Chapter 45 Complications of Laparoscopic and Hysteroscopic Surgery
INTRODUCTION
Unfortunately, many laparoscopic advances were developed by trial and error accompanied by significant morbidity and mortality.1 The application of electrosurgery, automated stapling devices, patient positioning, and trocar use produced unique mechanisms for surgical injury, many of which were not predicted. When can new technologies and procedures be considered safe? How many laparoscopic procedures should be performed before a surgeon is deemed proficient? A recent study of the learning curve associated with laparoscopically assisted vaginal hysterectomies (LAVH) suggests that a gynecologist must perform more than 30 cases before morbidity rates are significantly reduced.1
LAPAROSCOPY
Nerve Injury
Categories of Nerve Injuries
Fortunately, most neurologic injuries associated with patient positioning during laparoscopic surgery do not result in nerve separation and resolve spontaneously with time.2 Those associated with radical surgical dissection may be more likely to be serious and permanent.
Specific Nerve Injuries
Femoral Nerve
The femoral nerve is the largest nerve of the lumbosacral plexus and is derived from the posterior divisions of the L2, L3, and L4 nerve roots (Fig. 45-1). It pierces the psoas muscle and runs inferolaterally within the muscle to emerge between the iliacus and psoas muscles. It then courses under the inguinal ligament to enter the femoral sheath lateral to the femoral artery.
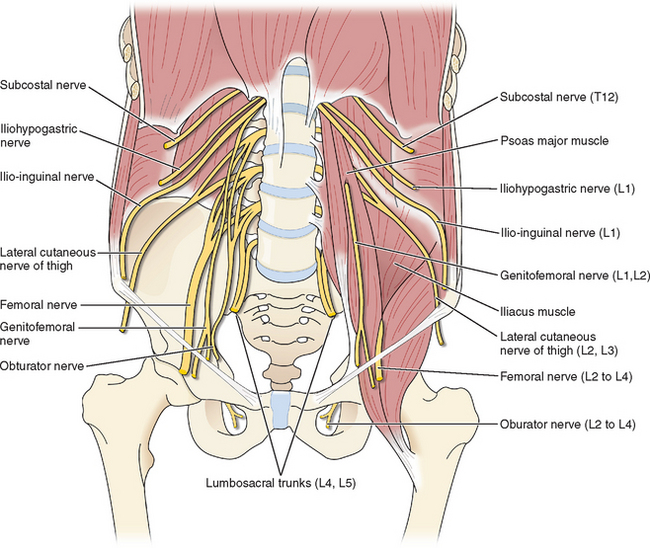
Figure 45-1 Schematic representation of nerves that can be injured during laparoscopy.
(Reproduced from Drake R, Vogl W, Mitchell AWM: Gray’s Anatomy for Students. Philadelphia, Elsevier, 2005.)
Femoral neuropathy during laparoscopy usually results from excessive hip flexion or abduction or from long operating times.2 Patients undergoing vaginal or laparoscopic surgery should be placed in a lithotomy position such that the thigh is flexed no greater than 90 degrees and abducted no greater than 45 degrees. If positioning is changed intraoperatively, these relationships should be maintained.
Obturator Nerve
The obturator nerve arises from the anterior nerve roots of L2, L3, and L4 (see Fig. 45-1). It descends through the psoas muscle, emerging medially at the pelvic brim, and passes through the obturator foramen into the thigh. Its main function is to allow thigh adduction; it supplies motor function to the gracilis, obturator, adductor longus, brevis, and magnus muscles.
Obturator neuropathy can also occur as a result of excessive hip flexion.3 The mechanism whereby excessive hip flexion can cause obturator nerve injury is anatomic. As the obturator nerve leaves the obturator foramen, it lies directly against bone and can become acutely angulated and deformed if the hips are excessively flexed, particularly during prolonged surgery. Injury to the obturator nerve usually manifests as weakness in the hip adductors and sensory loss in the upper medial thigh.
Nerves of the Anterior Abdominal Wall and Inguinal Region: Ilioinguinal, Iliohypogastric, and Genitofemoral
The ilioinguinal, iliohypogastric, and genitofemoral nerves have an overlapping sensory distribution in terms of their cutaneous manifestations, often making it difficult to distinguish between them. The course of these nerves is quite variable. The iliohypogastric and ilioinguinal nerves originate from the T12 and L1 nerve roots of the lumbosacral plexus (see Fig. 45-1). They cross over the quadratus lumborum muscles and pierce the transversus abdominis muscle in parallel at about the level of the anterior superior iliac spine.4 The genitofemoral nerve originates from the L1 and L2 nerve roots to pass anterior to the psoas muscles (see Fig. 45-1). The iliohypogastric nerve supplies sensation to the suprapubic region, and the ilioinguinal nerve supplies sensation to the inguinal canal. The genitofemoral nerve provides sensory innervation to the labial skin (genital branch) and the superior thigh (femoral branch).
The most common injury to these nerves is due to abdominal and pelvic incisions with subsequent suture ligature or fibrotic entrapment. With a Pfannenstiel incision, this injury is most likely to occur when the incision extends beyond the fascial aponeurosis to include the medial edge of the internal oblique muscle.5 During laparoscopic trocar insertion, the risk of injuring these nerves increases as the trocars are placed inferior to the anterior superior iliac spine.4,6 Palpation of the anterior superior iliac spine before trocar placement is useful for gaining lateral bearings.
Sciatic Neuropathy
The most common mechanism of injury to the sciatic nerve during gynecologic surgery is prolonged hip flexion resulting in nerve tension and stretching. Tension is increased with hip flexion when the knee joint becomes straightened or externally rotated. The sciatic nerve can stretch approximately 1.5 inches when the hip is flexed and the leg extended. Therefore, it is important to be cautious not to use excessive hip flexion when placing patients in stirrups, particularly the hanging type. When free-hanging stirrups are used for gynecologic cases, this injury has been reported in procedures lasting as short as 35 minutes.7
Effect of Carbon Dioxide Insufflation and Venous Gas Embolism
Effect of Carbon Dioxide Absorption
Capnography (ETCO2) and pulse oximetry are reliable markers of arterial gases in healthy patients. This may not apply to American Society of Anesthesiologists (ASA) class II and III. Increases in ETCO2 are usually due to absorption of CO2 from the peritoneal cavity. However, this may also be due to a variety of clinical circumstances that cause a ventilation/perfusion mismatch (V/Q) that increases the physiologic dead space. A steep Trendelenburg position and increased intra-abdominal pressures can accentuate this mismatch, especially in obese patients. A pneumoperitoneum will decrease pulmonary compliance. Obesity will decrease compliance further8 and increase the airway pressure required to ventilate the patient. Decreased cardiac output will also increase the V/Q mismatch and lead to increase in ETCO2.
Vascular Injuries during Laparoscopy
Veress Needle Injury
Avoidance
To avoid injury, laparoscopic surgeons must make every effort to place the Veress needle in the proper angle and direction (discussed in the section Retroperitoneal Vessel Injury). Once the needle is placed, the surgeon should attempt to demonstrate the intraperitoneal location of the needle tip before insufflation.
Retroperitoneal Vessel Injury
Injury of major abdominal blood vessels is a rare but treatable life-threatening complication of laparoscopy, which occurs in approximately 3 per 10,000 laparoscopies.11 These injuries most commonly occur during insertion of the Veress needle or the primary trocar.
Prevention
Injury to aorta and inferior vena cava can almost always be avoided by using the appropriate direction and angle for the insertion of both the Veress needle and primary trocar. It is common sense to direct the Veress needle and primary trocar toward the midline because the major retroperitoneal vessels bifurcate near the level of the umbilicus.12 However, because the exact midline is often difficult to gauge after the patient has been draped, the proper angle of insertion becomes especially important.
The best angle of insertion appears to change according to the patient’s body mass index (BMI=kg/m2) (see Chapter 44). In patients who are either in the ideal weight or overweight groups (corresponding BMI = 25kg/m2 and 25 to 30kg/m2, respectively), the Veress needle and primary trocar should be inserted through the umbilicus at 45 degrees from horizontal.13 A greater angle of insertion in these patients increases the risk of retroperitoneal vessel injury because the bifurcation is beneath the umbilicus in many cases, and the left common iliac vein is beneath the umbilicus in most patients.12 This is particularly important in the thinnest patients, in whom the distance from the umbilicus to the retroperitoneal vessels may be as little as 2 to 3 cm.13
Treatment
When a major vascular injury is suspected, the following steps should be taken without delay:
If either the surgeon or facility are not fully prepared to effectively treat a major vascular injury, thought should be given to using only an open laparoscopic technique or performing laparoscopy with a closed technique elsewhere.
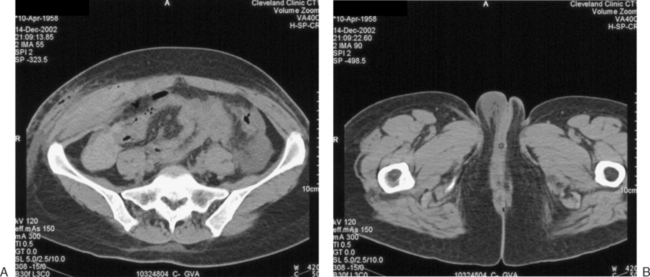
Abdominal Wall Vessel Injury
Damage to the deep vessels usually leads to immediate and rapid blood loss, whereas damage to the superficial vessels most often results in a persistent external trickle after the port is removed. Postoperatively, a superficial vessel injury (Fig. 45-2) typically presents with pain at the trocar site and a palpable mass. Postoperative deep vessel injury presents with increasing pain and decreasing hematocrit without a palpable mass because the vessels are located behind the rectus abdominis muscle or the bleeding occurs into the peritoneal cavity. A computed tomography scan will demonstrate the correct location of the hematoma.
Prevention
The primary method for avoiding injury to any of these vessels is to visualize the vessels before lateral trocar insertion. Two techniques have been used for this purpose: transillumination and direct laparoscopic visualization. Transillumination of the anterior abdominal wall with the laparoscopic light source is an effective way to visualize the superficial vessels in almost 90% of patients.14 The inferior epigastric vessels cannot be seen by transillumination because they lie beneath the rectus abdominis muscle and fascia. However, the inferior epigastric vessels can be directly visualized laparoscopically immediately beneath the peritoneum in 60% of patients where they lie between the insertion of the round ligament at the inguinal canal and the medial umbilical fold (see Chapter 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree