Cancer of the Colon and Rectum
Lee D. Gorden
Todd M. Tuttle
Isaac Jones is a previously healthy 66-year-old man who arrives at the emergency department with a complaint of light-headedness when standing. He describes passing black tarry stools three to four times in the past week. He has lost nearly 20 pounds in the past 6 months. He does not smoke, and he drinks alcohol only occasionally. His only medication is ibuprofen for mild arthritis.
What are the distinctions among melena, hematochezia, bright red blood per rectum, and heme-positive when describing a patient’s stools?
View Answer
All of these terms describe bleeding from the gastrointestinal (GI) tract.
Melena: The passage of tarry, reddish-black stools
Hematochezia: Bloody stools
Bright red blood per rectum: Implies bleeding from a distal source or a massive hemorrhage from a proximal source
Heme-positive bleeding: Bleeding that is not grossly visible; however, stools test positive on hemoccult cards
The correct description of a patient’s stools may give important clues as to the source and rate of bleeding.
At the initial physical examination, Mr. Jones’ vital signs are as follows: blood pressure, 140/80 mm Hg; heart rate, 104 beats per minute; temperature, 37°C; respiratory rate, 12 breaths per minute. His chest is clear to auscultation bilaterally, and a mild, regular, tachycardia is revealed. The abdomen is soft, not tender, and not distended, with normal bowel sounds. The rectal examination is significant, with hemoccult-positive melanotic stool in the vault. His neurologic examination produces normal findings.
Laboratory studies show a normal electrolyte profile. The white blood cell count is 7.4 × 103 cells per mm3 (normal count, 4.5 to 11 cells per mm3), hemoglobin level is 8.1 g per dL (normal level, 14 to 18 g per dL), with a mean corpuscular volume (MCV) of 72 fL (normal range, 86 to 98 fL), and the platelet count is 240,000 per mL (normal count, 150,000 to 450,000 per mL). Liver function test findings are within normal limits.
Which conditions should be considered in the differential diagnosis of lower GI tract bleeding?
View Answer
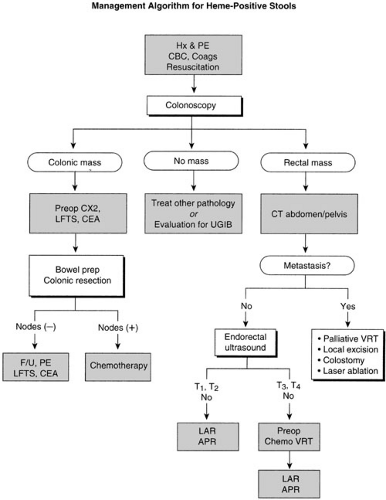
The most common causes of lower GI bleeding are, in order of decreasing frequency, diverticular disease, carcinoma of the colon, inflammatory bowel disease, colonic polyps, vascular ectasias, ischemic colitis, rectal ulcers, and hemorrhoids, together with several very rare disorders (1). Algorithm 14.1 outlines a management algorithm for the workup for heme-positive stools.
Mr. Jones is anemic, and the low MCV suggests that his blood loss results from a chronic, not an acute, process. He undergoes colonoscopy, which reveals a fungating mass proximal to the hepatic flexure. The lesion is not amenable to endoscopic removal, and surgery is recommended.
What types of tumors occur in the colon and rectum?
View Answer
Adenocarcinomas are the most common malignant colorectal tumors. Other malignant tumors are carcinoids, GI stromal tumors, primary lymphomas, and metastatic tumors originating from other organs (2). The most frequently encountered neoplasms are adenomas and adenomatous polyps (discussed later in this chapter).
How common is colorectal cancer?
View Answer
Cancer of the colon and rectum is the third most commonly diagnosed malignancy and the second leading cause of cancer deaths in men and women in the United States. In 2002, an estimated 107,300 new cases of colon cancer and 41,000 new rectal cancers occurred. An estimated 56,600 patients died in 2002 from colorectal cancer. Importantly, nearly 50% of patients diagnosed develop metastases within 5 years. However, mortality from colorectal cancer has decreased over the past several decades (3).
What are some important anatomic considerations of the blood supply to the colon and rectum?
View Answer
The arteries that supply the colon are paralleled by veins of the same names. The superior and inferior mesenteric veins join the splenic vein, which drains into the portal vein to the liver. Thorough review and knowledge of this anatomy is essential to a successful surgical resection.
The lymphatic drainage of the colon parallels the venous channels. Lymph nodes may be found in the colonic mesentery, the mesorectum, and the para-aortic area. Low-lying cancers of the anal canal may spread to the deep inguinal nodes, and tumors of the anus may spread to the superficial inguinal nodes.
How should individuals be screened for colorectal cancer?
View Answer
Average-risk, asymptomatic patients should undergo colorectal cancer screening at age 50. The most commonly used method is annual fecal occult blood test plus flexible sigmoidoscopy every 5 years. Colonoscopy can be performed every 5 to 10 years or double-contrast barium enema every 5 years. Virtual colonoscopy using computed tomography (CT) or other imaging modalities is not yet recommended (4, 5, 6).
What are the surgical options for the treatment of colon cancers?
View Answer
The surgical treatment of colon tumors depends on their location. For single lesions, a segmental resection is usually performed, whereas for synchronous lesions, a more extensive resection may be required. Standard surgical procedures according to the location of the tumor include right hemicolectomy, transverse colectomy, left hemicolectomy, and sigmoid colectomy, with the corresponding mesentery and mesenteric lymph nodes included in the resection. A surgical margin of at least 2 cm is desirable, both proximal and distal to the tumor (7).
Should laparoscopic resection be performed for colon cancer?
View Answer
Laparoscopic treatment for many nonmalignant diseases now is preferred over a traditional open operation. For laparoscopic-assisted colectomy, several small ports are introduced into the peritoneal cavity and pneumoperitoneum is established. Laparoscopic staging is performed, the colon is mobilized, and the vascular pedicle ligated and divided. The tumor-containing colon is then exteriorized through a small incision. Standard extracorporeal techniques are used to divide the colon and perform the anastomosis. Weeks et al. described the results of a multicenter prospective randomized trial comparing laparoscopic-assisted versus open colectomy for colon cancer. Only minimal short-term quality of life benefits were found in patients undergoing laparoscopic-assisted colectomy. Survival data from this study are not available (8,9).
The role of laparoscopic colectomy for colon cancer remains controversial and is continuing to be evaluated in trials. In the 2003 guideline, the National Comprehensive Cancer Network did not recommend laparoscopic colectomy.
Mr. Jones is scheduled to undergo a right hemicolectomy.
Is any additional diagnostic or staging information required before surgery?
View Answer
An appropriate preoperative staging evaluation for colon cancer patients includes chest radiograph, colonoscopy, complete blood count, platelet count, carcinoembryonic antigen (CEA) level, and pathology review. The routine use of abdominal-pelvic CT is controversial. For rectal cancer, abdominal-pelvic CT is useful because the finding of metastatic disease may alter treatment decisions. In addition, endorectal ultrasound (ERUS) should be performed on patients with rectal cancer.
The CEA level, an important tumor marker, should be established preoperatively so that subsequent levels can be monitored. Abnormal preoperative liver function tests in patients with colonic malignancy are of concern and may suggest metastatic disease in the liver.
In patients with rectal cancer, the most important step is preoperative determination of the stage of the patient’s disease. Again, history and physical examination, including a digital rectal examination and, for women, a pelvic examination, are very important. Patients with rectal tumors should undergo CT of the abdomen and pelvis.
ERUS is the most accurate method for staging local tumors. When performed by an experienced surgeon or radiologist, this procedure can disclose the depth of invasion with an accuracy of 85% to 90% and predict any nodal metastases with an accuracy of 85%. ERUS can help identify candidates for local therapy, patients who need radical surgery, and patients who would benefit from preoperative radiation therapy.
How should the bowel be prepared before colorectal surgery?
View Answer
Three principles direct preparation of the colon for surgery:
Mechanical preparation of the colon to cleanse it of stool
Intraluminal antibacterial treatment
Systemic antibiotic therapy. The addition of oral antibiotics to the standard mechanical bowel preparation reduces complications after colonic surgery by as much as 40%.
An accepted preoperative bowel preparation procedure is as follows:
The patient is maintained on a clear liquid diet for 24 hours before surgery.
A balanced electrolyte solution, such as GoLYTELY or magnesium citrate, is used for mechanical cleansing and lavage of the bowel until the output is clear. A tap water or phosphate enema is a possible addition.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree