Cancers of the Biliary Tree: Anatomy and Staging
Attila Nakeeb
Henry A. Pitt
Biliary tract cancers affect more than 7,500 Americans each year, with an incidence of 4 cases per 100,000 residents in the United States. Biliary malignancies are composed of cancers of the bile ducts (cholangiocarcinomas) and gallbladder cancers. Cholangiocarcinomas are further subdivided by anatomic location into (i) intrahepatic, (ii) perihilar, and (iii) distal tumors (1). Biliary malignancies are often asymptomatic until late in the course of the disease. As a result, these tumors often present in an advanced stage. A margin-negative (R0) surgical resection provides the only opportunity for long-term survival. Both the late diagnosis and the complex operative techniques required for potentially curative resection contribute to the challenge of managing patients with biliary malignancies. A thorough understanding of hepatobiliary anatomy and both clinical and pathological tumor staging are essential for determining the most appropriate treatment for patients with biliary malignancies.
Hepatic Anatomy
A precise knowledge of the anatomy of the liver and biliary tract and of their relationship to associated blood vessels is essential for the performance of safe hepatobiliary surgery. Surgeons must have a complete understanding of the general anatomy of the liver, biliary tree, portal veins, and hepatic arteries. In addition, a detailed understanding of each individual patient’s anatomy is necessary because anatomic variants in the liver vasculature and biliary tree are common (2).
Segmental Anatomy
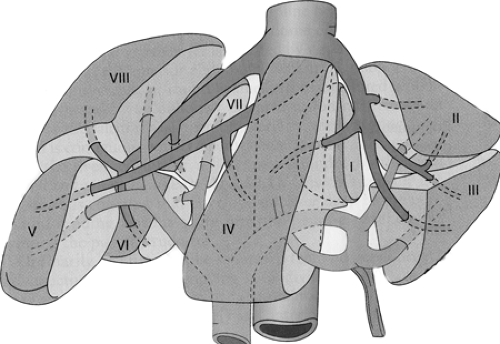
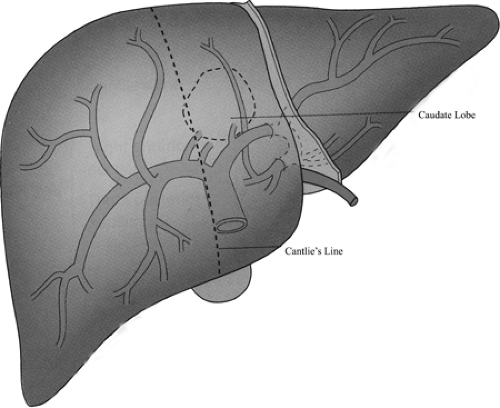
The most widely accepted nomenclature is based on Couinaud’s description of the discrete anatomic segments of the liver (Fig. 36.1). The eight segments of a liver can be determined using surface anatomy and location of the three main hepatic veins, the portal pedicle bifurcation into right and left, and the umbilical fissure and falciform ligament. The right and left halves of the liver are delineated by a plane through the middle hepatic vein and the inferior vena cava (IVC). Segments II, III, and IV lie to the left of this plane and form the left half of the liver. Segments V, VI, VII, and VIII lie to the right of this plane and form the right half of the liver. Segment I, or the caudate lobe, is morphologically distinct from the two halves of the liver and emanates from a process of liver lying posterior to the portal pedicle and anterior to the IVC. Whereas the right and left halves of the liver derive their blood supply from the corresponding right and left portal veins and hepatic arteries, segment I derives its blood supply from both. Additionally, the right half of the liver has venous drainage through the right and middle hepatic veins, and the left half of the liver through the left and middle hepatic veins. Segment I, however, drains directly via small branches into the IVC.
The right half of the liver can be further subdivided using a plane through the right hepatic vein and the IVC. Liver anterior to this plane forms its right anterior section, and liver posterior to this plane forms the right posterior section. The right anterior section of the liver comprises segment V (inferior to the portal bifurcation) and segment VIII (superior to the portal bifurcation). The right posterior section of the liver comprises segment VI (inferior to the portal bifurcation) and segment VII (superior to the portal bifurcation). The left half of the liver can be further subdivided using a plane through the umbilical fissure and falciform ligament. Liver medial to this plane forms the left medial section of the liver or segment IV, and liver lateral to this plane forms the left lateral section of the liver. The left lateral section of the liver is further subdivided into segment II (which is superior to the left hepatic vein) and segment III (which is inferior to the left hepatic vein).
Hepatic Veins
Three major hepatic veins carry blood from the liver to the IVC. Most patients have a single, large right hepatic vein that joins the right anterior wall of the IVC and a middle and left hepatic vein that converge into a common trunk 1 to 2 cm from the IVC and enter the left anterior wall of the IVC. In approximately one third of patients, the three main hepatic veins join the IVC via three distinct trunks. Usually, multiple accessory right hepatic veins empty from the right half of the liver directly into the IVC as it courses posterior to the liver.
Portal Veins
The superior mesenteric and splenic veins join posterior to the neck of the pancreas to form the main portal vein. It receives pyloric and coronary vein branches as it courses cephalad and obliquely to the right to form the most posterior structure within the hepatoduodenal ligament (portal triad). In the hilus of the liver, the main portal vein bifurcates into a short oblique right portal vein and a longer, more transverse, and more superficial left portal vein (Fig. 36.2). These branches then enter the parenchyma and become invested along with the other components of the portal triad by extensions of Glisson’s capsule. Both the right and left portal veins give off small branches to dually supply segment I. The right portal vein usually enters the hepatic parenchyma immediately and is quick to divide into a right anterior portal vein supplying segments V and VIII and a right posterior portal vein supplying segments VI and VII. The left portal vein may remain near the surface of the left half of the liver in the hilar plate for a significant distance as it courses
to the umbilical fissure to give off medial branches to segment IV and lateral branches to segments II and III.
to the umbilical fissure to give off medial branches to segment IV and lateral branches to segments II and III.
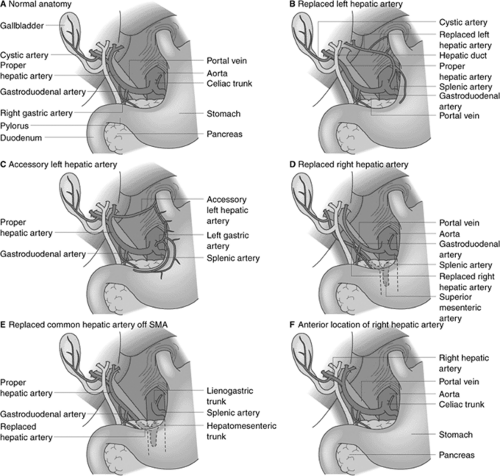
Hepatic Arteries
There is much variability in the hepatic arterial supply to the liver. The most common anatomy (Fig. 36.3) is a common hepatic artery that arises from the celiac trunk and courses near the superior border of the neck of the pancreas. After the origins of the gastroduodenal and right gastric arteries, the proper hepatic artery courses in the hepatoduodenal ligament in front of the portal vein and to the left of the common hepatic duct. The proper hepatic artery usually bifurcates into right and left hepatic arteries outside the liver. The right hepatic artery usually courses posterior to the common hepatic duct but anterior to the right portal vein to supply the right liver. The left hepatic artery usually remains extrahepatic until near the base of the umbilical fissure, where it enters the liver to give off branches to segments II, III, and IV. Classical hepatic arterial anatomy is found in only approximately 50% to 60% of patients. A replaced or accessory right hepatic artery may arise off of the superior mesenteric artery near its origin and course posteriorly or through the head of the pancreas to lie along the right posterior border of the hepatoduodenal ligament. A replaced or accessory left hepatic artery may arise off of the left gastric artery and course transversely toward the base of the umbilical fissure in the lesser omentum. In general, within the hepatic parenchyma, the hepatic arterial branches course closely with bile duct branches and fairly closely with portal venous branches.
Biliary Tree
Intrahepatic Bile Ducts
The right and left livers are drained by the right and left hepatic ducts, respectively, whereas the caudate (Segment I) is drained by several small ducts joining the bifurcation and the first several centimeters of both hepatic ducts. The intrahepatic ducts are tributaries of the corresponding hepatic ducts, which penetrate the liver invaginating Glisson’s capsule at the hilus (Fig. 36.4). Bile ducts are usually located above the corresponding portal branches, whereas hepatic arterial branches run inferiorly to the veins. The left hepatic duct directly drains the bile ducts to segments II, III, and IV, which constitute the left liver. The right hepatic duct drains the bile ducts from segments V, VI, VII, and VIII, which constitute the right liver. Usually, the bile ducts from segments V and VIII join to first form the anterior sectoral duct, and the bile ducts from segments VI and VII join to first form the posterior sectoral duct prior to forming the right hepatic duct.
Gallbladder
The gallbladder is a reservoir for bile located on the undersurface of the liver at the confluence of the right and left halves of the liver. It is separated from the hepatic parenchyma by a cystic plate, which is composed of connective tissue applied to Glisson’s capsule. The gallbladder may be deeply imbedded into the liver or occasionally presents on a mesenteric attachment, but usually lies in a gallbladder fossa. The gallbladder varies in size and consists of a fundus, a body, and an infundibulum. The tip of the fundus usually reaches the free edge of the liver and is closely applied to the cystic plate. The infundibulum of the gallbladder makes an angle with the body and may obscure the common hepatic duct constituting a danger point during cholecystectomy. The cystic duct arises from the infundibulum of the gallbladder and extends to join the common hepatic duct. The lumen measures between 1 and 3 mm in diameter, and its length varies depending on the type of union with the common hepatic duct. Calot’s triangle is bounded by the common hepatic duct on the left, the cystic duct inferiorly, and the cystic artery superiorly. Arterial blood reaches the gallbladder via the cystic artery, which usually originates from the right hepatic artery. The cystic artery may also originate from the left hepatic, common hepatic, gastroduodenal, or superior mesenteric artery. The cystic artery is usually located parallel and medial to the cystic duct, but its course varies with its origin. The cystic artery divides into superficial and deep branches before entering the gallbladder. The venous drainage of the gallbladder is directly into the liver parenchyma or into the common bile duct plexus. Lymphatic drainage from the gallbladder occurs in a predictable fashion and correlates with the pattern of lymph node metastases seen in gallbladder cancer. Lymph flow from the gallbladder initially drains to the cystic duct node and then descends along the common bile duct to pericholedochal lymph nodes. Flow then proceeds to nodes posterior to the head of the pancreas and then to interaortocaval lymph nodes. Secondary routes of lymphatic drainage include the retroportal and right celiac lymph nodes.
Common Bile Duct
The cystic and common hepatic ducts join to form the common bile duct. The common bile duct is
approximately 8 to 10 cm in length and 0.4 to 0.8 cm in diameter. The common bile duct can be divided into three anatomic segments: supraduodenal, retroduodenal, and intrapancreatic. The supraduodenal segment resides in the hepatoduodenal ligament lateral to the hepatic artery and anterior to the portal vein. The course of the retroduodenal segment is posterior to the first portion of the duodenum, anterior to the IVC, and lateral to the portal vein. The pancreatic portion of the duct lies within a tunnel or groove on the posterior aspect of the pancreas. The common bile duct then enters the medial wall of the duodenum, courses tangentially through the submucosal layer for 1 to 2 cm, and terminates in the major papilla in the second portion of the duodenum (Fig. 36.4). The distal portion of the duct is encircled by smooth muscle that forms the sphincter of Oddi. The common bile duct may enter the duodenum directly (25%) or join the pancreatic duct (75%) to form a common channel, termed the ampulla of Vater.
approximately 8 to 10 cm in length and 0.4 to 0.8 cm in diameter. The common bile duct can be divided into three anatomic segments: supraduodenal, retroduodenal, and intrapancreatic. The supraduodenal segment resides in the hepatoduodenal ligament lateral to the hepatic artery and anterior to the portal vein. The course of the retroduodenal segment is posterior to the first portion of the duodenum, anterior to the IVC, and lateral to the portal vein. The pancreatic portion of the duct lies within a tunnel or groove on the posterior aspect of the pancreas. The common bile duct then enters the medial wall of the duodenum, courses tangentially through the submucosal layer for 1 to 2 cm, and terminates in the major papilla in the second portion of the duodenum (Fig. 36.4). The distal portion of the duct is encircled by smooth muscle that forms the sphincter of Oddi. The common bile duct may enter the duodenum directly (25%) or join the pancreatic duct (75%) to form a common channel, termed the ampulla of Vater.
The blood supply of the common bile duct is segmental in nature and consists of branches from the cystic, hepatic, and gastroduodenal arteries. These meet to form collateral vessels that run in the 3 and 9 o’clock positions. The venous drainage forms a plexus on the anterior surface of the common bile duct that enters the portal system. The lymphatic drainage follows the course of the hepatic artery to the celiac nodes.
Clinicopathologic Staging of Gallbladder Cancer
Gallbladder cancer most often presents with right upper quadrant abdominal pain often mimicking other more common biliary and nonbiliary disorders. Weight loss, jaundice, and an abdominal mass are less common symptoms. Unfortunately, the nonspecific nature of these symptoms often leads to a delay in the diagnosis. Specific symptoms usually develop only after invasion or obstruction of nearby structures has occurred.
Pathologic Staging
Accurate pathologic staging of biliary malignancies is important for providing prognostic information to patients and for comparing the results of various therapeutic trials. The American Joint Committee on Cancer (AJCC) staging for gallbladder cancer is shown in Table 36.1 (3). This system, based on the TNM classification, takes into account the extent of the primary tumor (T), the presence or absence of regional lymph node involvement (N), and the presence or absence of distant metastatic disease (M).
Only 10% of gallbladder cancers are confined to the gallbladder wall at diagnosis, with liver involvement found in 59%, lymph node involvement in 45%, infiltration of the common hepatic duct in 35%, perineural involvement in 42%, and involvement of other organs in 45% of patients. Hepatic and other hematogenous metastases were detected in 34% and 20% of patients, respectively (4).
The appropriate management and overall prognosis for gallbladder cancer are strongly dependent on tumor stage and are discussed in detail in the following chapter. For stage I tumors, simple cholecystectomy may be the only treatment that is required. Unfortunately, tumors that are limited to the gallbladder’s mucosa represent only about 5% of all gallbladder cancers. Stage II tumors require an “extended cholecystectomy,” which includes segmental resection of the adjacent liver bed
and a regional lymph node dissection including all periportal, retropancreatic, and celiac lymph nodes. For stage II tumors, which represent approximately 10% of gallbladder cancers, an extended cholecystectomy may improve survival from 30% to 40% with simple cholecystectomy to 70% to 85% with the more aggressive approach (5,6,7,8,9,10,11,12). This major improvement in survival with extended cholecystectomy is achieved with minimal morbidity and a low mortality. Stage III and IV patients are not considered resectable and are treated with chemotherapy and/or radiation therapy.
and a regional lymph node dissection including all periportal, retropancreatic, and celiac lymph nodes. For stage II tumors, which represent approximately 10% of gallbladder cancers, an extended cholecystectomy may improve survival from 30% to 40% with simple cholecystectomy to 70% to 85% with the more aggressive approach (5,6,7,8,9,10,11,12). This major improvement in survival with extended cholecystectomy is achieved with minimal morbidity and a low mortality. Stage III and IV patients are not considered resectable and are treated with chemotherapy and/or radiation therapy.
Radiologic Evaluation
Ultrasound, computed tomography (CT), and magnetic resonance (MR) can all be used in the diagnosis of gallbladder cancer. Their techniques are reviewed in more detail in the following chapter but are briefly summarized here. Any of these techniques can be used to demonstrate replacement of the gallbladder by tumor; invasion into the liver or adjacent structures such as the colon, duodenum, or extrahepatic bile ducts; and involvement of the hepatic arteries or portal veins.
Initial assessment of patients with biliary tract symptoms often includes a right upper quadrant ultrasound. Early carcinoma may present as a fixed mass not associated with acoustic shadowing or a complex mass filling the lumen with localized thickening of the gallbladder wall. Often, it is difficult to differentiate between cholecystitis and early carcinoma because thickening of the gallbladder wall is a feature of both diseases (13). If the tumor is advanced, ultrasonography shows a loss of the interface between the gallbladder and liver. This feature is indicative of tumor invasion. Ultrasound can reveal other associated signs such as the presence of cholelithiasis, porcelain gallbladder, invasion of neighboring structures or hepatic metastases, vascular invasion, biliary dilatation, adenopathies, and ascites (14). In advanced stages of the disease, when most patients are diagnosed, ultrasound has a sensitivity of 85% and an accuracy of 80% for the diagnosis of gallbladder cancer (15), but it has limitations in the diagnosis of involved lymph nodes and staging of disease (16). With the recent advent of color doppler ultrasonography, it is now possible to differentiate between biliary sludge and carcinoma by studying fine vessel patterns (17). Endoscopic ultrasonography (EUS) has also been used for diagnostic evaluation. This technique, which may greatly improve the diagnosis of gallbladder carcinoma, can better predict the depth of tumor involvement and can be combined with fine needle aspiration (FNA) biopsy (15,18).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree