TECHNIQUES
TRANSARTERIAL CHEMOEMBOLIZATION
Superior Mesenteric Arteriogram with Venous Phase Imaging
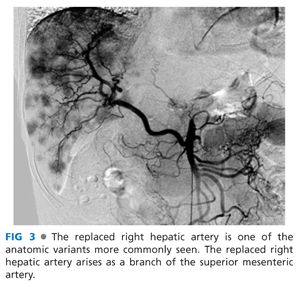
■ A 4- or 5-Fr catheter is used to selectively catheterize the superior mesenteric artery (SMA). The arterial phase (FIG 2) is inspected for anatomic variants such as a replaced right hepatic artery (FIG 3) or other anatomic variants. The potential for “parasitized” blood flow recruited from the SMA to the liver must also be assessed.

■ The venous phase (FIG 4) is inspected to evaluate patency of the portal vein and to evaluate for hepatofugal flow. TACE can be performed in cirrhotic patients with hepatofugal portal flow, but a smaller volume of liver should be embolized each time.

Celiac and Common Hepatic Arteriograms
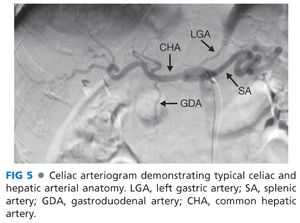
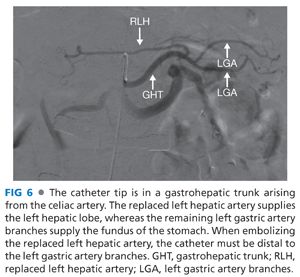
■ The 4- or 5-Fr catheter is used to selectively catheterize these vessels. The arteriograms (FIG 5) are evaluated for anatomic variants such as a replaced or accessory left hepatic artery arising from a gastrohepatic trunk (FIG 6) and phrenic arteries, which may arise at the origin of the celiac.
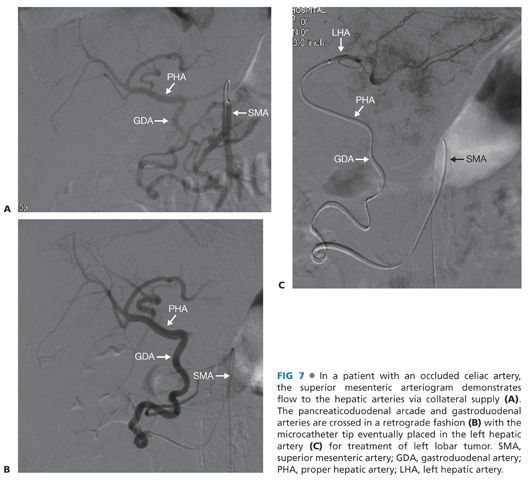
■ If the celiac artery is occluded, the occlusion can often be crossed and possibly stented to allow access or the procedure may be performed from the superior mesenteric artery in a retrograde approach via the pancreaticoduodenal arcade (FIG 7).
■ Evaluate where the arterial supply to the tumors is arising. Try to limit embolization of branches that do not supply the tumors.
Advancement of the Catheter to Point of Embolization
■ Commonly, this will be performed using a coaxial microcatheter.
■ Advance the catheter as selectively as possible; however, a lobar embolization may be required if the tumors are scattered throughout the liver.
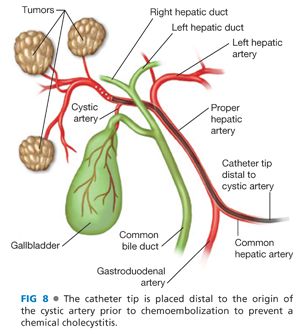
■ In patients with intact gallbladders, evaluate where the cystic artery originates (FIG 8). Ideally, embolization should be performed distal to the cystic artery. Treatment proximal to the cystic artery can cause a chemical cholecystitis with a more severe postembolization syndrome.
■ Arteriogram to evaluate selective cannulation of the feeding vessel(s) and to assess for arteriovenous shunting
Embolization Using the Embolic Material
■ Oily chemoembolization
■ Ethiodol is a poppy seed oil-based contrast. The Ethiodol vehicle is mixed, most commonly with a combination of cisplatin, doxorubicin, and mitomycin-C. The Ethiodol acts as a carrier and the chemotherapy is released slowly from the mixture. The Ethiodol is retained within the tumor and the neovasculature of the tumor (FIG 9). This is followed by particulate embolization of the target vessels.

■ Drug-eluting microspheres
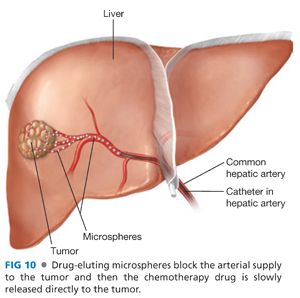
■ LC beads are a polyvinyl alcohol-based microsphere and QuadraSpheres are a copolymer microsphere.
■ 50 to 75 mg of doxorubicin is loaded into each vial of microspheres with a maximum of two vials being used per procedure. 100 to 300 micron LC beads™ and 50 to 100 micron QuadraSpheres™ are commonly used. The particles are then injected (FIG 10) until there is significant slowing of flow within the target vessels.
■ Irinotecan has been used, instead of doxorubicin, in treating patients with colorectal cancer that has metastasized to the liver.
■ Transarterial embolization (TAE), also known as bland embolization, has also been performed. TAE uses Ethiodol embolization, particulate embolization, or a combination of both without the addition of any chemotherapeutic agent.
Removal of the Catheters and Sheath
■ The puncture site is closed using manual pressure or an arterial closure device.
Follow-up
■ Labs in about 4 weeks to evaluate liver function
■ Repeat imaging if needed.
■ Repeat embolization, if needed, in about 4 to 6 weeks.
RADIOEMBOLIZATION
Sir-Spheres™ or TheraSphere™
■ 90Y binds to particles that are less than 35 microns in size. Sir-Spheres™ are resin-based particles, whereas the TheraSphere™ particles are nonbiodegradable glass microspheres.
Superior Mesenteric, Celiac, and Common Hepatic Arteriograms
■ The initial steps are similar to TACE. The arteriograms are evaluated for vessel patency and anatomic variants.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








