Ultrasonographic findings
Patients witha positive sign (#)
Abnormal aspect of the small intestine
36
Increased peristalsis
32
Abdominal fluid
30
Pericardial effusion
18
In a case–control study of 11 adults with histologically proven CD and 20 healthy subjects (Table 2) Rettenbacher et al. (1999) found that the controls were negative whereas the cases showed: an increase of intraluminal fluid content, the presence of moderate small bowel dilatation, increased peristalsis and moderate bowel wall thickness. Further extra-intestinal signs, such as the mesenteric lymph node enlargement, free abdominal fluid, a dilated superior mesenteric artery or portal vein and hepatic steatosis were also identified with overall frequencies of 52–84 %.
Table 2
US findings in a series of 11 adult patients with histologically proven CD (from Rettenbacher et al. 1999)
Ultrasonographic findings | Patients with a positive sign (#) |
|---|---|
Moderate small bowel dilatation | 8 |
Increased intraluminal fluid content | 11 |
Small bowel wall thickness | 7 |
Increased peristalsis | 8 |
Mesenteric lymph node hypertrophy | 9 |
Free abdominal fluid | 5 |
Dilated superior mesenteric artery or portal vein | 7 |
Hepatic steatosis | 6 |
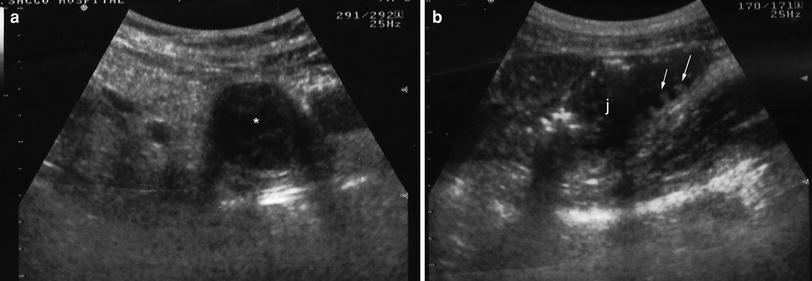
A prospective study on an adult population by Fraquelli et al. (2004) evaluated the diagnostic accuracy of several US signs in predicting CD in a cohort of 162 patients consecutively examined, who presented with chronic diarrhoea or iron-deficiency anaemia or dyspepsia. These conditions are all frequent manifestations of CD. This population had a pretest CD probability of about 10 %, as estimated from a previous series (Hin et al. 1999). All the patients underwent anti-endomysial IgA antibody determination and a duodenal biopsy. Two operators, blind to the clinical, serological and histological findings, evaluated the presence of six US signs: the increased transverse diameter of small bowel loops contained increased fluid (Fig. 1a, b), the increased small bowel wall thickness (Fig. 1c) with hypertrophic valvulae conniventes (Fig. 1d, e), the pattern of peristalsis, the presence of free abdominal fluid within the abdominal cavity (Fig. 2a, b), the presence of enlarged mesenteric lymph nodes (Fig. 3) and the presence of enlarged fasting gallbladder volume (Fig. 4).
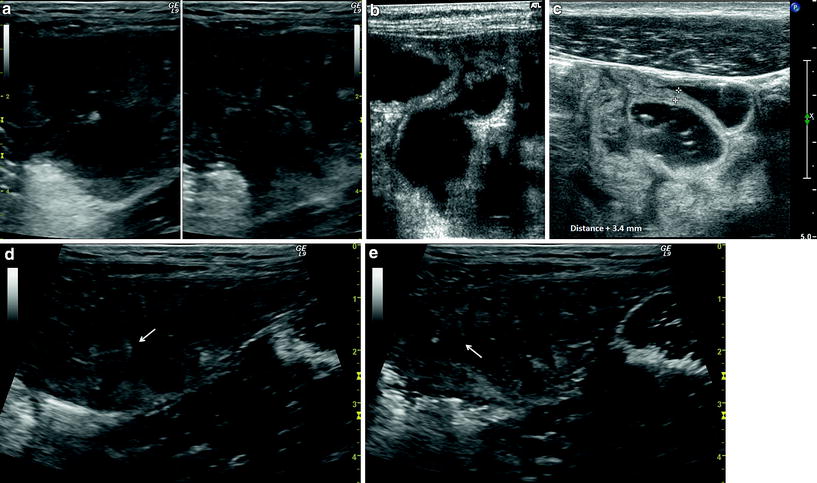
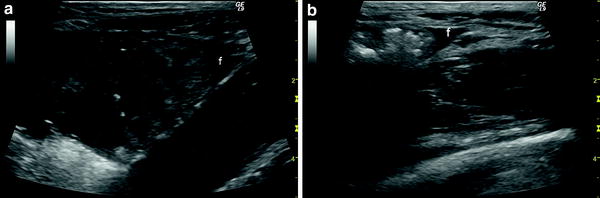
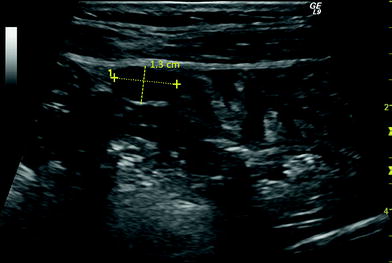

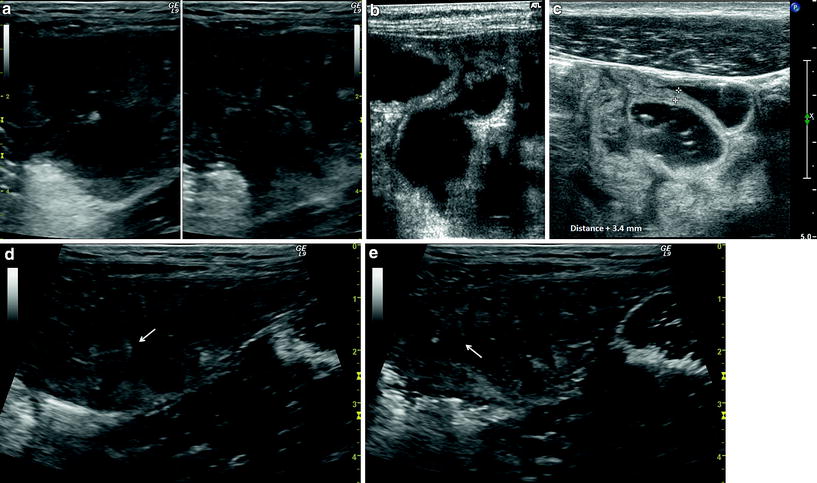
Fig. 1
a, b Dilated small bowel loops with anechoic liquid content in coeliac disease. c US image showing small bowel loops with increased small bowel wall thickness. d, e Dilated small bowel loops with hypertrophic valvulae conniventes (arrows) in coeliac disease
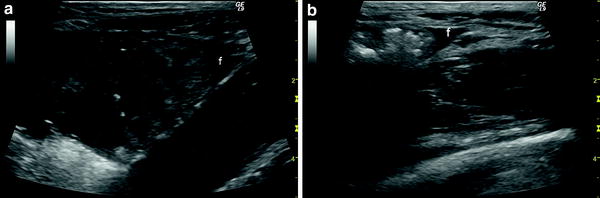
Fig. 2
a, b US images showing a small amount of anechoic free fluid (f) within the abdominal cavity in coeliac disease
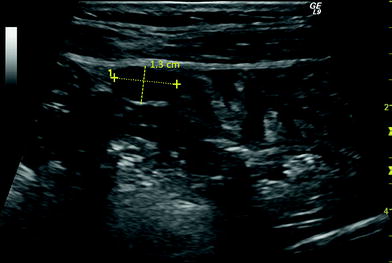
Fig. 3
Enlarged mesenteric lymph node in coeliac disease

Fig. 4
Enlarged gallbladder in coeliac disease
A total of 12 patients (7 %) were diagnosed as having CD on the basis of EMA positivity and histological duodenal findings consistent with Marsh grade III (11 cases) or IV (1 case). Out of the 150 EMA-negative cases, all having normal duodenal histology, 72 (48 %) were eventually diagnosed as having functional disease, and 78 (52 %) as having organic disease, including nine showing ileal involvement (six with Crohn’s disease and three with the final diagnosis of giardiasis and common variable immunodeficiency, primary lymphangiectasia, and ileal carcinoid). Interestingly, the US pattern in the patients with ileal Crohn’s disease, showing a localised and marked bowel wall thickening, was completely different from that observed in CD patients. The details concerning the diagnostic accuracy of the six US signs are shown in Table 3.
Table 3
Sensitivity, specificity, positive and negative likelihood ratio (LR+ and LR−), and positive and negative predictive value (PPV and NPV) of six US signs in predicting CD
US parameters | Sensitivity % | Specificity % | LR+ | LR− | PPV % | NPV % |
|---|---|---|---|---|---|---|
Increased GB volume Increased gallbladder volume (reference value: ≤20 mL) | 73 (46–99) | 96 (92–99) | 17.0 (7.3–41.0) | 0.28 (0.1–0.7) | 57 (31–83) | 98 (95–100) |
Dilated small bowel loops + increased fluid content (reference value: ≤2.5 cm) | 92 (76–100) | 77 (70–84) | 4.0 (2.8–5.5) | 0.10 (0.1–0.7) | 24 (11–36) | 99 (97–100) |
Thickened small bowel wall (reference value: ≤3 mm) | 75 (50–99) | 91 (86–95) | 8.0 (4.4–14.5) | 0.27 (0.1–0.7) | 39 (19–59) | 98 (95–100) |
Increased peristalsis | 83 (62–100) | 87 (82–92) | 6.6 (4.0–10.7) | 0.10 (0.05–0.7) | 34 (17–51) | 98 (96–100) |
Free abdominal fluid | 50 (22–78) | 96 (93–99) | 12.5 (4.7–33) | 0.52 (0.3–0.9) | 50 (22–78) | 96 (92–99) |
Enlarged mesenteric lymph nodes (reference value: ≤5 mm) | 42 (14–69) | 97 (95–99) | 15.6 (6.8–50.6) | 0.59 (0.4–0.9) | 55 (23–88) | 95 (92–99) |
Furthermore, the positive likelihood ratios (LR+) of >10 observed for increased gallbladder volume, free abdominal fluid and enlarged mesenteric lymph nodes allowed for a confirmatory strategy, whereas the negative likelihood ratios (LR−) of 0.1 observed for dilated small bowel loops and increased peristalsis supported an exclusion strategy (Sackett and Haynes 2002).
The k values (i.e. the statistical measure of inter-rate agreement between US sing and duodenal histologic findings) ranged from 0.76 for increased peristalsis to 0.95 for dilated small bowel loops, and were consistent with the good interobserver agreement in evaluating the US signs. It is interesting to note that a strict GFD led to EMA negativity and the complete reversal of the US abnormalities after 1 year.
Overall, increased gallbladder volume, abdominal free fluid and mesenteric lymph node enlargement reliably and accurately predict CD, whereas the lack of intestinal dilatation and increased peristalsis makes it possible to rule out the diagnosis. The specificity of US was 99 % in the presence of all six signs, with an obvious decrease in sensitivity (33 %). Moreover, an LR+ value of 50 allowed for a confirmatory strategy and a PPV of 80 %. Conversely, in the presence of at least one US sign, sensitivity was 92 % with an LR− value of 0.10 and an NPV of 99 %, a diagnostic performance that was comparable to that of dilated small bowel loops.
The above findings support the role of US in predicting CD; however, its role in a diagnostic algorithm should be varied on the basis of the probability of the disease in a given population.
A 2007 retrospective study focused on 250 adult patients with suspected or proved CD: among them 59 had histologically proven CD. The US of the small intestine revealed irregular peristalsis of the small intestine in 79 % cases and intermittent invaginations in 30 %. The thickening, shortening and decrease in number of the jejunum folds (ileum like transformation) at US was observed in 90 % patients. An increase in the number of ileal folds (jejunum like transformation) was evident in 75 % patients. Mesenterial lymphadenopathy was observed in 95 % patients. (Bartusek et al. 2007).
In the case–control study by Castiglione et al. (2007), 50 CD patients and 50 dyspeptic subjects (control group) underwent abdominal US. The presence of fluid-distended small bowel loops with thickened valvulae conniventes and increased peristalsis was considered a US sign of coeliac disease. All clinical, biochemical and all US signs were assessed at the diagnosis and re-evaluated after 1 year of gluten-free diet: signs were present in 66 % of CD patients. Sensitivity, specificity, positive and negative predictive values resulted: 66, 96, 94 and 74 %, respectively. Abnormal US findings were recorded in 82 % of the patients with endoscopical markers of CD, in 87.5 % of the symptomatic patients, and in 61 % of the patients without symptoms. After 1 year of gluten-free diet US was still abnormal in 20 % patients, with no correlation with laboratory tests e/o symptoms.
A very recent study on a paediatric population aimed at assessing the usefulness of abdominal US for the diagnostic work up of those cases suspected of having CD involving negative serum antibodies and difficult cases. A diagnosis of CD with negative serum antibodies was probable in 71 patients who underwent US and duodenal biopsy for histologic examination. Intestinal histology and subsequent clinical and histologic follow-up confirmed the diagnosis in 11 patients and excluded it in 59. Abdominal US showed that the presence of dilated bowel loops and thickened bowel wall had a sensitivity of 83 % and a negative predictive value of 93 % in CD diagnosis. The concomitant presence of the two signs increased the sensitivity to 92 % and the NPV to 98 % (Soresi et al. 2011), once again confirming that the absence of dilated bowel loops is the indicator with the highest probability of excluding the diagnosis of CD.
The combination of small intestine US and an anechoic contrast agent (SICUS) have been assessed in a case–control study which involved 33 patients with histologically proven CD and 30 healthy volunteers matched for sex and age. Loop diameter, Kerckring’s folds number, peristaltic waves, and Doppler resistance index [RI; i.e. (peak systolic velocity—end diastolic velocity)/peak systolic velocity] appeared to be significantly different between CD patients and controls. In addition, liquid content, ileal jejunalization and mesenteric lymphoadenomegaly were only present in CD patients (52, 48 and 96 %, respectively), but in none of the controls. Only the Doppler RI values significantly correlated with the histologic degree of damage (Dell’Aquila et al. 2005).
2.1 Rare Manifestations of Coeliac Disease
Other less common manifestations of CD that can be discovered with abdominal US examination are the presence of mesenteric lymph node cavitation and the presence of transient small bowel intussusceptions (Hec et al. 2012).
The cavitation of mesenteric lymph nodes is a rare complication of CD but its pathogenesis remains to be clarified (Fig. 5). It has been described as being revealed by US or computed tomography in a few cases, and was sometimes associated with hyposplenism (Burrell et al. 1994; Bahlouli et al. 1998; Bardella et al. 1999; Reddy et al. 2002; McBride et al. 2010).