Hepatocellular Cancer: Pathology
Gregory Y. Lauwers
Vikram Deshpande
An increasing incidence of hepatocellular carcinoma (HCC) in Western countries, secondary to HCV hepatitis and other factors, including obesity, has been paralleled by advances in hepatic imaging and surgery. Detected either during monitoring of patients at risk or secondary to symptoms, the resection of an increased number of cases has resulted in an abundance of pathological material. Consequently, over the past few years, there has been a steady stream of information related to the histologic characteristics of HCCs, their pattern of spread, the risk factors for recurrence, and long-term prognosis. Another growing field has been related to the diagnosis of early HCC. Understanding by histopathologists, surgeons, hepatologists, and oncologists of the nuances of the diagnosis of early HCC, as well as the importance of detailed pathological analysis of a hepatectomy specimen, is crucial to developing an appropriate therapeutic algorithm.
Macroscopic Features of Hepatocellular Carcinoma
Despite early reports to the contrary, the gross morphologic characteristics in HCC do not seem to be affected by the geographic origins of the patients (1,2,3). Essentially, variations in the morphologic appearance of HCC depend on the size of the tumor and the quality of the surrounding liver, namely, the presence or absence of cirrhosis. Western series have emphasized that between 42% and 51% of HCCs arise in noncirrhotic livers (4,5). However, some of the “noncirrhotic” cases may be better characterized as being associated with limited fibrosis.
Differences in the multiplicity of tumors, incidence of encapsulation, and rate of venous invasion have been reported in these tumors. Also, HCCs in noncirrhotic livers grow faster and are larger than those in cirrhotic livers (6,7).
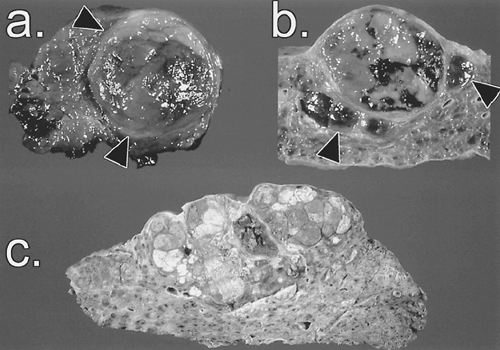
In cirrhotic livers, small HCCs are usually well demarcated and surrounded by a fibrous capsule, whereas advanced tumors are expansive multinodular masses, frequently accompanied by intrahepatic metastases (8). Conversely, HCCs arising in noncirrhotic livers tend to present as single large massive tumors that may infiltrate both lobes (5,6).
The size of HCCs is an important risk factor for intrahepatic and extrahepatic spread (9,10,11). Tumors measuring <5 cm are less likely to develop intrahepatic metastasis, portal vein tumor thrombosis, or hematogenous metastasis (9,11,12). However, the rate of intrahepatic metastasis rises dramatically (96% vs. 60% of cases) and the incidence of portal vein thrombosis almost doubles (75% vs. 40% of cases) when HCCs grow larger than 5 cm in size (9,10).
Irrespective of the pattern of growth, most HCCs are soft neoplasms often displaying hemorrhage and necrotic foci. Their color ranges from tan-gray to green, the intensity of the latter reflecting the degree of bile production (13). Presence of a capsule is a function of the tumor’s size and is found around 46% of HCCs measuring <2 cm in diameter, seen in 84% of tumors between 2 and 5 cm, and in only 45% of HCCs >5 cm in diameter (14). The presence of a capsule is an important characteristic because it is associated with improved survival, lower intrahepatic recurrence rate, and reduced incidence of local venous invasion (4,15). Whether tumor encapsulation is more frequent in patients without cirrhosis remains debated (2,4,16).
Macroscopic Classification
The growth pattern of HCCs has some importance because the different types are associated with various risks of intrahepatic and extrahepatic spread (9). The classification of Eggel, published a century ago and based on autopsy cases, is still widely used (17). In this scheme, HCCs are divided into three categories: nodular, massive, and diffuse types. The nodular type is composed of tumor nodules scattered within the cirrhotic parenchyma. The massive type consists of a circumscribed, huge tumor mass occupying most or all of a hepatic lobe. This type, commonly observed in patients without cirrhosis, arises frequently in the right lobe and can be surrounded by satellite nodules. The relatively rare diffuse type is characterized by innumerable indistinct small tumor nodules. However, nowadays, the smaller resected HCCs, do not readily fit into Eggel’s classification. This has led to the development of new classifications, none of them widely accepted (1,18). The most notable change is the one proposed by the Liver Cancer Study Group of Japan, by which the nodular type is divided into three categories: the single nodular type, the single nodular type with perinodular tumor growth, and the confluent multinodular type (13) (Fig. 31.1). Other classification schemes have included subtypes such as the small HCC (<2 cm) and the rare pedunculated HCC (19).
Other Significant Gross Features of Hepatocellular Carcinomas
Multicentricity of Hepatocellular Carcinoma
Multicentricity, an important predictor of late intrahepatic recurrence after hepatectomy, is noted in 16% to 74% of resected HCCs (9,14,20,21,22,23). These results, however, pertain essentially to patients with cirrhosis and contrast sharply with HCCs arising in noncirrhotic livers, in which the rate of
multifocal tumors is only 12% (6). Two mechanisms account for the multiplicity of HCCs: the metachronous development of tumors through the mechanism of multicentric carcinogenesis, and metastatic intrahepatic spread via the portal system (24,25). Lesions are considered metastatic in nature
multifocal tumors is only 12% (6). Two mechanisms account for the multiplicity of HCCs: the metachronous development of tumors through the mechanism of multicentric carcinogenesis, and metastatic intrahepatic spread via the portal system (24,25). Lesions are considered metastatic in nature
If they demonstrate a portal vein tumor thrombus or grow contiguously with a thrombus
If multiple small satellite lesions surround a larger main tumor
If a single tumor is present near the main tumor but is significantly smaller in size and exhibits the same histology (24)
Intravascular and Biliary Growth
Tumor thrombi in the portal vein system represent the source of intrahepatic metastases of HCC. Major portal vessel thrombosis portends a poor prognosis, with most such patients experiencing recurrence within 1 year and death within 2 years after the resection (12,26). Less frequently, tumor thrombi may form within hepatic veins, sometimes extending into the inferior vena cava and eventually the right atrium (27).
Tumor invasion into the hepatic duct, common bile duct, or both is rare but is associated with notably worse prognosis (19). It sometimes poses a preoperative diagnostic challenge, with most patients presenting with obstructive jaundice or hemobilia frequently and incorrectly diagnosed as having a cholangiocarcinoma or choledocholithiasis (28).
Microscopic Features of Hepatocellular Carcinoma
Neoplastic hepatocytes exhibit various degrees of hepatocellular differentiation. They are usually polygonal with abundant eosinophilic and granular cytoplasm surrounded by distinct cell membranes. Characteristically, the nucleus is round and vesicular with a distinct nucleolus. Various intracytoplasmic inclusions can be observed, including glycogen, fat, bile, fibrinogen (pale bodies), Mallory bodies (accumulation of keratin and p62 stress protein) and intracellular hyaline bodies (accumulations of p62 stress protein), alpha-fetoprotein (AFP), giant lysosomes, or α1-antitrypsin (29,30).
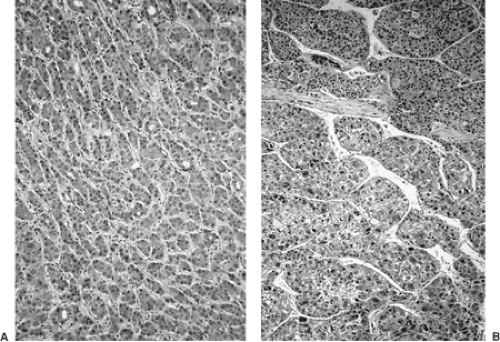
A trabecular arrangement mimicking normal hepatic cords is the basic architectural growth pattern of HCCs. However, the histologic appearance is variable, with several variations on this basic theme.
Histologic Patterns
The World Health Organization classification recognizes five major histologic patterns. Except for the fibrolamellar pattern, their significance is more of diagnostic value than indicative of prognosis (29). The four other subtypes, frequently found simultaneously, are trabecular, pseudoglandular (acinar), compact, and scirrhous.
The trabecular and pseudoglandular architectural patterns are commonly encountered in well to moderately differentiated HCCs. The trabeculae, which can vary widely in thickness from a few cells thick (microtrabecular) to more than a dozen cells (macrotrabecular), are separated by sinusoidlike spaces lined by flat endothelial cells (Fig. 31.2). In the acinar (or pseudoglandular) variant, the cells are arranged in a rosettelike fashion with a central bile canaliculus (Fig. 31.3). In the solid type, a variant of macrotrabecular architecture, the sinusoids are compressed and obscured by the broad and compact trabeculae. Finally, the scirrhous pattern is characterized by abundant fibrous stroma separating cords of tumor cells. This pattern is often seen as a secondary change after radiation, chemotherapy, or infarction. Various degrees of the scirrhous pattern are found without any previous treatment in approximately 4% of cases (13,29).
Histologic Grading of Hepatocellular Carcinomas
The most commonly used grading scheme, developed by Edmondson and Steiner in 1954, is a four-tier system based on the degree of differentiation of the neoplastic cells (31). Grade I is composed of well-differentiated neoplastic hepatocytes arranged in thin trabeculae. In such cases, distinguishing HCC from small cell dysplasia is frequently difficult, particularly in needle biopsy specimens (Fig. 31.4). In grade II, the cells are larger and more atypical, sometimes organized in an acinar pattern. In grade III, architectural and cytologic anaplasia is prominent, but the tumor is still readily identified as hepatocytic in origin (Fig. 31.4). In grade IV, the neoplastic cells are markedly anaplastic and not easily identified as hepatocytic origin.
An alternate four-tier histologic grading scheme is advocated by the Liver Cancer Study Group of Japan (13). In this system, well-differentiated HCCs, most measuring <2 cm in diameter, are characterized by increased cellular density with irregular microtrabeculae, focal acinar formation, and frequent fatty change (Fig. 31.4). Cellular and nuclear atypia are distinctly absent. This carcinoma would correspond to the grade I carcinoma of the Edmondson-Steiner classification. In moderately differentiated HCCs, atypical hepatocytes have a trabecular arrangement, but a pseudoglandular pattern can also be observed (Fig. 31.3). Cytologically, the neoplastic hepatocytes have abundant eosinophilic cytoplasm with round nuclei and distinct nucleoli. The nucleus-to-cytoplasm ratio is equal to that of the normal hepatocytes. This type corresponds to grade II and III carcinoma of the Edmondson-Steiner scheme and is common among advanced HCCs.
A solid growth pattern characterizes the poorly differentiated HCCs. The neoplastic hepatocytes have an increased
nucleus-to-cytoplasm ratio and show pleomorphism, including mononucleated or multinucleated giant cells, or both. This category corresponds to Edmondson-Steiner grades III to IV.
nucleus-to-cytoplasm ratio and show pleomorphism, including mononucleated or multinucleated giant cells, or both. This category corresponds to Edmondson-Steiner grades III to IV.
In undifferentiated HCCs, the cells are characterized by scant cytoplasm with short spindle-shaped or round nuclei and grow in a solid or medullary pattern. These correspond to grade IV carcinoma of the Edmondson-Steiner classification.
Although they are widely used, the prognostic value of these systems is debated. Some series report better prognosis for low-grade HCC, whereas others deny a correlation between poor prognosis and high histologic grade (4,32). Also, Edmondson-Steiner grading was not found to be a predictor of intrahepatic recurrence by some, whereas a high histologic grade has been estimated by others to be a strong predictor of portal vein invasion (15,33). Whether the presence of cirrhosis influences the histologic grade is also debated. According to one series, the odds of having a high-grade HCC is almost double for patients with a cirrhotic liver compared to that of patients without cirrhosis (4).
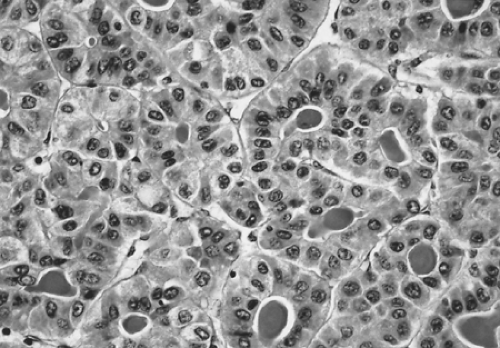 FIGURE 31.3. The pseudoglandular (acinar) pattern of hepatocellular carcinoma. The neoplastic hepatocytes are moderately atypical (grade II). Bile plugs are identified in the lumen. |
Cytologic Subtypes
The clear cell variant of HCC is composed of well to moderately differentiated tumor cells with a clear cytoplasm resulting from excessive intracytoplasmic deposits of glycogen (29). A tumor can be entirely of the clear cell type, or this variant may represent only a limited portion of an otherwise typical HCC. Its reportedly favorable prognosis has not been confirmed (34,35). In practice, clear cell HCC should be distinguished from metastatic clear cell variants of renal cell and adrenocortical carcinomas. In most cases, immunohistochemistry can provide the appropriate diagnosis.
Pleomorphic HCCs are characterized by marked variations in shape and size of the neoplastic hepatocytes and their nuclei. Seemingly benign giant cells (osteoclast type) or highly anaplastic bizarre cells can be observed (29). Spindle (or sarcomatoid) tumor cells are either focal or represent most of the tumor (29) (Fig. 31.5). Arterial chemotherapy has been implicated in this phenotypic transformation (27). The diagnosis of this variant can be challenging because it may resemble fibrosarcoma, leiomyosarcoma, and malignant fibrous histiocytoma. Distinction of this variant from a sarcoma is largely dependent on the identification of foci morphologically typical for HCCs. Cytokeratin (CK) immunoreactivity, although supportive of this variant, is not universally present, being reported in 62% of cases in one series (36).
Vascular Invasion
Because HCCs have a rich vascular stroma, microscopic portal vein or hepatic vein invasion can be expected to be a frequent finding. Even among candidates for liver transplantation (either single small HCCs of <5 cm or no more than three tumors all ≤3 cm), 33% of patients were shown to have microvascular invasion (37). Risk factors for portal vein invasion include tumor diameter >3 cm, high histologic grade, tumor multiplicity,
and mitotic rate >4 per 10 high-power fields (33,37). Whether venous invasion is more frequent in patients with cirrhosis than in those without is debated (4,33). Overall, it is an important prognostic indicator with patients with no vascular invasion experiencing a longer overall and diseasefree survival in part because intrahepatic metastases occur through portal vein invasion (23,32,38,39).
and mitotic rate >4 per 10 high-power fields (33,37). Whether venous invasion is more frequent in patients with cirrhosis than in those without is debated (4,33). Overall, it is an important prognostic indicator with patients with no vascular invasion experiencing a longer overall and diseasefree survival in part because intrahepatic metastases occur through portal vein invasion (23,32,38,39).
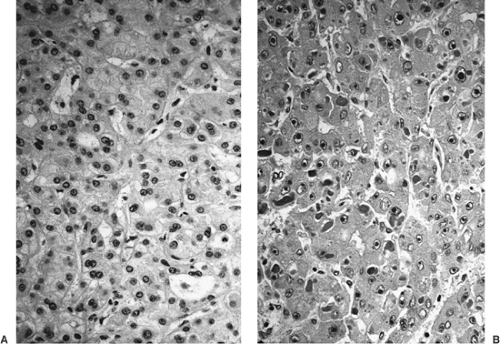 FIGURE 31.4. Cytologic subtypes of hepatocellular carcinoma. A: Grade I (well differentiated). The well-differentiated neoplastic hepatocytes show minimal cytologic and architectural atypia. Note the central acinar structure. B: Grade III (moderately differentiated). The tumor cells, arranged in ill-formed trabeculae, have large vesicular nuclei with prominent nucleoli.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|