Author
Year
N° pts
PSA (mean; ng/ml)
N° cores
Cancer detection rate (%)
Borboroglu et al. [48]
2000
57
8.6
22.5
30
Stewart et al. [49]
2001
224
8.7
23
34
Fleshner and Klotz [50]
2002
37
22.4
32–38
13.5
Rabets et al. [51]
2004
116
9.2
22.8
29
Patel et al. [52]
2004
100
9.4
20–24
25
Pinkstaff et al. [53]
2005
210
13.6
21.2
37
Walz et al. [54]
2006
161
9.4
24.2
41
As PSA has a sensitivity of about 21 % only and a specificity of 60–70 % at the cut off 4 ng/mL, any avenues have been explored to improve its sensitivity. These include a lower cut off, age-specific or age-adjusted PSA, PSA density (PSAD), PSAD density transition zone (PSA-TZ), PSA velocity (PSAV), free PSA/ total PSA, % free PSA and various PSA molecular forms [55].
Percent-Free PSA
PSA occurs in two major forms in the blood. One form is attached to blood proteins while the other circulates free (unattached). The percent-free PSA (fPSA) is the ratio of free PSA circulates compared to the total PSA level. Percent free PSA has been demonstrated to improve PSA usefulness both in the grey zone (PSA 4–10 ng/ml) and from 2.5 to 4 ng/ml [56]. The recommended cut-off to recommend prostate biopsies is 10 % or less, although men should be cautious if it is between 10 and 25 % as this is considered the grey zone. The major problem of free PSA is that its value is influenced by prostate volume and associated prostatitis. Furthermore, the cut-off of 25 % is far from being universally agreed upon.
PSA Density
PSA levels are higher in men with larger prostate glands [57]. The PSA density (PSAD) is sometimes used for men with large prostate glands to try to adjust for this observation. The classical cut-off is 0.15 ng/ml/cc. PSA density has not been shown to be as useful as the percent-free PSA test in clinical practice although it is integrated sometimes in risk calculators.
PSA Density of the Transition Zone
PSA adjusted for transition zone volume (PSA density of the transition zone) has been shown to be more accurate than the prostate-specific antigen density in distinguishing prostate cancer from benign prostatic hyperplasia in men with intermediate serum prostate-specific antigen of 4.1–10.0 ng/mL, from 2.5 to 4 ng/ml and in men with initial negative biopsies. Limitations to its widespread use include the variability of the transition zone measurement by TRUS [56, 58, 59].
Age-Specific PSA Ranges
PSA levels are normally higher in older men than in younger men, even when there is no cancer. This is because a major source of PSA leakage comes from the transition zone of the prostate which enlarges as men age. However, due to the usefulness of age-specific PSA ranges is not well proven, most authors do not recommend their use at this time outside of being integrated in risk calculators or nomograms.
PSA Velocity
PSA increases more rapidly in men with prostate cancer than in healthy men. The Baltimore Longitudinal Study of Aging (BLSA) found that men with a PSA rate of change (PSA velocity) greater than 0.75 ng/mL/year were at an increased risk of being diagnosed with prostate cancer and that PSA velocity was more specific than a 4.0 ng/mL PSA cutoff (90 versus 60 % specificity). The study results, though, were based on analyzing the banked serum of only 18 cancer cases, PSA velocity and its cut-off [60].
Data from the Rotterdam arm of the ERSPC trial found that PSA velocity was significantly higher in men with prostate cancer than in men with a negative biopsy (0.62 vs. 0.46 ng/mL/year). However, PSA velocity did not independently predict cancer after adjusting for PSA level [61].
Repeat TRUS Biopsy
Urologists are frequently faced with the dilemma of treating a patient with a high index of suspicion for prostate cancer, but with an initial set of negative biopsies. Negative biopsy does not ensure the absence of disease [62]. Whatever parameter is used to determine the need for a repeat biopsy, it is important to have a look at first the initial biopsy. Factors to consider include the location and number of cores taken as well as the size of the prostate.
If the prior negative biopsy was a sextant scheme, the cancer detection rate may be as high as 39 % with a repeat extended biopsy, whereas if the prior negative biopsy was an extended scheme, the cancer detection rate is usually much lower between 15 and 30 %. Saturation biopsy techniques and transperineal templates have also been proposed but supplanted nowadays by imaging techniques like MRI [34]. The variability in cancer detection rates does not justify its invasiveness (Table 40.1). Others have proposed up to 21 biopsies in previously negative biopsies [63].
Prostate Biopsy After Radiotherapy
Post-radiotherapy (RT) prostate biopsies are likely to pose problems in histological interpretation. False negatives due to sampling error, false positives due to delayed tumour regression, and indeterminate biopsies showing radiation effect in residual tumour of uncertain viability are common occurrences [64]. However, with very experienced uro-pathologists, these limitations can be minimized.
Predictors of a Positive Biopsy
The main aims of the TRUS biopsy are not only to diagnose prostate cancer but also to determine its aggressiveness. This is especially true at a time of increased complication risks after TRUS biopsies and with the dilemma posed by low volume, low grade prostate cancer. Nomograms are often used to predict the likelihood of a positive biopsy and several have now incorporated more extended biopsy schemes in their calculations, including for repeat biopsies [65].
Prostate Biopsy Technique
Transrectal ultrasound (TRUS)–guided biopsy is the preferred method except in patients who had the rectum and anus excised, in which case the biopsy is performed by the transperineal route. TRUS is carried out by using a 5- to 8-MHz handheld high-resolution probe with capabilities of sagittal and transverse (coronal) imaging (Fig. 40.1). A disposable adaptor is fitted on the probe that will direct the biopsy needle into various regions of the prostate as guided by ultrasound imaging. Currently, extended schemes consisting of at least 10–12 biopsies including lateral biopsies, but without transition zone biopsy, is now considered as the diagnostic gold standard (Fig. 40.2). Some authors have argued that more extended schemes minimize the risk of missing an aggressive disease but this remains debated [66]. Extended schemes decrease the grade discordance between biopsy and prostatectomy specimens but increase the risk of detecting insignificant prostate cancer.
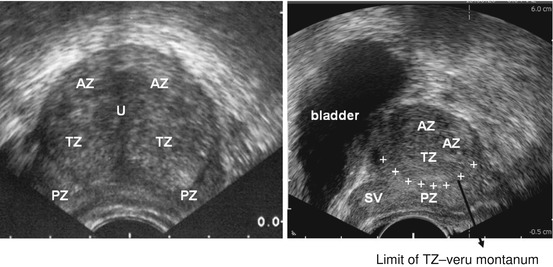
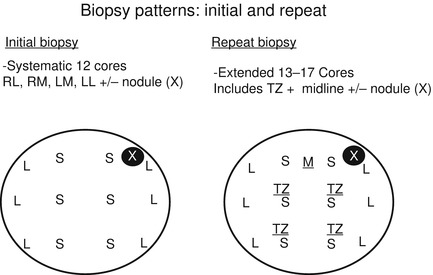
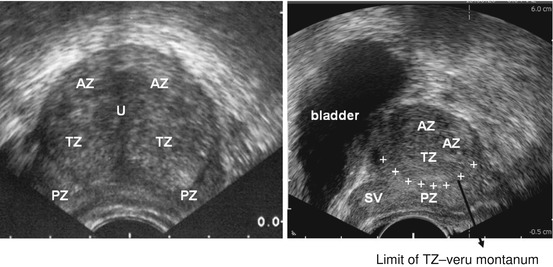
Fig. 40.1
Transverse and sagittal view of prostate during Ultrasound. AZ anterior zone, U urethra, TZ transitional zone, PZ peripheral zone, SV seminal vesicles
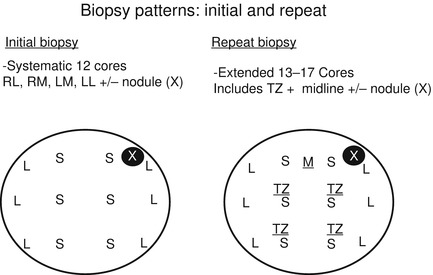
Fig. 40.2
Initial and repeat biopsy schemes at UHN, Toronto (Courtesy of Dr. Ants Toi, University Health Network, Toronto, Canada)
Principles of the TRUS Examination
Informed Consent
Alternatives, consequences, and complications of biopsy are discussed prior to the procedure. Patients should have clear directions in dealing with the complications of a TRUS biopsy, including risk of hospitalization and sepsis.
Antibiotic Prophylaxis
Oral aminoquinolones in the form of ciprofloxacin or norfloxacin are sufficient in uncomplicated cases but cases of resistance to quinolones are the source of increasing concern. It is important for centers to be aware of local microbiological trends and antibiotic resistance. Standard rectal swabs are not performed beforehand and there are logistical difficulties in trying to do them, however, with infection rates rising, the findings of rectal swabs may become more and more important in the future. Patients with cardiac valve problems should receive intravenous antibiotics although this is not universally agreed upon. Meropenem should be considered for post-biopsy urosepsis [67].
Anticoagulation
These medications are discontinued for several days prior to the biopsy although aspirin can be continued. In high risk patients, hospitalization and parenteral heparin cover may be necessary.
Digital Rectal Examination
Digital rectal examination should be performed prior to the biopsy to make sure that rectum is empty and to rule out rectal pathology. In some centers, an enema is routine prior to TRUS biopsy. In addition, DRE will help to note any abnormal areas in the prostate and the presence of a nodule. These areas are included in the biopsies.
Pain Relief
Patients feel pain and discomfort because of the ultrasound probe and needle passage through the prostate gland, particularly below the dentate line in the anorectum [68]. Patients also experience considerable psychological stress because of the fear of impending cancer diagnosis. The pain induced during the procedure can lead to contraction of pelvic floor muscles causing exacerbation of pain. Periprostatic infiltration with 1–2 % lignocaine significantly decreases the pain during the procedure [68].
Biopsy
The anatomy of the prostate, bladder, seminal vesicles, and ampulla of vas is examined for asymmetry and distortion. This is followed by examination of the prostate for abnormal shadows, hypoechoic areas, erosion of capsule, and volume measurement. The gland is scanned in both the sagittal and coronal planes. The width of the prostate is measured in the axial (coronal) plane and the length of the prostate is measured in the sagittal plane, including the transition zone of the prostate. Most of the TRUS machines have the capability for calculation of volume.
The zonal anatomy of the prostate is described in Chap. 39. As 70 % of cancers occur in the peripheral zone and nearly 25 % occur in the central zone, biopsies of the posterior part of the prostate seem logical, and for biopsy purposes, the prostate gland can be divided into base, midregion, and apex. The transition zone is included in repeat biopsies. The needle tip is placed near the region of the intended biopsy and the gun is fired to get the sample. The length of the biopsy core also determines the detection rate, particularly at the apex, with a longer core giving higher detection rates. Each core is sent to the laboratory in a separate container properly libelled for histological diagnosis.
Role of Transition Zone Biopsies
In men with previously negative biopsies, TRUS-guided TZ biopsy should be done to exclude the cancer. Also with the increasing use of MRI and fusion MRI and TRUS, the TZ may be specifically targeted. There is no demonstrated role of TZ biopsies on the initial biopsies though.
Role of Real-Time MRI-TRUS Fusion for Guidance of Targeted Prostate Biopsies
The current biopsy process is blind, involving 12 or more random needle samples but new technology such multi-parametric magnetic resonance imaging (MRI) coupled with transrectal ultrasound (TRUS) guided biopsy (called fusion technology) can accurately identify men with prostate cancer who are at risk of developing aggressive disease or target lesions not identified on TRUS examination, often in the anterior zone of the prostate [69–71].
Complications
Transrectal guided prostate biopsy is not without risks and complications. Taking more biopsy cores does not necessarily increase the complication rates [72]. Most of the following complications are minor and self-limiting but can cause considerable anxiety to the patients. Bleeding: urethral bleeding/hematuria (35 %), hematochezia (9 %), and hematospermia (5 %) are usually self-limiting and do not need any active treatment. Infections: prostatitis, epididymitis, and septicemia; sepsis is the most dangerous complication as it can be life-threatening in elderly patients. Outflow symptoms: painful micturition. Urine should be tested for infection and appropriate antibiotics usually improve symptoms. Urinary retention could be precipitated by the biopsy due to hemorrhage and edema. Catheterization is done to relieve the obstruction and a trial removal can be done a couple of days later.
Staging Investigations
Prostate cancer spreads locally within its zones and into the ejaculatory ducts, seminal vesicles, and neurovascular bundles. Distal spread includes lymphatic (to internal iliac lymph nodes) and hematogenous routes to bones, lungs, and other organs. The bony metastasis involves bones of the axial skeleton. Visceral metastasis is rarely seen in newly diagnosed patients and rarely seen even in patients dying of prostate cancer [73].
For clinical staging the extent of the prostate cancer is assessed by DRE, PSA, TRUS, and Gleason histological grading. For example, in patients with stage T1c or less disease with a total Gleason Score of 6 and a PSA of less than 10 ng/mL, no further staging investigations would be required unless there is a specific indication, like symptoms [74]. Selective cross-sectional imaging modalities like computed tomography (CT), MRI and bone scan help to assess the extent of spread and are mainly performed for the following reasons:
1.
To determine lymph node status in high-risk patients as well as bone metastases
2.
Apical disease to guide for surgical management
3.
Suspected locally advanced disease
4.
Prior to radiotherapy
The risk of metastasis can be quantified by PSA levels, number of positive cores and clinical and TRUS biopsy findings. Noteworthy, in contemporary patients with PCa, the accuracy of CT scan as a preoperative nodal-staging procedure is poor, even in patients with high risk of lymph node involvement [75].
Magnetic Resonance Imaging for Prostate Cancer Staging
Magnetic resonance imaging has a number of advantages over CT in prostate cross-sectional imaging. It helps in the detailed evaluation of prostatic, periprostatic, and pelvic anatomy and therefore mostly is used as a staging study in men with biopsy-proven prostate cancer. T1 corresponds to haemorrhage, lymph nodes, bone metastasis, short T1 inversion recovery investigates bone metastasis, T2 defines prostate structure, tumour and capsule. Importantly, it is recommended to wait 3 months after prostate biopsies before performing MRI of the prostate (for local staging purposes) as biopsy induces artefacts.
MRI findings in extracapsular extension include a focal irregular capsular bulge, asymmetry or invasion of neurovascular bundles, and obliteration of rectoprostatic angle [76]. The sensitivity of MRI for SV involvement is unfortunately extremely variable (from 20 to 80 %) whereas its specificity is much better, over 80 %.
Bone Scan
Serum PSA levels can predict the results of radionuclide bone scan in newly diagnosed patients. In patients with a PSA of <20 ng/ml and no bony pain, the likely chance of bony metastasis is less than 0.3 %. In 853 consecutive patients diagnosed with prostate cancer between 2003 and 2008 at a single centre who all underwent bone scan using technetium Tc at diagnosis, results confirmed that staging bone scans might be considered only for patients with a biopsy Gleason Score >7 or with a PSA >10 ng/ml and palpable disease (cT2/T3) prior to treatment [77].
PET/CT
Molecular imaging techniques, such as positron emission tomography (PET), may be of help in prostate cancer management and staging. PET can be combined with CT (PET/CT) to produce high-resolution images. Positron emission tomography, a functional imaging test uses a small amount of radioactive material to reveal how tissues and organs are functioning. The most commonly used PET tracer, Fluorodeoxyglucose presents limitations in imaging prostate cancer patients because most prostate cancers are not very 18 F-FDG avid, therefore, several alternative PET tracers either Choline (11C) or Citrate have been proposed to evaluate by PET these patients, with promising results.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







