disease observed within FAP families.32 This segregation was independent of the specific APC mutation of the kindred.
Histology
Most periampullary lesions are tubular or tubulovillous adenomas that arise from the intestinal-type epithelium of the ampulla.35 Foci of severe dysplasia or frank malignancy may be found within a lesion.36 Other neoplasms of the ampulla are far less common; these include benign lesions (adenomyoma, leiomyoma, lipoma, lymphangioma, hemangioma, carcinoid, and paraganglioma) and primary and metastatic malignancies (lymphoma, melanoma, and metastatic small cell carcinoma).37 A retrospective study by Bleau and Gostout29 supported the temporal progression of periampullary adenomas to carcinoma, with diagnosis of adenoma at a mean age of 39, high-grade dysplasia at age 47, and malignancy at age 54.
Clinical Presentation
Lesions of the periampullary area may be asymptomatic or manifest relatively early with symptoms of pancreaticobiliary origin. Clinical presentation is usually a consequence of obstruction, resulting in abdominal pain, nausea, vomiting, cholangitis, or jaundice37 or, less commonly, GI bleeding, iron deficiency anemia, or acute pancreatitis.38 Courvoisier’s sign is occasionally present, suggesting advanced disease.39 Biochemical evidence of biliary obstruction is common in symptomatic patients.40 The diagnosis is usually unsuspected before visualization of the ampulla, with most patients thought to have pancreatic malignancy, chronic pancreatitis, or choledocholithiasis.
Endoscopic Management of Periampullary Adenoma
Endoscopic management of periampullary adenomas can be separated into diagnosis, surveillance, and therapy. Colonic involvement in FAP can be asymptomatic, patients with FAP may have no family history (new mutations), and colonic manifestations of the disease may be delayed in attenuated forms of FAP.33 For these reasons, all patients with apparently “sporadic” periampullary adenomas should undergo colonoscopy.
Diagnosis
In patients with FAP, diagnosis of upper GI and particularly periampullary adenomas requires proficiency in side-viewing duodenoscopy because forward-viewing endoscopy alone may miss 50% of gross lesions visible with the side-viewer.29,41 Patients with FAP may have adenomas beyond the ampulla that are not seen with standard endoscopy. At least at index screening, it may be appropriate in FAP patients to include extended duodenoscopy with either a pediatric colonoscope or a push enteroscope. Biopsy specimens of the ampulla are necessary to detect early adenomatous change in light of the frondlike appearance of many normal papillae. Care should be taken to avoid the expected location of the pancreatic orifice (5 o’clock position) to reduce the risk of biopsy-related pancreatitis, and multiple biopsy specimens (at least six) are needed for adequate sampling. Nonetheless, ampullary biopsy carries a small risk of necrotizing pancreatitis and is not mandatory in an asymptomatic patient with an essentially normal-appearing ampulla. For larger lesions, mucosal biopsy alone may not sufficiently exclude invasive malignancy.42 Additional cross-sectional imaging and endoscopic ultrasound (EUS) is often used to evaluate for invasive disease.
A small series of patients undergoing high-resolution endoscopy with chromoendoscopy suggested an improved yield of adenoma detection in periampullary and duodenal polyposis. Dekker and associates43 evaluated 43 patients with FAP who underwent screening endoscopy using high-resolution endoscopes. They found that the additional use of indigo carmine chromoendoscopy increased the detection of adenomas from a median of 16 adenomas per patient to 21 adenomas per patient (P = .02) and enhanced margin detection in 51%. The addition of chromoendoscopy resulted in upgrading of the Spigelman stage (see Table 34.1) in 12% of patients (P = .03). Itoi and colleagues44 found that the use of either indigo carmine or narrow band imaging was superior to standard white light examination in 13 of 14 cases. In this study, visualization was categorized as difficult, fair, or excellent. Narrow band imaging had significantly higher proportion of “excellent” visualization of the tumor margin than indigo carmine chromoendoscopy (P = .012).
Because of the poor sensitivity of endoscopic biopsies in detecting malignant change, we routinely employ EUS to assess for depth of invasion and adjacent biliary or pancreatic involvement. Because we generally avoid diagnostic cholangiopancreatography, we pursue endoscopic retrograde cholangiopancreatography (ERCP) to assess for biliary or pancreatic ductal extension only when endoscopic ampullectomy is being considered during the same session. Although limitations of EUS include compression of the affected tissues and inability to “water-fill” the second portion of the duodenum adequately to assess for depth of invasion consistently, it has shown utility in the TNM (primary tumor, regional nodes, metastases) staging of periampullary malignancy with staging accuracy of 84%.42,45–48
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree