Chapter 12 Clinical investigation of hepatopancreaticobiliary disease
Clinical History and Physical Examination
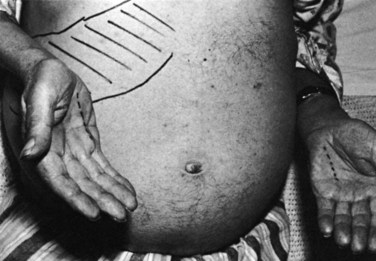
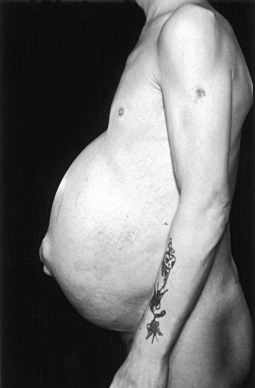
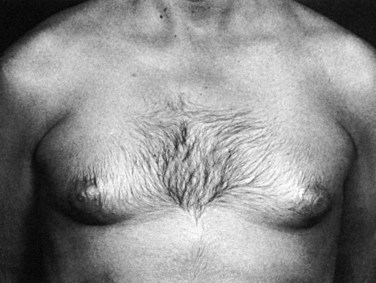
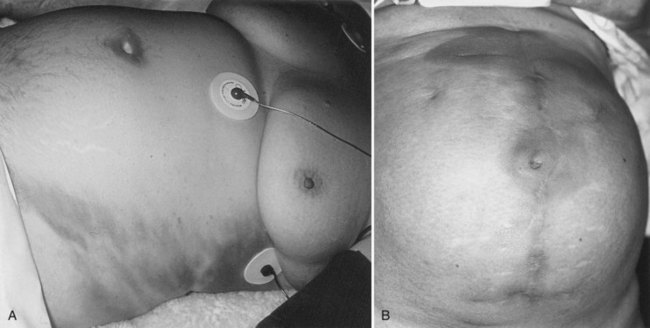
Examination should assess the presence or absence of the stigmata of chronic liver and biliary disease (see Chapter 7), including jaundice, pruritus, spider nevi (Fig. 12.1), hepatosplenomegaly (Fig. 12.2), ascites (Fig. 12.3), and caput medusae. Abnormal abdominal masses should also be noted. The circulation in patients with liver failure is hyperdynamic with flushed extremities and a bounding pulse, and peripheral cyanosis may be evident. Fetor hepaticus—a sweet, musty odor of the breath—is associated with hepatocellular failure and is thought to be related to changes in the gut flora (Challenger & Walsh, 1995). Spider nevi are angiomata that occur in the vasculature of the superior vena cava, and their disappearance and reappearance vary with liver function and are thought to be associated with estrogen excess (Bean, 1959). Palmar erythema (Fig. 12.4) affects the thenar and hypothenar eminences and is associated with the hyperdynamic state. Other changes include loss of axillary and pubic hair and whitening of the nails (Lloyd & Williams, 1948). Gynecomastia (Fig. 12.5) and testicular atrophy can also occur.
Chronic encephalopathy associated with portal hypertension and portosystemic shunting varies in severity, producing symptoms that range from mild confusion and a shortened attention span to marked intellectual deterioration that may end in coma. Psychomotor tests have been devised to quantify the intellectual deterioration and allow monitoring (Sherlock & Dooley, 2002). A flapping tremor of the extended wrist (“liver flap”) and later cogwheel rigidity and ankle clonus may be present. Acute liver failure is associated with jaundice, confusion, delirium, and renal failure. These features may occur on a background of cirrhosis, and the precipitating cause may be treatable (e.g., infection).
Patients also may be seen with acute abdominal pain or jaundice. Examination may reveal localized peritonism in the right upper quadrant or epigastrium with a tender mass or generalized peritonitis in cases of gallbladder perforation or severe pancreatitis. A Murphy sign is a “catch” in the breath elicited by gently pressing on the right upper quadrant and asking the patient to take a deep breath. A Boas sign is hyperesthesia of the skin over the lower right ribs posteriorly. One or both of these signs may be found in acute cholecystitis. Erythema ab igne is caused by prolonged local application of heat and may be evident in the right upper quadrant in patients with chronic gallbladder disease or, more commonly, on the back in patients with chronic pancreatitis (Fig. 12.6). In Asia, bleeding from a ruptured hepatocellular carcinoma is a common acute presentation. Patients with severe acute pancreatitis may develop a bluish discoloration of the flanks as a result of retroperitoneal bleeding (Turner sign) or in the periumbilical area (Cullen sign; Fig. 12.7).
Examination of the Liver
The liver is examined using a combination of palpation and percussion from above and below to delineate its borders. Dullness to percussion of the upper border extends as far as the fifth intercostal space. Auscultation is also important, because a venous hum may be heard with portal hypertension, and a bruit may be heard in association with hepatocellular carcinomas. The normal liver is usually impalpable; however, in asthenic individuals, the anterior edge may be palpable. Enlargement of the liver occurs in many pathologic states, although a tonguelike extension from the right lobe—a Riedel lobe, which is of no pathologic significance—may be mistaken for a tumor (Fig. 12.8). Causes of hepatomegaly are listed in Table 12.1. A lobe may undergo hypertrophy and become palpable, and this may occur in the presence of liver atrophy or after liver resection. Reduction in liver size also is important, because this may occur in cirrhosis and certain types of hepatitis. Consistency also is relevant; a hard, knobbly liver often represents the presence of metastases, whereas smooth enlargement may be due to cirrhosis.
Table 12.1 Causes of Hepatomegaly
| Variant Anatomy |
| Inflammatory |
| Metabolic |
| Hematologic |
| Tumors |
| Cardiovascular |
Examination of the Spleen
Examination of the spleen should begin in the right iliac fossa and proceed toward the left subcostal region, because this is the direction in which splenomegaly occurs. Rotation of the patient 45 degrees to the right may aid palpation, because the spleen then falls onto the examining right hand. During this maneuver, the left hand should support the rib cage and relax the skin and abdominal musculature by drawing these down to the right. Percussion may be useful, and if ascites is present, the spleen may be ballotable. If the spleen is sufficiently enlarged, the notch on its anterior border may become palpable. Causes of splenomegaly are listed in Table 12.2.
Table 12.2 Causes of Splenomegaly
| Infection |
| Hematologic |
| Neoplastic |
| Inflammatory |
Signs of Portal Hypertension
Portal hypertension (see Chapter 70A, 74 ) is due to either intrahepatic or extrahepatic portal venous obstruction. Intrahepatic portal hypertension usually is associated with hepatomegaly and may be accompanied by splenomegaly and ascites. Dilated abdominal wall veins also may be found secondary to portosystemic anastomosis, giving rise to a caput medusae. The more common clinical site of portosystemic anastomosis is at the gastroesophageal junction, leading to esophageal varices; any evidence of upper gastrointestinal blood loss, whether hematemesis or melena, should be investigated with urgent endoscopy (see Chapter 75A). Rarely, these patients may develop hemorrhoidal varices around the anus as a result of portosystemic anastomosis.
Clinical Features of Other Types of Liver Disease
Ulcerative Colitis and Crohn Disease
Ulcerative colitis and Crohn disease are associated with hepatobiliary disorders, especially primary sclerosing cholangitis (see Chapter 41). It is important to include a detailed gastrointestinal systems review and investigations in any patient with unexplained liver disease.
Budd-Chiari Syndrome
This syndrome is characterized by venous outflow obstruction to the liver, which could be intrahepatic or extrahepatic (see Chapter 77). Acute venous obstruction is usually secondary to another pathologic process and presents with abdominal pain, vomiting, hepatomegaly, ascites, and jaundice, which may be mild. Hepatocellular failure leading to death is usually rapid. Chronic venous obstruction of the liver usually presents with ascites and hepatomegaly. If the inferior vena cava (IVC) is blocked with tumor or thrombus, gross edema of the legs and superficial venous distension of the abdominal veins is apparent. Diagnosis is made on imaging.
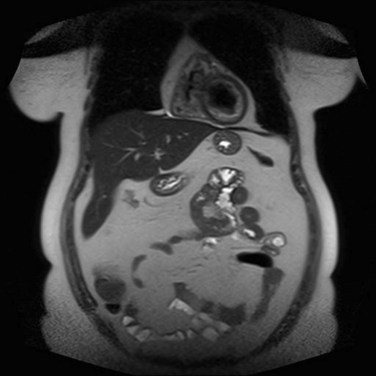
Polycystic Disease
Symptoms of polycystic disease are usually caused by the mass effect of the enlarged liver (see Chapter 69A). Abdominal distention and breathlessness are common. Early satiety and vomiting can occur because of pressure on the stomach. Acute abdominal pain is usually due to infection or bleeding into a cyst.
Acute Liver Failure
Acute liver failure (ALF) is characterized by massive cellular injury to a previously healthy liver, and it is associated with the development of hepatic encephalopathy (see Chapter 72). This can occur as a result of paracetamol (acetaminophen) toxicity, usually caused by overdosage, or from a massive viral infection. ALF is associated with a high mortality and requires careful monitoring. Orthotopic liver transplantation is the only effective treatment for this condition, although some cases of ALF can recover spontaneously. Donor organ shortage has dictated the development of criteria that can help to predict whether a patient with ALF has a potential to recover or whether a liver transplant is required. More recently, these criteria have also been used to predict the prognosis of patients with cirrhosis undergoing surgery for hepatocellular carcinoma (Kuang et al, 2009). Various sets of criteria have been proposed, of which the Model for End-Stage Liver Disease (MELD) and the King’s College Hospital (KCH) criteria are the best known. Most criteria utilize prothrombin time/INR, serum bilirubin, serum creatinine, arterial blood pH, and hepatic encephalopathy in categorizing patients’ disease severity.
Liver Masses
Patients with large liver masses may be seen initially with right upper quadrant discomfort or a palpable mass in the upper abdomen. More often, liver masses are discovered during imaging as part of the investigation of jaundice, nonspecific abdominal symptoms, or follow-up of malignancy. If the liver mass is discovered incidentally, a full clinical history should be obtained with particular attention to gastrointestinal and respiratory symptoms. Details and duration of oral contraceptive and anabolic steroid use should be recorded. Relevant past history, especially of other malignancies, should be obtained, and the possibility of viral hepatitis should be considered. A thorough abdominal examination should be performed, especially for abnormal masses and ascites, and a digital rectal examination is mandatory at the initial assessment. Signs of jaundice, liver insufficiency, and development of collateral circulation should be sought. A comprehensive hematologic and biochemical screening (Table 12.3) should include an assessment of coagulation factors and of common tumor markers (α-fetoprotein, carcinoembryonic antigen (CEA), CA 19-9, CA 125). Cross-sectional imaging evaluation of liver masses is discussed later in this chapter (see Investigation of Hepatobiliary Disease; see also Chapters 16 and 17).
Table 12.3 Laboratory Investigations in Hepatopancreatobiliary Disease
| Hematologic Tests |
| Liver Function Tests |
| Immunologic and Serologic Tests |
| Tumor Markers |
| Other Tests |