Chapter 39 Combined Biliary and Duodenal Obstruction
Background and Overview
Pancreatic cancer is the most common cause of combined biliary and duodenal obstruction. There are multiple other tumors that can also lead to this type of combined obstruction, including ampullary cancer, cholangiocarcinoma, gallbladder cancer, gastric cancer, and metastatic lesions either to the head of the pancreas or around the head of the pancreas. A study involving 17 patients with metastatic cancer to the pancreas showed that renal cell carcinoma was the most common site of primary cancer (8 of 17 patients, 47%).1 Other primary tumors in the same study included medullary carcinoma of the thyroid, lymphoma, alveolar rhabdomyosarcoma, squamous cell carcinoma of the esophagus, squamous cell carcinoma of the lung, and small cell carcinoma of the lung.
In a study of 64 patients with combined biliary and duodenal obstruction, etiologies of obstruction were primary pancreaticobiliary cancer in 84% of patients, gastric cancer in 7.8% of patients, metastatic cancer (colon, breast, kidney) in 6.2% of patients, and an anastomotic recurrence in a single patient.2 In a retrospective review of 18 patients undergoing simultaneous treatment of malignant biliary and duodenal obstruction, the underlying disease process was pancreatic cancer in 78% of patients, biliary cancer in 11% of patients, lymphoma in 5% of patients, and metastatic cancer in 1% of patients.3
An awareness of how often patients with initial biliary obstruction will later require duodenal stent placement for duodenal obstruction is important for planning endoscopic therapy. It is also important to consider how often patients with initial duodenal obstruction will later require biliary stent placement for biliary obstruction. The latter situation is less common. In a study of endoscopic therapy for malignant gastric outlet obstruction, 16 of 36 patients (44%) developed malignant biliary obstruction in addition to their gastric outlet obstruction (9 patients with pancreatic cancer, 2 patients with duodenal cancer, 2 patients with metastatic colon cancer, 2 patients with cholangiocarcinoma, and 1 patient with gallbladder cancer).4 Malignant biliary obstruction occurred before development of gastric outlet obstruction in 9 patients, concurrently in 4 patients, and developed after enteral stenting in 3 patients. A separate study showed that in patients who received plastic biliary stents for malignant obstruction, 6% to 9% of the patients later developed duodenal obstruction (requiring gastrojejunostomy), again highlighting the joined nature of these conditions.5
After the development of combined biliary and duodenal obstruction, overall survival time is poor. In one study of 64 patients treated endoscopically for combined biliary and duodenal obstruction, overall median survival after stenting was 81 days.2 This is somewhat unsurprising, as gastric outlet obstruction alone is usually associated with unresectable disease.4 In other studies, similarly short survival times have been noted in patients treated endoscopically for combined biliary and duodenal obstruction, with median survival times of 78 days.3,6
Comparison of Surgical versus Endoscopic Palliation
In a prospective study of 39 patients with malignant gastric outlet obstruction, 18 patients were randomized to gastrojejunostomy and 21 were randomized to stent placement.7 Food intake improved more rapidly in the stent group, but long-term relief was better after surgery using Adler and Baron’s Gastric Outlet Obstruction (GOO) Scoring System.4 This study also found more major adverse events, recurrent obstructive symptoms, and reinterventions in the stent group compared with the surgical group. There were no significant differences in median survival time or quality of life between the two groups.
Another prospective study randomized 27 patients with malignant gastric outlet obstruction to laparoscopic gastrojejunostomy or duodenal stent placement.8 In contrast to the prior study, the adverse event rate with the stent group was lower, with no adverse events in the stent group and 8 of 13 patients (62%) in the surgery group developing adverse events. The stent group also experienced a significant improvement in physical health (using an SF-36 questionnaire), while the surgery group did not. Cumulative survival over the first year was similar among the two groups.
A meta-analysis evaluated outcomes of 307 procedures from 9 studies comparing endoscopic stenting and surgical gastroenterostomy for palliation of malignant gastroduodenal outlet obstruction.9 Endoscopic stenting was associated with higher clinical success, shorter time to initiation of oral intake, lower incidence of delayed gastric emptying, shorter hospital stay, and less morbidity than the surgical group. There was no significant difference in 30-day mortality between the two groups. A decision analysis study that compared open gastrojejunostomy, laparoscopic gastrojejunostomy, and endoscopic stenting for palliation of malignant gastric outlet obstruction showed that stenting resulted in the lowest mortality and the lowest cost of the three treatment options.10
Type 1-2-3 System
Mutignani et al. developed a simple classification system to describe the three most common anatomic scenarios of combined duodenal and biliary obstruction based on the relation of the duodenal obstruction to the major papilla.2 The type of anatomic obstruction will help determine the type of endoscopic approach for treatment and the likelihood of technical success.
Type 1 gastric outlet obstruction occurs at the level of the duodenal bulb or upper duodenal genu, but without involvement of the major papilla. Type 2 obstruction occurs in the second portion of the duodenum with involvement of the major papilla. Type 3 obstruction occurs in the third portion of the duodenum distal to and without involvement of the major papilla. Type 3 obstruction is the least common type of combined obstruction and typically occurs secondary to pancreatic cancer arising from the uncinate process, although it can be seen in patients with primary small bowel cancer as well.2 Technical difficulty of endoscopic therapy for combined obstruction is thought to be most difficult with type 2 obstruction, least difficult with type 3 obstruction, and intermediate with type 1 obstruction.11
Endoscopic Treatment of Type 1 Obstruction
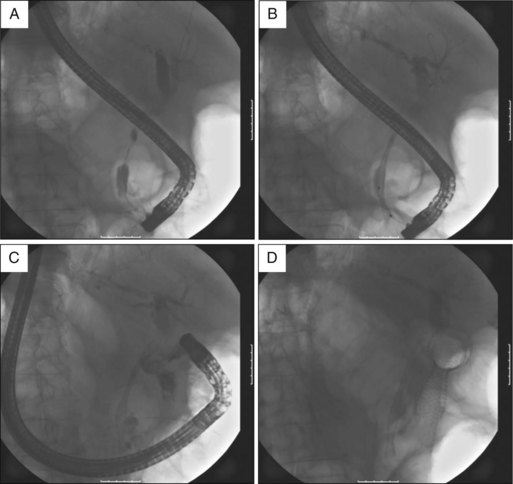
Type 1 obstruction occurs at the level of the duodenal bulb or upper duodenal genu, without involvement of the major papilla (Fig. 39.1). There are two different scenarios that can occur with type 1 obstruction, one in which the duodenoscope is able to pass beyond the duodenal stricture to the major papilla and the other in which the duodenoscope is not able to pass beyond the duodenal stricture to the major papilla.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree