Fig. 42.1
Visualization of sentinel nodes (SNs) and lymph ducts (LDs) by means of three-dimensional computed tomographic lymphography (3D-CT LG). Iopamidol is injected into the periareolar skin and the skin above the tumor. The 3D-CT LG procedure reveals the precise lymphatic flow from the tumor to the SN. In the case depicted here, the lymphatic flow from the tumor is branched to the periareolar direction and directly to the axilla. Lymph drains from the tumor, encircles the nipple, and travels to the lymph nodes of the axilla. A second duct carries lymph directly from the tumor to the axilla
3D-CT LG reveals the sentinel node within 1 min after contrast injection. By 3 min and 5 min after injection, the flow of dye beyond the sentinel node can be tracked to the second and third nodes toward the venous angle with the complex plexus [7, 8]. An example is shown in Figure 42.2, which reveals 5 bead-like grouped nodes beyond the sentinel node and the communicating lymphatic plexuses.
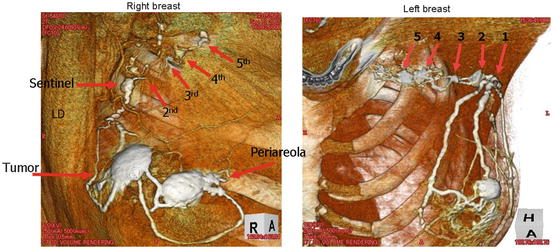
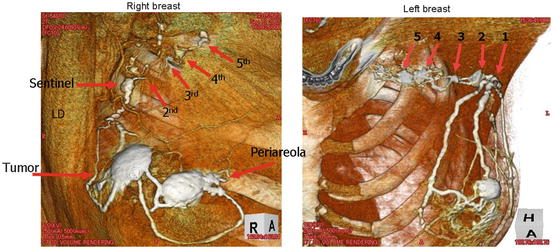
Fig. 42.2
Examination of a right and left breast by means of three-dimensional computed tomographic lymphography (3D-CT LG). Examination is performed chronologically 1, 3, and 5 min after iopamidol injection.Iopamidol flows into the sentinel node (SN) and then into successive nodes. Here, a string of five bead-like grouped lymph nodes is seen in the axilla after partial removal of the pectoral muscle. These successive nodes are thought to indicate the path of lymph metastasis. The arrows point to lymph nodes 1-5, which receive lymph from the SN
42.3.2 Endoscopic Sentinel Node Biopsy
Sentinel node biopsy is performed endoscopically by the dye-staining method. In the periareolar region and over the tumor, 2 mL of 1% indocyanine green is injected subcutaneously. After 20 min, a 1-cm incision is made along the skin cleavageline in the axilla, along the marks placed with the aid of 3D-CT LG. A Visiport optical trocar is inserted into the incision. The view is obtained through the Visiport with a 10-mm-diameter, rigid, oblique-viewing endoscope, and the stained lymph nodes are found by tracking the dye in the lymph ducts (Figure 42.3). The nodes are sampled, and the samples are sent out for intraoperative frozen section pathology.
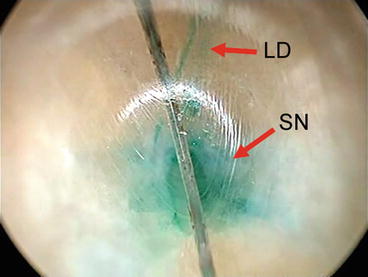
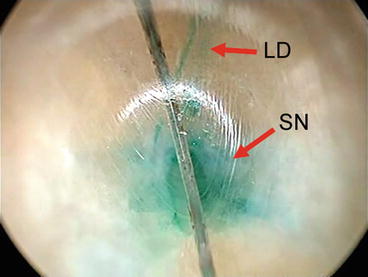
Fig. 42.3
Endoscopic view (through the Visiport) of the sentinel node (SN) and the draining lymph duct (LD). Both the SN and LD are stained green. The SN is found by tracking the flow of dye through the LD
42.4 VABS by TARM Approach
42.4.1 Skin Incision
Conventional endoscopic surgery for the breast is performed via skin incisions in the axilla and in the periareolar region. However, with the TARM approach, the skin incision is made in the axilla, horizontally about 2.5 cm along the natural skin fold. A LapProtector for the breast is inserted. The surgical margins are marked by injection of blue dye at 8 points.
42.4.2 Dissection Behind the Mammary Gland
First, the adipose tissue is cut deeply to the shallow lateral chest fascia, and the cut is extended to the lateral edge of the pectoral muscle. The pectoral muscle fascia is bluntly dissected beyond the back of the tumor by UltraRetractor vein harvest under video assistance. The penetrating vessels are cut and coagulated with a Harmonic Scalpel (Ethicon, Cincinnati, OH, USA) and electrocoagulator.
The mammary gland is lifted to create a retromammary space. 2-0 Vicryl sutures are placed in the gland via the skin, and attached to a lifting device, anchoring the mammary gland. The anchor point is 1 cm away from the cut margin. This step creates a large working space behind the mammary gland and facilitates vertical cutting of the gland.
The cut is initiated at the point marked at the proximal margin. The proximal margin is recognized by the blue dye markings as well as a straight needle inserted through the skin. The gland is cut vertically toward the skin, as illustrated in (Figure 42.4). The distance between the end of the cut and the skin above is easily evaluated by touching the patient’s skin.
Fig. 42.4
Diagram of the trans-axillary retro-mammary (TARM) approach (a) Frontal view of the surgical procedure. Arrows show the axillary skin incision, dissection route, and partial resection of the mammary gland, for breast cancer in the left caudal medial quadrant. (b) Cross-sectional view of the retro-mammary route. Arrows show the approach from the axillary skin incision, dissection of the major pectoral muscle fascia, upward cutting to subcutaneous tissue at the proximal surgical margin, and dissection of subcutaneous tissue over the tumor
42.4.3 Dissection of the Subcutaneous Tissue Overlying the Tumor
A skin flap over the tumor is made by the tunnel method. Many penetrating tunnels are created at 1-cm intervals in the subcutaneous tissue at a fixed depth with the use of an endodissector. Blood vessels collect in the septa between these tunnels, and the septa are cut with a Harmonic Scalpel (Ethicon). This minimizes blood loss.
42.4.4 Partial Excision of the Gland Along With the Tumor and Safety Margin
To excise the tumor with an adequate safety margin, the 8 dye-marked points are very important because we cannot touch the tumor directly. The gland is cut with a Harmonic Scalpel (Ethicon) or bipolar scissors to minimize blood loss. For a clear view, mist and smoke are evacuated with the suction probe. The resected part of the gland is pulled out through the axillary port in an Endo Catch specimen pouch (Covidien, New Haven, CT, USA). When the specimen is larger than the port, the wound can be widened or the gland cut into pieces within the pouch so that the pouch can be easily pulled out. After careful hemostasis and warm saline lavage, breast reconstruction is performed.
42.4.5 Breast Reconstruction
For breast reconstruction, we usually mobilize the mammary gland and fill the lateral defect with a skin flap. However, when there is a shortage of subcutaneous fat tissue, absorbable synthetic cotton fiber, oxidized cellulose (Surgicel Absorbable Hemostat), can be used effectively to fill the defect. This absorbable hemostat can be unravelled like cotton.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








