Diagnostic Testing of Disorders of Pelvic Support
Olugbenga A. Adekanmi
Robert M. Freeman
The complex interaction between the integrated pelvic support structures making up the bony pelvis, muscles, and fascia helps to maintain normal positioning and function of the pelvic organs both at rest and during physical activity. Symptoms of female pelvic floor disorders often arise as a result of disruption of the normal interaction between these supporting structures. This chapter examines the current role of diagnostic testing for dysfunction of pelvic floor support.
INTRODUCTION
Management of female pelvic floor disorders usually relies on careful and detailed clinical assessment of the anterior, middle, and posterior compartments as an integrated functional unit. However, diagnostic testing may be necessary in order to assess complex symptoms, to plan surgical intervention, or even to determine the presence of “occult” dysfunction that might give rise to new symptoms following surgical intervention. Investigations available for the assessment of disorders of the pelvic support include imaging techniques for visualization of the supporting structures and their function and urodynamic investigations for assessing function of the “displaced” lower urinary tract.
The imaging techniques currently available for assessment of female pelvic floor support disorders include traditional radiology examinations such as abdominal radiography, colpography, cystography, and proctography. More recent techniques include magnetic resonance imaging (MRI) and ultrasonography. Traditional conventional techniques involving x-ray imaging, although simple and relatively inexpensive, appear to have limited value in the evaluation of female pelvic floor dysfunction because they offer poor visualization of soft tissues and involve exposure of patients to irradiation. The relatively new imaging techniques of MRI and ultrasound offer more detailed visualization of the soft tissues and provide improved knowledge about the dynamic interaction between the pelvic supporting structures. However, their current role should probably be considered as that of a research tool because of a lack of internationally agreed test methodology, image analysis and interpretation, and more importantly a lack of evidence to show that application of the tests can improve clinical outcomes.
Urodynamic investigations can be useful in the evaluation of lower urinary tract symptoms associated with pelvic support defects and might help to determine or exclude the presence of occult lower urinary tract dysfunction (e.g., incontinence) that can become evident following surgical correction of pelvic organ prolapse.
CONVENTIONAL RADIOLOGY
Plain Abdominal and Pelvic X-Ray
Plain x-ray imaging offers good visualization of the bony pelvis and is valuable in the identification and location of suspected radiopaque foreign bodies. It does not show soft tissue abnormalities and is unable to demonstrate the pelvic support anatomy. For that reason plain x-ray imaging has a very limited role in investigating pelvic support disorders.
Lateral Bead Chain Cystourethrography
Cystourethrography was first applied to the investigation of female urinary disorders in 1928. Subsequently, imaging with a metallic bead chain in the urethra to aid lateral visualization of the bladder neck was included. However, it has virtually disappeared from routine clinical practice because of the lack of reproducibility and the lack of validity of the posterior vesicourethral angle as a useful marker of urodynamic stress incontinence (1).
Colpocystourethrography
Colpocystourethrography was introduced as an x-ray contrast imaging technique to outline the vagina (and rectum) in addition to the bladder. It involved the insertion of radiopaque dye into the bladder, urethra, vagina, and rectum. Dynamic imaging was performed with the patient standing, first while contracting the pelvic floor and second during Valsalva. It was used to investigate the dynamics of the pelvic organs during prolapse and also to study female urinary incontinence. It is no longer routinely performed.
Voiding Cystourethrography
Voiding cystourethrography enables visualization of the lower urinary tract during voiding, which can be difficult using other imaging techniques. It can detect diverticula of the bladder and urethra (2), urethral obstruction, vesicoureteric reflux trabeculation of the bladder (often associated with detrusor overactivity) and “occult/potential” stress incontinence associated with cystocele. It remains a useful tool in the evaluation of recurrent urinary incontinence after previous failed surgery, and with prolapse reduction in continent women with pelvic organ prolapse, combined cystometry and cystourethrography (videocystourethrography) can increase the detection rate of occult stress incontinence (3).
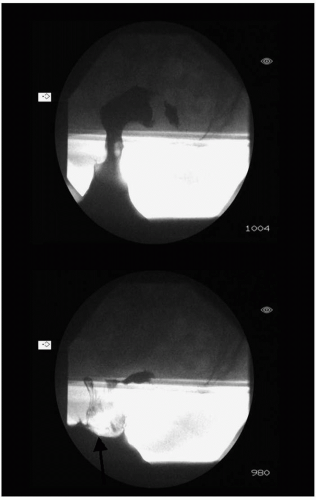
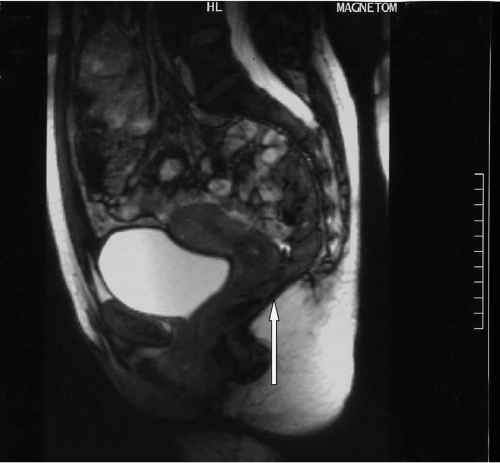
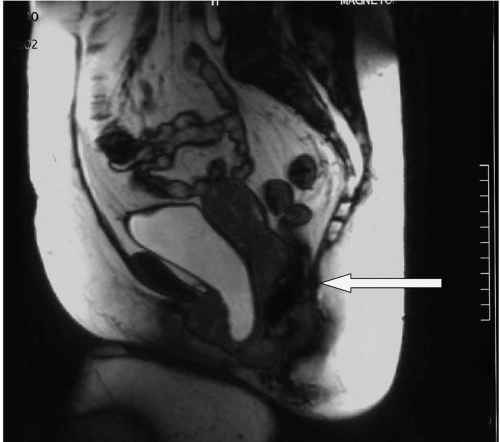
Defecography
Defecography is used to demonstrate the dynamics of rectal evacuation and identify support abnormalities of the posterior vaginal compartment. It involves injection of a thick barium paste into the rectum and subsequent videofluoroscopic observation at various stages of rest, Valsalva, voluntary evacuation, and recovery. The small bowel is opacified with an oral barium meal. Defecography can identify the presence of enteroceles, rectoceles (Fig. 26.1), rectal intussusception, rectal prolapse (Fig. 26.2), and incomplete evacuation. A recent development is cystodefecoperitoneography (CDP), which involves the use of contrast medium in the urinary bladder and intraperitoneally (4,5). It allows for further assessment of peritoneoceles and enteroceles (5,6). Assessment of the anterior vaginal compartment with the simultaneous imaging of the bladder does not correlate well with clinical assessment of anterior vaginal wall descent (7).
MAGNETIC RESONANCE IMAGING (MRI)
The role of MRI in the evaluation of pelvic support anatomy has increased in popularity since its introduction in 1990 by Klutke et al (8). At present the use of MRI should be limited to clinical research because of the need for improved understanding of its role in the management of pelvic organ prolapse, the current lack of standardized techniques, and the relatively high costs. Nevertheless, MRI has been used for grading pelvic organ descent, and it appears to be a valuable tool in the evaluation of anatomic defects associated with prolapse. It has the potential for being the “gold standard” test for pelvic support imaging because it is easily reproducible and provides a permanent visual record of the bony, soft tissue, fascial connections, and musculature of the pelvic support structures.
MRI allows evaluation of tissue states, function, and motion dynamics and has many advantages over traditional imaging techniques, including its excellent tissue contrast, noninvasive nature, and the absence of ionizing radiation. It produces relatively easily recognizable images. MRI works on the principle that every tissue contains hydrogen nuclei that have a constant magnetic spin, and the MRI scanner utilizes an extremely powerful magnet with a field strength of approximately 0.3 to 2.0 Tesla (i.e., the unit of magnetic field strength; in comparison, a refrigerator magnet has a field strength of 0.01 T; the earth’s magnetic field is 0.00003 to 0.00007 T).
Three commonly used imaging sequences help to distinguish tissues from one another. The T1-weighted sequence provides good spatial resolution (detail) and is useful for visualizing anatomy. Fat appears bright and water appears dark. The T2-weighted sequence is sensitive to local edema and is useful for identifying pathology. Fat appears bright but less than on T1-weighted images. Water also appears bright. In proton density images, fat
appears bright and water/simple fluid dark. For all the sequences, cortical bone and air appear black (9).
appears bright and water/simple fluid dark. For all the sequences, cortical bone and air appear black (9).
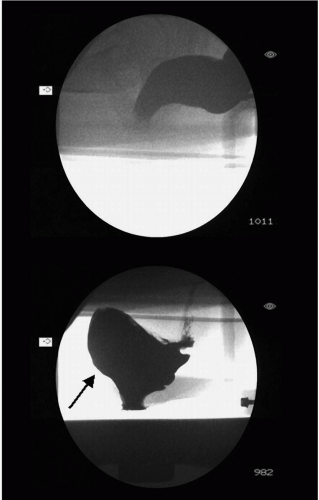 FIGURE 26.1 ● Defecography in a patient with defecatory symptoms but no obvious prolapse on clinical examination. Image below shows an anterior rectocele with incomplete bowel emptying on evacuation. |
Visibility of Vaginal Compartments on MRI
Although sagittal pelvic MRI allows simultaneous visualization of all vaginal compartments, enabling an accurate determination of the relationship of the contents to each other (Figs. 26.3 and 26.4), there has been concern about its ability to adequately visualize the posterior compartment. Healy et al (10) found that there was poor agreement between MRI and evacuation proctography for the measurement of anorectal junction descent and anorectal angle. Also, MRI detected fewer rectoceles, possibly because it was performed in
the supine position, thus excluding the effects of “gravity” and downward pressure. Techniques to improve visualization of the posterior compartment, including filling the rectum with 100 mL aqueous sonographic gel (11) and use of open configuration MRI scanning that allows imaging in the sitting position, have been undertaken to improve assessment of pelvic organ prolapse (12,13).
