Chapter 52 Definition and classification of pancreatitis
Overview
Despite four international consensus meetings over 40 years, the issue of definition and classification of pancreatitis (see Chapters 53 to 55) is still under critical revision. The main reason is the difficulty, in contrast to other common inflammatory gastroenterologic diseases, to obtain pancreatic tissue specimens to define the diagnosis better during the inflammatory process. Any classification of pancreatitis must be based on clinical, morphologic, and laboratory features.
The history of the definition and classification of pancreatitis is characterized mainly by the distinction between acute and chronic pancreatitis as stated by Lagerlof in 1942. These two clinical conditions seemed to be two different and separate pathologic processes. In recent years, with the widening of clinical observation and improved accuracy of imaging studies, particularly magnetic resonance imaging (MRI) of the bile ducts and duct of Wirsung, the classic distinction between acute and chronic pancreatitis is under critical revision.
History of the Definition and Classification of Pancreatitis
The history of the definition and classification of pancreatitis shows the progressive awareness of experts that acute and chronic inflammation should be defined by different pathologic, clinical, and etiogenetic perspectives (Table 52.1). The different points of view correlate with each other and together provide the best comprehension of the inflammatory process. Consequently, the clinical management of an individual patient can be improved only by considering all the features of pancreatitis.
Table 52.1 A Synopsis of Pancreatitis Classification from 1946 to 2011
| Classification | Definition |
|---|---|
| Marseille, 1965 | Description of morphologic characteristics and etiologic factors of the disease; no categorization according to disease severity, no imaging findings |
| Cambridge, 1984 | Classification of disease severity based on pancreatic imaging criteria (US, CT, ERCP); discussion of etiologic factors and pancreatic function |
| Revised Marseille, 1985 | Description and further subclassification of morphologic changes; definition of “obstructive chronic pancreatitis” as a distinct form; no discussion of the correlation between anatomic and functional changes, no inclusion of pancreatic imaging findings |
| Marseille-Rome, 1988 | Further description of “chronic calcifying” and “chronic inflammatory” pancreatitis as distinct forms; description of etiologic factors; no further elaboration of clinical, functional, or imaging criteria |
| Atlanta, 1992 | Description of clinical and morphologic features of pancreatitis; dynamic classification system able to characterize the individual patient and predict severity |
| Zurich, 1997 | Description of clinical presentation and classification of the disease in “definite” and “probable” chronic pancreatitis according to imaging findings, functional testing, and histologic examination |
| Japan Pancreas Society, 1997 | Description of clinical presentation and classification of the disease in “definite” and “probable” chronic pancreatitis according to imaging findings, functional testing, and histologic examination; definition of radiologic and laboratory features in patients lacking etiologic and pathogenetic features |
| TIGAR-O, 2001 | Detailed categorization of etiologic risk factors and correlation between acute and chronic pancreatitis |
| ABC, 2002 | Disease grading according to clinical criteria; limited separation of different disease severities; not all clinical presentations categorized |
| Manchester, 2006 | Disease grading according to clinical criteria; limited separation of different disease severities |
| M-ANNHEIM, 2007 | Categorization of patients according to etiology, clinical stage, and severity of disease; severity of pancreatic inflammation assessed using a specific scoring system |
US, ultrasound; CT, computed tomography; ERCP, endoscopic retrograde cholangiopancreatography
The first effort to classify and define pancreatitis by a worldwide group of experts led to the Marseille Consensus Meeting in 1963 (Sarles, 1965). The panel of pancreatologists agreed that acute and chronic pancreatitis were different diseases mainly because of different morphologic patterns. Relapsing pancreatitis was characterized by the presence of multiple episodes in a morphologic pattern of acute or chronic processes. The distinctive features of the two diseases were the pathologic benign course of acute inflammation, with biologic restitution in the acute condition, and the progressively worsening parenchymal lesions in the chronic condition (Table 52.2). The present histology-based classification does not provide clinically useful definitions, making it impossible to compare different experiences. From the clinical point of view, acute and chronic pancreatitis show a similar pattern, at least in the earlier phases.
Table 52.2 Marseille Classification of Pancreatitis
| Feature | Acute Pancreatitis/Acute Relapsing Pancreatitis | Chronic Relapsing Pancreatitis/Chronic Pancreatitis |
|---|---|---|
| Clinical characteristics | Single/multiple episodes | Multiple episodes/no acute exacerbations is common |
| Morphologic characteristics | Not defined | Irregular sclerosis with destruction and focal segmental or diffuse loss of parenchyma with varying dilation of ductal system; strictures, intracanalicular stones (calcifications), cysts, pseudocysts; islets of Langerhans are involved much later in the course of the disease; morphologic picture is similar, independent of cause |
| Course | Clinical and biologic restitution if the cause is removed | Functional and morphologic lesions persist or progress after the cause is removed |
Modified from Sarles H, 1965: Proposal adopted unanimously by the participants of the symposium of acute pancreatitis in Marseille, 1963. Bibl Gastroenterol 7:7-8.
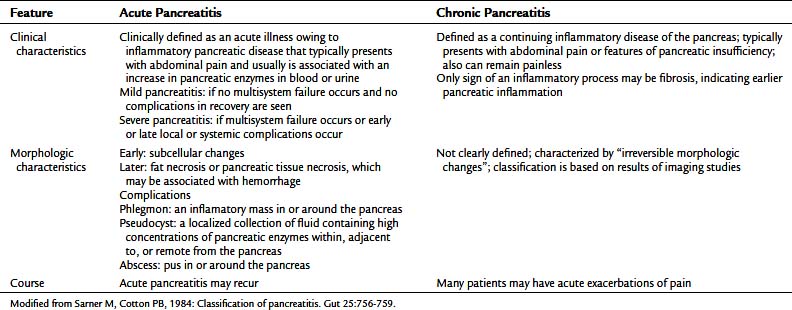
Progress in the comprehension of pancreatitis and its classification resulted from the Cambridge meeting (Sarner & Cotton, 1984). The distinction between acute and chronic pancreatitis was confirmed, and the term relapsing pancreatitis was avoided in the chosen terminology. The importance of the clinical impact of different severity systemic responses was emphasized (Table 52.3), and the importance of definition of a morphologic characterization of the inflammatory process was recognized, particularly for the acute pancreatitis group. The Cambridge group pointed out the relevant problem of etiology, and the role of imaging in chronic pancreatitis was addressed.
Endoscopic retrograde cholangiopancreatography (ERCP) classification (Table 52.4) is still in use in some centers. Several studies in the literature showed that ERCP findings are not pathognomonic of chronic pancreatitis but could coexist with many clinical conditions. In particular, cholelithiasis and its complications lead to demonstrable alterations in the morphology of the duct of Wirsung, as stated in the Cambridge classification (Buchler et al, 1987; Misra et al, 1990), and these morphologic changes could persist for many months. In biliary cirrhosis, Sjögren syndrome, and sclerosing cholangitis, pancreatic duct changes are commonly observed at ERCP (Bastid et al, 1990; Epstein et al, 1982; Lindstrom et al, 1991). For all these reasons, the ERCP morphology of the duct of Wirsung is not mandatory to diagnose chronic disease. In addition, increasing use of MRI of the bile ducts and duct of Wirsung provides excellent morphologic imaging of the main and side branch ducts.
Table 52.4 Grading of Chronic Pancreatitis by Endoscopic Retrograde Cholangiopancreatography
| Normal | |
| Equivocal | |
| Mild | |
| Moderate |