Fig. 44.1
Cryoprobe placement for whole-gland treatment (Courtesy of Galil Medical, Inc, USA with permission)
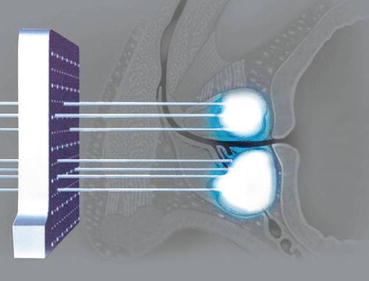
Fig. 44.2
Cryoprobe template insertion (Courtesy of Galil Medical, Inc, USA with permission)
Argon gas is used to cause the rapid freezing at the cryoprobe tip, based on the Joule-Thomson effect: when high pressure argon flows through the cryoprobe, it generates at the tip a very cold temperature, resulting in ice ball formation which damages the tissue. All the cryoprobes are inserted under ultrasound guidance. The number of cryoprobes used will depend on the target prostatic volume. Thermal sensor needles are also inserted into the prostate and the Denonvilliers’ fascia for the temperature monitoring. A warming catheter is placed in the urethra for its protection and also to prevent the freezing of sphincteric muscle. Thermal sensor needles and ultrasound allow a real-time monitoring and a good control of freezing during the procedure. The objective is to achieve a temperature of the target zone to −40 °C or lower while minimizing effects of freezing temperature on rectum and external sphincter which helps in avoiding collateral damage that can result in rectal and urinary symptoms. Once the targeted area is frozen for 10 min, the thawing is employed. This is called the freeze-thaw process. Two freeze-thaw cycles appear to achieve the best tissue ablation [4].
The exact position of the needle placement is verified using ultrasound during the procedure. To achieve a proper placement following precautions are observed.
Cryoprobes should not be placed farther than 1.8 cm apart, they should not be placed farther than 1.0 cm from the margin of the prostate and the distance between the urethra and any cryoprobe should not be less than 0.8 cm [5]. At the end of the procedure, cryoprobes, thermal sensor needles and warming catheter are removed. A urinary catheter is inserted and left in place for 2 or 3 days.
Assessment After Cryotherapy
The response to the treatment is assessed by serial serum prostate specific antigen (PSA) estimations as done after radical prostatectomy (RP) or radiation therapy (RT) (PSA). PSA levels are checked at 3 monthly intervals for the first year and thereafter once every 6 months [2]. After cryotherapy, PSA is still detectable because of the preservation of peri-uretral tissue, which could potentially produce residual PSA. The acceptable PSA levels following treatment are not well defined. However, getting the PSA nadir level within 3 months should provide early evidence of the treatment efficacy. We should consider that PSA nadir ≤0.5 ng/ml should be achieved to expect an increased chance of a stable PSA and negative control biopsy [6]. At the opposite, high PSA value should be associated with a high risk of residual disease [7].
Treatment failure should be determined by using the PSA-based definition of biochemical failure (BCF) and any positive biopsy. Various definitions of BCF are currently used in the literature including the American Society for Therapeutic Radiology and Oncology (ASTRO) definition (three consecutive rising PSA levels) and the Phoenix definition (PSA nadir plus 2). Then, in order to get a better evaluation of treatment results, control biopsies could be recommended between 6 months and 1 year after the treatment [8].
In the beginning, high morbidity rates were reported after cryotherapy. Patients were most concerned about the risks of incontinence and impotence. With improvements of technology, complication rates have fallen but a good evaluation remains mandatory as some of the complications can still be encountered: short term complications include urinary retention, penile or scrotal swelling, penile paraesthesia, sepsis while long term complications include urinary incontinence, fistula, urethral stricture, sloughing, perineal pain and erectile dysfunction [9].
Primary Cryotherapy
Primary cryotherapy represents a viable option for whole-gland treatment in patients with pathological evidence of localized PCa, who do not wish to undergo a RP or RT. Moreover, cryotherapy represents a valuable option in older population and patients with comorbidities.
Patient Selection
Suitable candidates for primary cryotherapy are men with clinically confined PCa (stage T1c or T2), with any Gleason grade, without metastatic disease (N0M0), and with a greater than 10-year life expectancy. Theoretically, cryotherapy can be considered for low, intermediate and high risk PCa. However, it is important to note that high risk patients may require multimodal therapy and also the role of cryotherapy for clinical T3 disease remains to be determined [2].
Other features like gland volume, prior transurethral resection of the prostate (TURP), number of positive cores, baseline PSA, and the risk of lymph node involvement are important to consider when selecting patients. In term of gland size, it may be difficult to achieve a uniformly cold temperature in a prostate larger than 50 cm3. A short hormonal deprivation treatment could be used to downsize gland volume. A prior TURP is a relative contraindication for cryotherapy, due to the increasing risk of tissue sloughing. Larger number of positive cores and higher PSA (>20 ng/ml) represent a risk of lymph node involvement and therefore cryotherapy may not offer optimal local control [1] (Table 44.1).
Table 44.1
Indications to whole-gland primary cryotherapy
Indications to cryotherapy |
|---|
cT1c- cT2 |
PSA < 20 ng/ml |
Gleason score ≤ 7 |
Gland size ≤ 50 cm3 |
To summarize, optimal candidates for primary cryotherapy generally include those with lower stage, lower-volume disease with PSA levels ≤10 ng/ml.
Treatment Outcomes
Oncological Outcomes
Long-term data after primary cryotherapy are now available. Several studies have been published on follow-up data ranging in duration from 5 to 10 years. Cohen et al. [10] reported a 10-year biochemical disease-free survival rate of 80.56, 74.16, and 45.54 % for low, intermediate, and high-risk groups respectively (D’Amico criteria). The 10-year negative biopsy rate was 76.96 %. Five-year data from the Cryo-OnLine Database (COLD) Registry [11] demonstrated a biochemical free disease survival at 84.7, 73.4 and 75.3 % for % for the low, intermediate and high risk groups respectively, using the ASTRO definition and at 91.1, 78.5 and 62.2 % using the Phoenix definition. In this study, only 28.5 % of the patients underwent control biopsies. Positive biopsy rate was 38 % in the group of patients with suspicion of failure treatment due to abnormal or increasing PSA, and 14.5 % for patients who underwent biopsy without any cause. However, negative post-treatment biopsy will not be a proof of cancer eradication and a long term follow-up is necessary. Nevertheless, when comparing results with those of other non-extirpative technique (radiotherapy or brachytherapy), primary cryotherapy seems to offer equivalent outcomes in terms of efficacy [12, 13].
Complications
Clavien-Dindo’ low grade (grade I) perioperative complications like urinary retention, penile or scrotal swelling and penile paresthesia can be seen in patients treated with cryotherapy [8]. These events can be easily managed with appropriate medical treatment. More serious complications such as perioperative sepsis are not frequent and they obviously require a more aggressive intervention. Below we will focus on the long-term adverse events of the procedure.
Recto-urtehral Fistula
Even though this complication is rarely reported after primary cryotherapy due to improved technique improvements, this is probably the most feared. The current risk of recto-urethral fistula ranges between 0 and 0.5 %, which appears similar to those following radical prostatectomy and radiation therapy [7].
Urinary Incontinence
Urinary Incontinence (UI) is a potential complication after cryotherapy. Use of a urethral warmer catheter should prevent such risk, but its possibility still exists. The causes are usually due to damage to the striated sphincter and detrusor instability [2]. The incidence of severe urinary incontinence reported in the range of 1–7.5 % [14].
Erectile Dysfunction
Erectile Dysfunction (ED) occurs frequently after primary cryotherapy primarily due to the freezing of neurovascular bundles. The rate of ED ranges from 49 to 93 % at 1 year [1]. The mechanism is significantly different from the damage that occurs during surgery. As ED is caused by freezing of the neurovascular bundles, the nerves themselves remain intact during the treatment; so for this reason, a potential recovery is a possibility. In order to achieve a better penile rehabilitation, regular use of a vacuum erection device is recommended [5]. Nevertheless, because there is a high risk of post-treatment ED, whole-gland primary cryotherapy is not considered in patients who wish to preserve their sexual function.
It is important to note that these outcomes are not necessarily a reflection of the true efficacy of cryotherapy as currently practiced because some of the reported data have been collected from different generation systems. We could now expect decreasing rate of complications using modern cryotherapy.
Salvage Cryotherapy
Salvage cryosurgery can be considered as a treatment option with a curative intent in men who have failed radiation therapy. Salvage therapy is generally indicated for patients with rising PSA, positive prostatic biopsies and no metastatic disease. A pretreatment nomogram based on serum PSA at diagnosis, biopsy Gleason grade and initial clinical stage was developed and might allow the selection of ideal candidates for salvage cryotherapy [15]. Williams et al. [16] recently reported that salvage cryotherapy led to an acceptable 10-year disease free survival with pre-salvage PSA and Gleason score as the best predictors of disease recurrence. A PSA nadir >1 ng/dl following cryotherapy was verified as a poor prognosis. Furthermore, Cheetham et al. [12] presented their long-term results of primary and salvage prostate cryotherapy and their series showed an 87 % overall 10-year prostate-cancer-specific survival, despite early cryotherapy technology and the majority of patients being D’Amico high risk.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