the supine position, thus excluding the effects of “gravity” and downward pressure. Techniques to improve visualization of the posterior compartment, including filling the rectum with 100 mL aqueous sonographic gel (11) and use of open configuration MRI scanning that allows imaging in the sitting position, have been undertaken to improve assessment of pelvic organ prolapse (12,13).
MR Quantification (Grading) of Pelvic Organ Prolapse
The use of MRI to quantify pelvic descent in all three vaginal compartments was first described by Yang et al (14), who analyzed sagittal images of 26 symptomatic and 16 control women. They evaluated pelvic descent using the pubococcygeal line (PCL) (Fig. 26.5) as the internal reference from
which measurements are made. The PCL was defined as a line extending from the most inferior portion of the symphysis pubis to the tangent of the last coccygeal joint. Normal reference limits were determined and it was established that the bladder base should not descend more than 1 cm below, the cervix or vaginal cuff should remain at least 1 cm above, and the rectum no more than 2.5 cm below the PCL. They also demonstrated that other measurements, such as the thickness of levator ani muscles, length of the urethral, and periurethral muscle ring, can be obtained on MRI (14). The PCL has subsequently been used by other investigators (11,12,15, 16, 17, 18, 19, 20, 21, 22, 23). Hodroff et al (24) found that MRI grading of prolapse differentiated between those without prolapse and those with prolapse of the anterior vaginal wall (i.e., Pelvic Organ Prolapse Quantification [POPQ] grade 0 from grades I and II) but it did not differentiate between the International Continence Society (ICS) POPQ grades of prolapse (i.e., ICS POPQ [25] grades I and II).
which measurements are made. The PCL was defined as a line extending from the most inferior portion of the symphysis pubis to the tangent of the last coccygeal joint. Normal reference limits were determined and it was established that the bladder base should not descend more than 1 cm below, the cervix or vaginal cuff should remain at least 1 cm above, and the rectum no more than 2.5 cm below the PCL. They also demonstrated that other measurements, such as the thickness of levator ani muscles, length of the urethral, and periurethral muscle ring, can be obtained on MRI (14). The PCL has subsequently been used by other investigators (11,12,15, 16, 17, 18, 19, 20, 21, 22, 23). Hodroff et al (24) found that MRI grading of prolapse differentiated between those without prolapse and those with prolapse of the anterior vaginal wall (i.e., Pelvic Organ Prolapse Quantification [POPQ] grade 0 from grades I and II) but it did not differentiate between the International Continence Society (ICS) POPQ grades of prolapse (i.e., ICS POPQ [25] grades I and II).
A slight variation of the PCL referred to as the sacrococcygeal inferior pubic point (SCIPP) line has also been used for grading of pelvic descent on MRI (26). This line extends from the inferior border of the pubic symphysis to the sacrococcygeal joint.
Recently, a new reference line, the midpubic line (MPL) (see Fig. 26.5), was described as a line drawn through the longitudinal axis of the pubic bone, passing through its midequatorial point (27). It corresponds to the level of the hymenal ring, the reference point used in the POPQ system (25).
MRI grading of pelvic organ prolapse using this method was shown to have a good agreement with ICS POPQ clinical staging.
MRI grading of pelvic organ prolapse using this method was shown to have a good agreement with ICS POPQ clinical staging.
MR Imaging of Pelvic Support Anatomy
The role of MRI in the evaluation of female paraurethral and bladder neck anatomy was first demonstrated by Klutke et al (8) in a study involving a female cadaver with no known history of urinary incontinence, and 50 (5 continent, 45 incontinent) patients between the ages of 30 and 73 years. It was seen on MRI that levator muscle fibers support the pelvic organs like a hammock. They found medial extensions from the levator muscles to the bladder neck and proximal urethra, which they referred to as the urethropelvic ligaments. On axial MRI of the lower third of the vagina (vaginal support level III [28]), the anterior vaginal wall conforms to and reflects the well-supported bladder neck and proximal urethral area; the normal H configuration on cross-sections of the vagina is easily visualized on MRI (8) (Fig. 26.6). Based on deviation from the normal anatomical appearances, it is possible to demonstrate paravaginal defects (Fig. 26.7) on MRI at the three vaginal levels (8,28,29). The appearances on MRI of anterior vaginal compartment central endopelvic fascial defects have also been described (30) (Fig. 26.8). However, this still requires validation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree