Chapter 41 Recurrent Pregnancy Loss
INTRODUCTION
Recurrent pregnancy loss is a profound personal tragedy to couples seeking parenthood and a formidable clinical challenge to their physicians. Spontaneous abortion occurs in approximately 15% of clinically diagnosed pregnancies in reproductive-age women, but recurrent pregnancy loss occurs in about 1% to 2% of this same population.1 Great strides have been made in characterizing the incidence and diversity of this heterogeneous disorder, and a definite cause of pregnancy loss can be established in approximately two thirds of couples after a thorough evaluation.2 A complete evaluation will include investigations into genetic, endocrinologic, anatomic, immunologic, microbiologic, thrombophilic, and iatrogenic causes. Recurrent pregnancy losses may induce significant emotional distress; in some cases intensive supportive care may be necessary. Successful outcomes will occur in more than two thirds of all couples.3
DEFINITION OF PREGNANCY LOSS
Several studies have recently indicated that the risk of recurrent miscarriage after two successive losses is similar to the risk of miscarriage in women after three successive losses; thus, it is reasonable to start an evaluation after two or more consecutive spontaneous miscarriages to determine the etiology of their pregnancy loss, especially when the woman is older than age 35 or when the couple has had difficulty conceiving.3,4 Any loss before 20 gestational weeks is considered a miscarriage. Some authors further divide these into embryonic losses, which occur before the ninth gestational week, and fetal losses, which occur at any time from the 9th gestational week to 20 weeks’ gestation, although there is no developmental phase to justify this distinction. Those couples with primary recurrent loss have never had a previous viable infant; those with secondary recurrent loss have previously delivered a pregnancy beyond 20 weeks’ gestation and then suffered subsequent losses. Other investigators advocate the designation of tertiary recurrent loss to identify those women who have multiple miscarriages interspersed with normal pregnancies.
RECURRENCE RISK
The main concerns of couples who have had a spontaneous abortion are the cause and the risk of recurrence. In a first pregnancy, the overall risk of loss of a clinically recognized pregnancy is 15%.5,6 The true rate of early pregnancy loss, however, is estimated to be around 50% because of the high rate of losses that occur before the first missed menstrual period. Studies that evaluated the frequency of pregnancy loss, based on highly sensitive tests for quantitative hCG, indicated that the total clinical and preclinical losses in women age 20 to 30 is approximately 25%, whereas the loss rate in women age 40 or more is at least double that figure.7,8 For women who have had one miscarriage, the risk of another loss rises slightly, to 14% to 21%. After two or three miscarriages the rate rises to 24% to 29% and 31% to 33%, respectively.9 The ability to predict the risk of recurrence is influenced by several factors.
Maternal Age
Advancing maternal age is associated with a higher rate of pregnancy loss of both normal and abnormal conceptuses.10,11 This probably reflects poor oocyte quality and reduced endocrine function in this group. In one study of more than 1 million pregnancies, the overall rate of spontaneous abortion was 11% and the approximate rates of clinically recognized miscarriage according to maternal age were 9% to 17% (age 20 to 30), 20% (age 35), 40% (age 40), and 80% (age 45).10
Pregnancy Outcome
Although the risk of miscarriage increases with each successive pregnancy loss, a pregnancy ending in a live birth reduces the risk of miscarriage in the subsequent gestation.12,13
Parity
Increasing parity is associated with an increased rate of spontaneous abortion.14 This may be partially explained by the correlation between maternal age and parity.
Gestational Age
The gestational age at the time of pregnancy loss should be considered in determining both the etiology of the loss and risk of recurrence. The recurrence risk increases as gestational age at the time of loss increases.11,15
ETIOLOGIES OF RECURRENT PREGNANCY LOSS
Genetic Factors
Chromosomal Disorders
Parental chromosome anomalies occur in 3% to 5% of couples with recurrent pregnancy loss as opposed to 0.2% in the general population. These include translocations, inversions, and the relatively rare ring chromosomes. Balanced translocations are the most common chromosomal abnormalities contributing to recurrent pregnancy loss.16 In recurrent pregnancy loss, this abnormality is found more frequently in the female partner, at a female-to-male ratio of from 2:1 up to 3:1.
Translocations
Robertsonian translocations involve two acrocentric chromosomes (numbers 13, 14, 15, 21, or 22) that fuse near the centromere region with loss of the short arms. Although a carrier of a Robertsonian translocation is phenotypically normal, there is a risk of unbalanced gametes and therefore unbalanced offspring. The risk of subsequent abortions varies with the type of translocation and the sex of the carrier. Robertsonian translocations are a more homogeneous group, and so the information on them is the most consistent. Studies indicate that when the Robertsonian translocation is maternal, there is a greater risk that the fetus will exhibit an unbalanced phenotype.17
Neri and coworkers found that carriers of these translocations had a 20% to 25% risk of spontaneous abortion. The only exceptions are translocations involving homologous chromosomes. If, for example, both copies of chromosome 22 fuse, the carrier should produce only trisomy 22 or monosomy 22, all of which would abort. Carriers of this type of translocation should therefore have a 100% rate of pregnancy loss, but two unexplained normal offspring from such carriers have been reported.18,19
Inversions
Chromosomal inversions occur less frequently than translocations. An inversion occurs when a single chromosome undergoes two breaks and is reconstituted, with the segment between the breaks inverted. Inversions are of two types: paracentric, in which both breaks occur in one arm, and pericentric, in which there is a break in each arm. An inversion does not usually cause an abnormal phenotype in carriers, because it is a balanced rearrangement. Its medical significance is for the progeny; a carrier of either type of inversion is at risk of producing abnormal gametes that may lead to pregnancy loss. A female inversion carrier is at an approximately 8% risk of producing anomalous offspring; the risk is reduced to 4% in male carriers.20
Ring Chromosomes
Ring chromosomes are formed when a chromosome undergoes two breaks and the broken ends of the chromosome reunite in a ring structure. Ring chromosomes are quite rare; because of mitotic instability, it is not uncommon for ring chromosomes to be found in only a proportion of cells. The medical literature is limited to isolated case reports, and the specifics of the effects of ring chromosomes on recurrent pregnancy loss are not known.21
Recurrent Aneuploidy
The first chromosomally abnormal abortus was documented in 1961, and since then a large body of data on the chromosomal status of spontaneous abortuses has accumulated. The overall frequency of chromosome abnormalities in spontaneous abortions is at least 50%. Of these abnormalities, most are numerical: 52% are trisomies, 29% are monosomy 45,X, 16% are triploidies, 6% are tetraploidies, and 4% are structural rearrangements.22 The earlier the abortion, the higher the chance of chromosomal abnormality. In Boúe’s study,22 66% of abortions at 2 to 7 weeks’ gestation were abnormal, whereas the percentage fell to 23% for abortions at 8 to 12 weeks’ gestation.
Evidence suggests that some couples are at risk for conceptions complicated by recurrent aneuploidy. Empirically, the birth of a trisomic infant places a woman at an approximate 1% increased risk for a subsequent trisomic conceptus.23 Germline mosaicism has been reported in recurrent cases of Down syndrome and may also be responsible for recurrent aneuploidy in some couples.24
Single-Gene Mutations
The role of single-gene mutations at the molecular level in recurrent pregnancy loss remains speculative. It is known from studies in transgenic mice that some selected mutations and inactivation of some specific transcription factors can cause pregnancy failure.25 It is speculated that similar mutations in genes required for embryonic, placental, or cardiac development in humans are likely to cause pregnancy loss.
X-Inactivation
In somatic cells of female mammals, only one X chromosome is active. Inactivation of the second X occurs early in embryonic life to achieve dosage compensation with males. The inactive X may be paternal or maternal; it is entirely a matter of chance which of the pair becomes inactivated in a cell. Occasionally, preferential inactivation of one allele occurs. Extremely skewed X-inactivation, defined as more than 90% inactivation of one allele, is observed in 2% of newborns and 4.5% of reproductive-age women.26
Several authors have found the skewed X-inactivation pattern in phenotypically normal women with recurrent pregnancy loss.27,28 Others have also found a statistically significant increase in the spontaneous abortion rate among family members who carried the skewed X trait.29 Presumably these women have an X-linked mutation or germline mosaicism.
Endocrinologic Factors
Luteal Phase Defect
Maintenance of early pregnancy depends on the production of progesterone by the corpus luteum. Between 7 and 9 weeks’ gestation the developing placenta takes over progesterone production. Luteal phase defect is defined as an inability of the corpus luteum to secrete progesterone in high enough amounts or for too short a duration. Abnormalities of the luteal phase have been reported to occur in up to 35% of women with recurrent abortion.30
Several potential mechanisms are thought to give rise to a luteal phase defect: decreased production of progesterone by the corpus luteum, decreased follicle-stimulating hormone (FSH) levels in the follicular phase, abnormal patterns of luteinizing hormone (LH) secretion, decreased response by the endometrium to already-secreted progesterone, and increased prolactin levels. The preponderance of evidence suggests that luteal phase defect is a preovulatory event most likely linked to an alteration in preovulatory estrogen stimulation, which may indicate poor oocyte quality and a poorly functioning corpus luteum.31,32
Some authors have advocated the measurement of serum progesterone levels in the luteal phase for the diagnosis of luteal phase defect, with levels below 10 ng/mL considered abnormal.33 However, progesterone levels are subject to large fluctuations because of pulsatile release of LH. Moreover, there is a lack of correlation between serum levels of progesterone and endometrial histology.34 Nonetheless, serum progesterone levels of 10 ng/mL or greater in the midluteal phase of the menstrual cycle are generally utilized to exclude luteal phase defect.
Untreated Hypothyroidism
Untreated hypothyroidism may increase the risk of miscarriage. A recent study of more than 700 patients with recurrent pregnancy loss identified 7.6% with hypothyroidism.35 Hypothyroidism is easily diagnosed with a sensitive thyrotropin test, and patients should be treated to become euthyroid before attempting a next pregnancy. It has also been suggested that thyroid antibodies are elevated in women with recurrent pregnancy loss. A retrospective study of 700 patients with recurrent pregnancy loss demonstrated that 158 women had antithyroid antibodies but only 23 of those women had clinical hypothyroidism on the basis of an abnormal thyrotropin value.36 The presence of antithyroid antibodies may imply abnormal T-cell function; therefore, an immune dysfunction rather than an endocrine disorder may be responsible for the pregnancy losses.
Insulin Resistance
Patients with poorly controlled diabetes are known to have an increased risk of spontaneous miscarriage, which is reduced to normal spontaneous loss rates when women are euglycemic preconceptually.37 Hyperglycemia and vascular complications resulting in compromised blood flow to the uterus may be responsible for the pregnancy loss. It is known that women with PCOS have an increased risk of miscarriage. The mechanism is unknown, but may be related to elevated serum LH levels and high testosterone and androstenedione concentrations, which may adversely affect the endometrium.38 It also may be related to the high prevalence of insulin resistance in these women.39 Testing for fasting insulin and glucose is simple, and treatment with insulin-sensitizing agents may reduce the risk of recurrent miscarriage.40
Elevated Day 3 FSH
Elevated day 3 FSH levels have been associated with decreased pregnancy rates in women undergoing in vitro fertilization (IVF). Although the frequency of elevated day 3 FSH levels in women with recurrent miscarriage is similar to the frequency in the infertile population, the prognosis for recurrent miscarriage is increased with increased day 3 FSH levels.41 Thus, it is speculated that women with recurrent pregnancy loss and elevated day 3 FSH levels may have poor quality oocytes with inherent chromosomal abnormalities. Although no treatment is available, testing should be performed in women over age 35 with recurrent pregnancy loss, and appropriate counseling should follow.
Hyperprolactinemia
Normal circulating levels of prolactin may play an important role in maintaining early pregnancy. Data from animal studies suggest that elevated prolactin levels may adversely affect corpus luteal function; however, this concept has not been proven in humans.42 A recent study of 64 hyperprolactinemic women showed that bromocriptine therapy was associated with a higher rate of successful pregnancy and that prolactin levels were significantly higher in women who miscarried.43
Anatomic Factors
Anatomic uterine defects are present in 15% to 20% of women evaluated for three or more consecutive spontaneous abortions.2 These anatomic abnormalities can be classified as congenital or acquired. Uterine malformations appear to predispose women to reproductive difficulties, including first- and second-trimester fetal losses, preterm labor, and abnormal fetal presentation.
Congenital Uterine Anomalies
Congenital malformations of the reproductive tract result from failure to complete bilateral duct elongation, fusion, canalization, or septal resorption of the müllerian ducts. Müllerian anomalies were found in 8% to 10% of women with three or more consecutive spontaneous abortions who underwent hysterosalpingography or hysteroscopic examination of their uteri.2,44 Inadequate vascularity, compromising the developing placenta, and reduced intraluminal volume have been theorized as possible mechanisms leading to pregnancy loss.
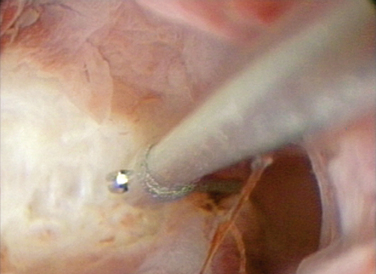
The most common abnormality associated with pregnancy loss is the septate uterus. The spontaneous abortion rate is high, averaging about 65% of pregnancies in some studies.45 A septum is primarily composed of fibromuscular tissue that is poorly vascularized (Fig. 41-1). This lack of vascularization may compromise decidual and placental growth. Alternatively, a uterine septum may impair fetal growth as a result of reduced endometrial capacity or a distorted endometrial cavity.45 Uncontrolled studies suggest that women who undergo resection of the uterine septum have higher delivery rates than women without treatment. Other congenital abnormalities, such as uterus didelphys, bicornuate uterus, and unicornuate uterus, are more frequently associated with later trimester losses or preterm delivery.
Diethylstilbestrol Exposure
Diethylstilbestrol (DES) is an orally active synthetic estrogen that was introduced in the 1940s for the treatment of recurrent pregnancy loss, premature delivery, and other complications of pregnancy. The use of DES in pregnancy was banned in 1971.46
Uterine abnormalities occur in 69% of women exposed to DES in utero.46 The most common abnormality is a T-shaped uterine cavity (70%). Other abnormalities include a small uterus, constriction rings, and intrauterine filling defects. In addition, 44% of DES-exposed women have structural changes in the cervix, including an anterior cervical ridge, cervical collar, hypoplastic cervix, and pseudopolyp. Women with a history of in utero exposure to DES appear to have a greater risk of adverse pregnancy outcome, including a twofold increased risk of spontaneous abortion and a ninefold increase in ectopic pregnancy rates.47
Acquired Uterine Abnormalities
Intrauterine Masses
Intrauterine cavity abnormalities, such as leiomyomas and polyps, can contribute to pregnancy loss. There are several hypotheses concerning how leiomyomas may be associated with recurrent pregnancy loss. Depending on the leiomyoma size and location, it may partially obliterate or alter the contour of the intrauterine cavity, providing a poorly vascularized endometrium for implantation or otherwise compromising placental development. Uterine leiomyomas and polyps may also act like an intrauterine device (IUD), causing subacute endometritis. Until recently, it was felt that only submucous leiomyomas should be surgically removed before subsequent attempts at pregnancy. However, several recent studies investigating the implantation rate in women undergoing IVF have clearly demonstrated decreased implantation with intramural leiomyomas in the range of 30 mm.48 When smaller leiomyomas are identified, it is unclear if myomectomy is beneficial.49
Incompetent Cervix
Cervical incompetence can be considered an acquired uterine anomaly that is associated with recurrent pregnancy loss. The diagnosis of cervical incompetence is based on the presence of painless cervical dilation resulting in the inability of the uterine cervix to retain a pregnancy. Cervical incompetence commonly causes pregnancy loss in the second trimester. It may be associated with congenital uterine abnormalities, such as septate or bicornuate uterus. Rarely, it may be congenital following in utero exposure to DES.47 It has been reported that trauma to the cervix from conization, loop electrosurgical excision procedures, dilation of the cervix during pregnancy termination, or short cervical lengths on ultrasound increase the risk of cervical incompetence.50
IMMUNOLOGIC FACTORS
The primary function of the immune system is to recognize and eliminate potentially pathogenic organisms from the body. To understand how immunologic factors can affect pregnancy, a basic understanding of the normal immune response is required. The immune response has two components: the innate, or nonspecific, immune response and the acquired, or adaptive, immune response.
Innate and Acquired Immune Responses
Acquired or adaptive immune responses are antigen-specific and lead to memory, but require 4 to 7 days to be effectively generated. T cells and B cells and a small proportion of NK cells largely mediate these responses. B cells differentiate in bone marrow. T and B cells occur in tissues in approximately equal numbers. T cells are responsible for cell-mediated immunity and are essential for B-cell function.51
T-helper Lymphocytes
T cells produce a range of cytokines following an immune challenge. The type of cytokine determines their differentiation into T helper 1 (Th1) and T helper 2 (Th2) lymphocytes. For example, Th1 lymphocytes secrete interleukin-2 (IL-2) and IFN-γ, creating a pro-inflammatory environment. Conversely, Th2 lymphocytes secrete cytokines, such as IL-4 and IL-10, that are predominantly involved in antibody production following an antigenic challenge. The actions of the two types of lymphocytes are intertwined, acting in concert and responding to counterregulatory effects of their cytokines. Hormones have a powerful effect on this action. During their reproductive years, women are more likely to develop a Th1 response after challenge with an infectious agent or antigen, except during pregnancy, when a Th2 environment prevails.52
Autoimmune Factors: Maternal Response to Self
In some instances, there is a failure in normal control mechanisms that prevents an immune reaction against self, resulting in an autoimmune response.53 Autoantibodies to phospholipids, thyroid antigens, nuclear antigens, and others have been investigated as possible causes for pregnancy loss.35 Antiphospholipid antibodies include both the lupus anticoagulant and anticardiolipin antibodies. There is still controversy concerning testing for other phospholipids, but an increasing number of studies suggest that antibodies to phosphatidyl serine are also associated with pregnancy loss.54
Systemic Lupus Erythematosus
Most clinical studies find that pregnancy loss is more common among women with systemic lupus erythematosus (SLE) than among normal women.55 The rate of spontaneous abortions among patients with SLE in one large study was estimated at 21%.56 Nearly three quarters of pregnancy losses appear to occur in the second and third trimesters.57 Most fetal deaths in women with SLE are associated with the presence of antiphospholipid antibodies.55,58 In a study of women with SLE and recurrent pregnancy loss, women with antiphospholipid antibodies had a tenfold increased risk of miscarriage compared to women with SLE but without antiphospholipid antibodies.55 Other factors associated with pregnancy loss in this population include (1) disease activity before conception, (2) the onset of SLE during pregnancy, and (3) underlying renal disease. Women with active SLE should be advised to delay conception until remission is established. Women with moderate renal insufficiency should be advised against pregnancy. Women should also be counseled about the higher rates of preeclampsia and premature delivery with SLE.57
Antiphospholipid Antibody Syndrome
Antiphospholipid antibody syndrome is an autoimmune condition characterized by the production of moderate to high levels of antiphospolipid antibodies and certain clinical features. The presence of antiphospholipid antibodies (anticardioplipin and lupus anticoagulant) during pregnancy is a major risk factor for adverse pregnancy outcome.59 In a large meta-analysis of studies of couples with recurrent abortion, the incidence of antiphospholipid antibody syndrome was between 15% and 20%, compared to about 5% in nonpregnant women without a history of obstetric complications.60 It is not yet understood how antiphospholipid antibodies arise in patients with the syndrome. Genetic factors and infection may play a role. The antibodies generated in patients with antiphospholipid antibody syndrome appear to recognize epitopes on phospholipid-binding proteins, unlike the antibodies that arise following infections such as syphilis and Lyme disease, which recognize phospholipids directly.61
Several mechanisms have been proposed by which antiphospholipid antibodies might mediate pregnancy loss. It appears that different coagulation proteins may be involved in binding to phospholipids, which may explain the predisposition to thrombosis. Antibodies against phospholipids could increase thromboxane and decrease prostacyclin synthesis within placental vessels. The resultant prothrombotic environment could promote vascular constriction, platelet adhesion, and placental infarction.60 Antiphospholipid antibodies appear to interfere with various components of the protein C antithrombotic pathway, including inhibiting the formation of thrombin, decreasing protein C activation by the thrombomodulin–thrombin complex, inhibiting assembly of protein C complex, inhibiting activated protein C activity, and binding to factors Va and VIIIa in ways that protect them from proteolysis by activated protein C.61 Another proposed mechanism is the disruption of the placental antithrombotic molecule, annexin V. The levels of annexin V are reduced in placental villi of women with recurrent pregnancy loss who are antiphospholipid antibody-positive.62 Antiphospholipid antibodies can also recognize heparin and heparinoid molecules and thereby inhibit antithrombin III activity.63 Antiphospholipid antibodies can interact with cultured human vascular endothelial cells with resultant injury or activation.61 A more direct action on the trophoblastic cells has been demonstrated and explains how antiphospholipid antibodies can cause early fetal loss. Antiphospholipid antibodies have been demonstrated to inhibit secretion of human placental chorionic gonadotropin and to inhibit the expression of trophoblast cell adhesion molecules (α1 and α5 integrins, E- and VE-cadherins).64
Antithyroid Antibodies
An increased frequency of antithyroid antibodies (antithyroid peroxidase, antithyroglobulin) have been reported in women with recurrent pregnancy loss. However, if the patient is euthyroid, the presence of antithyroid antibodies does not affect pregnancy outcome.65 Women who have positive antithyroid antibodies and are euthyroid are at an increased risk for hypothyroidism during and after pregnancy. These women should have their thyrotropin level tested during each trimester and postpartum for thyroiditis.66
Antinuclear Antibodies
Approximately 10% to 15% of all women will have detectable antinuclear antibodies regardless of their history of pregnancy loss. Their chance of successful pregnancy outcome is not dependent on the presence or absence of antinuclear antibodies. Treatments such as steroids have been shown to increase the maternal and fetal complications without benefiting live births67; thus, routine testing and treatment for antinuclear antibodies is not indicated.
Alloimmune Factors: Maternal Immune Response to Trophoblast
Implantation is the process by which the embryo is intimately connected with the maternal uterine and blood-borne cells. The implanting embryo possesses paternal antigens and therefore may be rejected as an allograft. However, in most cases, fetal rejection by the maternal immune system does not occur and seems to be prevented by mechanisms not yet defined. Alloimmune factors have been suggested to be associated with recurrent pregnancy loss. HLA sharing was thought to be associated with recurrent pregnancy loss based on a decreased maternal immune response and, thus, decreased production of blocking antibodies. Recent large studies, however, reveal no association between HLA (and HLA-DQα) homozygosity, and recurrent pregnancy loss.68 Other investigators have implicated certain embryotoxic factors, such as tumor necrosis factor (TNF-α) and IFN-δ, identified in the supernatants of peripheral blood lymphocytes from women with pregnancy loss; however, this has not been confirmed by independent studies. Immunophenotypes of endometrial cells from women with recurrent pregnancy loss demonstrate altered NK cell (CD56+) populations. Some have suggested that increased NK cells are associated with pregnancy loss, whereas others have indicated that decreased NK cells are associated with pregnancy loss. None of these findings have been clearly associated with pregnancy loss; thus, there are no definite recommended tests at this time.69 Several theories have been proposed to account for the immune-privileged state of the decidua.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree