Cystou reth roscopy
Geoffrey W. Cundiff
Alfred E. Bent
Cystourethroscopy provides a minimally invasive method of visually evaluating the lower urinary tract. It has broad applications in general gynecology and female pelvic surgery (1). The ability to recognize normal and pathologic findings is essential for assessment and surgical correction of female pelvic disorders.
HISTORICAL PERSPECTIVE
Although many credit Kelly with developing the female cystoscope, endoscopy of the female bladder preceded his report by half a century. Bozzini (2) described an endoscopic technique for evaluating the female bladder in the early 19th century. His invention consisted of a stand that supported different-sized hollow funnels, a candle for illumination, and a reflector to direct the light into the funnel when it was placed into the urethra. Desmormeaux (3) introduced a more practical endoscope in 1853 that used different-sized angulated tubes. The tubes increased the surface area of the bladder that could be inspected, and use of an alcohol lamp improved illumination. By 1877, Grünfeld’s (4) modification of the endoscope still used a hollow tube but added an obliquely placed glass lens at the vesical end. His endoscope was vastly improved by the adaptation of an electric light source reflected by mirrors. Nitze (5) developed a compound lens system that increased the field of vision and used an incandescent light source to provide illumination.
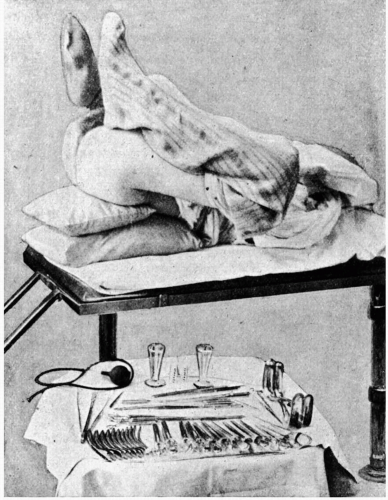
Kelly’s contribution was in overcoming the deficiencies of both Grünfeld’s and Nitze’s instruments and techniques. The Kelly cystoscope was a hollow tube, without glass, that used an obturator for placement (6). The knee-chest position allowed air to distend the bladder. A head mirror was used to reflect an electric light into the bladder for illumination (Fig. 7.1). The technique was simple yet provided an excellent view.
Modern endoscopy started with the development of the Hopkins fiberoptic telescope in 1954 (7). The use of glass fibers in place of an air chamber dramatically improved light transmission and resolution and also provided a wider viewing angle. The viewing angle could also be changed, which improved the extent of visualization and facilitated more invasive procedures. Later modifications of the Hopkins system incorporated a series of glass rods with optically finished ends separated by intervening spaces.
The improved view of the bladder provided by the Hopkins cystoscope compromised the view of the urethra. An angled telescope is not effective for evaluating the urethral mucosa because most cystoscopic sheaths have a terminal fenestra for use with a catheter deflector mechanism. This design allows the irrigant to escape during its distal location in the urethra. Robertson (8) addressed the compromised view of the urethra by applying fiberoptic technology to a shorter straight-on telescope, later known as the urethroscope.
The most recent development in cystoscopy is the flexible cystoscope. The flexible fiberoptic lens system permits an instrument that bends, thereby increasing the field of view. Comparisons continue regarding resolution and comfort between rigid and flexible instruments (9,10). However, the female urethra is so short that a rigid 17 French sheath with a blunted fenestra can be passed with minimal discomfort, and flexible cystoscopy in the female patient has fewer benefits than in the male patient.
EQUIPMENT
Urethroscopy
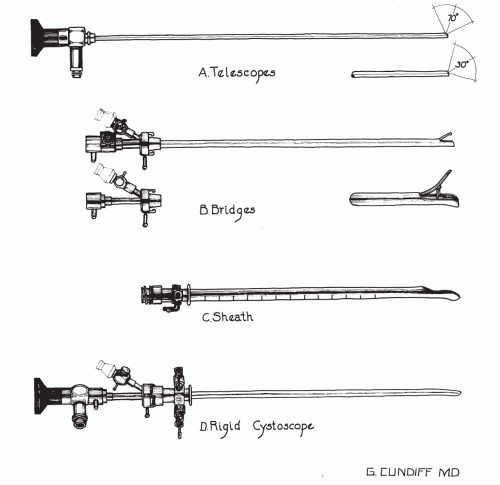
The urethroscope is composed of a telescope and sheath. The telescope has a 0-degree (straight-ahead) viewing angle, which provides a circumferential
view of the urethral lumen as distending medium opens the urethra. The sheath has a port for infusion of medium as well as a valve to initiate flow of medium or allow bladder emptying. Sheath sizes are 15 and 24 French. Fluid flow is minimal with the 15 French sheath, and thus there is minimal urethral distention during its passage. Although the view is minimally compromised using this sheath size, the larger sheath is better for viewing urethral diverticula and fistula. The instrument is also useful for vaginoscopy (Fig. 7.2).
view of the urethral lumen as distending medium opens the urethra. The sheath has a port for infusion of medium as well as a valve to initiate flow of medium or allow bladder emptying. Sheath sizes are 15 and 24 French. Fluid flow is minimal with the 15 French sheath, and thus there is minimal urethral distention during its passage. Although the view is minimally compromised using this sheath size, the larger sheath is better for viewing urethral diverticula and fistula. The instrument is also useful for vaginoscopy (Fig. 7.2).
Rigid Cystoscopy
The rigid cystoscope is composed of a telescope, bridge, and sheath (Fig. 7.3). Each component serves a different function and is available with various options to facilitate this role. The telescope transmits light to the bladder cavity and an image to the viewer. Several viewing angles are available, including 0- (straight), 12- (minimal angle for periurethral bulking), 25- or 30- (forward-oblique), 70- (lateral), and 120-degree (retro view) angles. The angled telescopes have a field marker
that assists the viewer with orientation. It is visible as a blackened notch at the outside of the visual field and opposite the angle of deflection. It points in the same direction as the light post.
that assists the viewer with orientation. It is visible as a blackened notch at the outside of the visual field and opposite the angle of deflection. It points in the same direction as the light post.
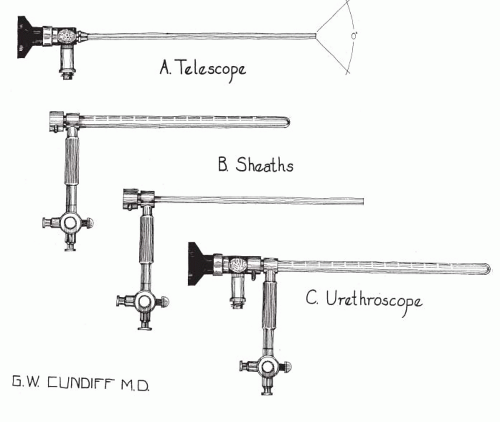 FIGURE 7.2 ● Components of a rigid urethroscope. (A) Telescope, 0-degree. (B) Sheaths, 15 and 24 French. (C) Assembled urethroscope. |
The 30-degree lens provides the best view of the bladder base and posterior wall, whereas the 70-degree lens permits inspection of the anterolateral walls. The retro view of the 120-degree lens is not usually necessary for cystoscopy of the female bladder but can be useful for evaluating the urethral opening into the bladder. A 70-degree telescope is perhaps the best general-use cystoscope for viewing the bladder and is essential in the presence of fixation of the bladder neck (urethrovesical junction [UVJ]) and when performing operative cystoscopy at the time of surgery.
The cystoscope sheath provides a vehicle for introducing the telescope and distending medium into the bladder. It is available in various calibers, from 15 to 28 French. The telescope partly fills the lumen of the sheath, leaving room for an irrigation/working channel. The smallest-diameter sheath is useful for diagnostic purposes, whereas larger-caliber sheaths allow instruments to be placed in the working channel. The proximal end of the sheath has two irrigating ports: one for introduction of the distending medium and the other for removal. The distal end of the cystoscope sheath is fenestrated to permit the use of instrumentation in the angled field of view. It is also beveled, opposite the fenestrae, to increase comfort on introduction into the urethra. Larger-diameter sheaths may require an obturator for placement. Most diagnostic work is performed with the 17 French sheath, especially in the awake patient. The sheath size for operative applications depends on the type of instrumentation.
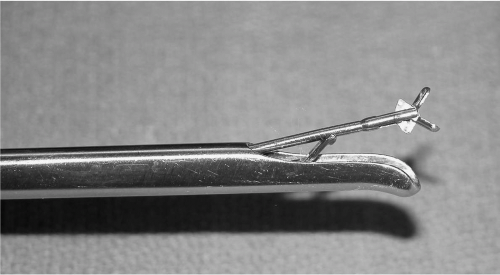
The bridge serves as the connector between the telescope and sheath and forms a watertight seal with both. It may have one or two ports for introduction of instruments into the working channel. The Albarrán bridge is a variation of the bridge that has a deflector mechanism at the end of an inner sheath (Fig. 7.4). When placed in the cystoscopic sheath, the deflector mechanism is located at the distal end of the inner sheath within the fenestra of the outer sheath. At this location, the elevation of the deflector mechanism assists the manipulation of instruments within the field of view.
Flexible Cystoscopy
The flexible cystoscope combines the optical systems and irrigation/working channel in a single unit. The optical system consists of a single imagebearing fiberoptic bundle and two light-bearing fiberoptic bundles. The fibers of these bundles are coated parallel coherent optical fibers that transmit light even when bent. This permits incorporation of a distal-tip deflecting mechanism that will deflect the tip 290 degrees in a single plane. A lever at the eyepiece controls the deflection. The optical fibers are fitted to a lens system that magnifies and focuses the image. A focusing knob is located just distal to the eyepiece. The irrigation/working port enters the instrument at the eyepiece opposite the deflecting mechanism. The coated tip is 15 to 18 French in diameter and 6 to 7 cm in length, with the working unit constituting half the length. The image may appear somewhat granular, but technology
is rapidly closing the gap with the image produced by rigid instrumentation. The flow rate of the working channel is slower than that of rigid instruments, and this may be further curtailed by passage of instruments down the channel. Use of the instrument channel may also limit some of the movement at the tip of the deflector mechanism. Flexible cystoscopes are more comfortable, especially for male patients. As mentioned previously, the short length of the female urethra and ease of passing the rigid cystoscope may offset perceived advantages of flexible instrumentation in the female patient.
is rapidly closing the gap with the image produced by rigid instrumentation. The flow rate of the working channel is slower than that of rigid instruments, and this may be further curtailed by passage of instruments down the channel. Use of the instrument channel may also limit some of the movement at the tip of the deflector mechanism. Flexible cystoscopes are more comfortable, especially for male patients. As mentioned previously, the short length of the female urethra and ease of passing the rigid cystoscope may offset perceived advantages of flexible instrumentation in the female patient.
Light Sources and Video Monitors
A high-intensity (xenon) light source is recommended for use in video monitoring and photography. The light cable must be checked periodically for transmission properties. Video monitoring eliminates awkward positioning of the operator and improves teaching abilities. It may also help to distract the patient, while allowing her to see important findings.
Distending Medium
Water or saline is generally used as a distending medium. The fluid is instilled by gravity through a standard intravenous infusion set, with the bag height about 100 cm above the patient’s symphysis to provide adequate flow. Pressurized flow is not required.
Instrumentation
A wide range of instrumentation is available for use through the cystoscope sheath. Those most commonly used in female patients are grasping forceps with either rat-tooth or alligator jaws. They are available in flexible or rigid styles and come in varying diameters (1). A monopolar ball
electrode is useful for electrocautery during operative cystoscopy. With the improvement in imaging and photography, biopsy of an obvious tumor may not be necessary, and the picture can be passed along to a consulting urologist for biopsy and transurethral resection of the abnormality.
electrode is useful for electrocautery during operative cystoscopy. With the improvement in imaging and photography, biopsy of an obvious tumor may not be necessary, and the picture can be passed along to a consulting urologist for biopsy and transurethral resection of the abnormality.
CYSTOURETHROSCOPY TECHNIQUES: DIAGNOSIS
Diagnostic cystourethroscopy in women is easily performed as an office procedure and is well tolerated without anesthesia in most cases. Lignocaine gel is useful in the female patient who has apprehension regarding pain (11). Most indications for endoscopy warrant evaluation of both the bladder and urethra (Table 12.1).
Urethroscopy
The urethroscope is placed into the urethra with the fluid infusion flowing in order to distend the urethra and facilitate both the view and the passage of the instrument to the bladder. The 24 French sheath allows optimal visualization, although it may be too large in 10% to 20% of patients. Comfort is essential, and the 15 French sheath should be used in these latter patients. The view is not as good with the smaller sheath as with the larger sheath, but it is adequate. The urethra could be dilated to allow passage of the larger sheath, and in this case topical anesthesia should be used for patient comfort. Topical anesthetic or dilation irritates the urethral mucosa, giving a false impression of inflammation, which should be considered in the final interpretation.
The urethral mucosa is viewed as the instrument is passed slowly to the bladder neck and into the bladder. This causes a small amount of burningtype discomfort. The trigone and ureters may be observed by angling the telescope toward the bladder base and, in some cases, by elevating the trigone with a vaginal finger. The UVJ is observed during the following commands: “hold your urine,” “squeeze your rectum,” “strain down like having a bowel movement,” and “cough.” The hold and squeeze commands are performed with the urethroscope withdrawn enough to allow the UVJ to close two thirds of the way. Movement can then be observed as the UVJ closes during the maneuver. The strain and cough commands are performed with the urethroscope withdrawn enough to allow the UVJ to close two thirds of the way. In this manner, opening of the UVJ can be observed. After modest bladder filling, the vaginal finger compresses and massages the urethra over the end of the urethroscope as the instrument is withdrawn. This allows observation for urethral glands, exudate, fistula, and diverticular openings. The patient has somewhat more discomfort during digital compression of the urethra and should be forewarned concerning this 5 to 10 seconds of discomfort.
Cystoscopy
Cystoscopy is generally performed using a 70-degree telescope with 17 French sheath and with some topical anesthetic on the sheath to facilitate movement in and out of the urethra. The cystoscope is placed into the urethral meatus with the bevel directed posteriorly and is advanced directly into the bladder, aiming at the patient’s umbilicus. An obturator is not necessary with a small sheath such as 17 French, but the fluid flow during insertion facilitates passage. A volume of 250 mL or greater is desirable for bladder inspection unless the patient has discomfort before this volume, and a slow trickle is maintained if needed for optimum view. The air bubble is identified at the bladder dome, and this serves as a landmark for the rest of the examination. The examination begins at the bladder dome, making full sweeps with the instrument at each hour of an imaginary clock, going from 12 to 4 o’clock, then 11 to 8 o’clock, and then observing the posterior bladder wall between 5 to 7 o’clock. Orientation is maintained by placing the field marker directly opposite the area of the bladder to be inspected. The bladder base may require digital vaginal elevation for complete assessment. The bladder volume can be assessed at the end of the inspection by filling the bladder to patient fullness and then measuring the amount of fluid by emptying the bladder through the sheath, or by measuring the volume voided by the patient after the procedure.
Antimicrobial Prophylaxis
A concern after cystourethroscopy is the prevention of infection, which may occur in up to 5% of cases. A number of these patients may have infection at the time of the examination, even with a recent negative urine culture, but it is best to avoid instrumentation in the presence of a known infection. Prophylaxis is practiced by many, but recent reports cite no difference in infection rates between patients treated with placebo and nitrofurantoin (12,13). If prophylaxis is used, only a 1- or 2-day course is suggested, and a urinary analgesic (e.g., phenazopyridine) may also be administered for one or two doses at 3-hour intervals. Patients may experience dysuria, urgency, frequency, and hematuria for several hours after the examination, but most have minimal postprocedure discomfort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree