Chapter 26 BLADDER AUGMENTATION
Bladder augmentation has evolved since the initial report in 1899 by Mikulicz,1 who first described the use of gastrointestinal tract segments for lower urinary tract reconstruction. In large part, this resulted from the introduction of clean intermittent catherization,2 the poor long-term results associated with the ileal conduit,3 realization about the importance of detubularization,4 and the importance of the role of bladder storage pressures in determining upper tract function.5 Augmentation cystoplasty with various intestinal segments has become an accepted reconstructive option for intractable incontinence and poor bladder compliance in many neuropathic and non-neuropathic disorders.6 Patient factors then guide individual selection of the augmentation method used.
INDICATIONS
The main indications for bladder augmentation are the presence of upper tract deterioration caused by high detrusor pressures at reduced bladder capacity and incontinence resulting from idiopathic detrusor instability. Compromised bladder capacity may be seen in patients with spina bifida, spinal cord injury, multiple sclerosis, or congenital conditions such as bladder exstrophy and its variants. Less common causes of reduced bladder capacity include chronic, interstitial, or radiation cystitis. Preoperative urodynamic studies should demonstrate a low-capacity, high-pressure bladder that is refractory to optimal medical management and intermittent catherization.7 When the native urethra is destroyed or cannot be catheterized, a continent catheterizable or an incontinent stoma to the augmented bladder or native bladder can be used. The options for bladder augmentation are intact gastrointestinal segments, seromuscular gastrointestinal segments, augmentation with tissue-engineered urothelium, autoaugmentation, and ureterocystoplasty. Various pros and cons are associated with each of these methods.
AUGMENTATION USING GASTROINTESTINAL SEGMENTS
Augmentation Technique
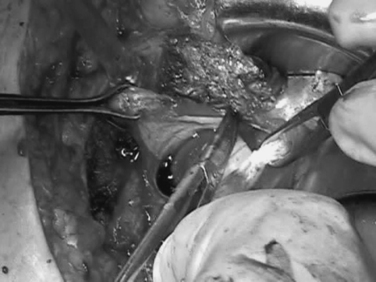
Enterocystoplasty with ileum or colon is the most commonly used procedure for vesical augmentation. Patients are admitted overnight (i.e., non-neurogenic cases) or 2 days earlier (i.e., neurogenic cases) for a complete mechanical and antibiotic bowel preparation. Intraoperatively, the ileoplasty is fashioned from 25 to 30 cm of ileum at least 15 cm from the ileocecal valve (Fig. 26-1). The segment of chosen bowel on its mesentery should be tested to ensure that it reaches the deep pelvis easily (Fig. 26-2). Using a hand-sewn or stapled technique, an enteroenterostomy is performed. The closed ileal segment is then detubularized at the antimesenteric border, beginning and ending approximately 2 cm from the closed ends (Fig. 26-3). The two adjacent borders of detubularized ileum forming what will be the posterior wall of the ileocystoplasty are then sutured with 2-0 Vicryl (Fig. 26-4). At this point, the bladder is distended with saline, and the overlying peritoneum is stripped from the posterior and superior surfaces (Fig. 26-5). A transverse “smile” incision is then made approximately 3 cm above the ureteral orifices, creating an anteriorly based detrusor flap.6 The small bowel is sutured to the bladder using a running transluminal suture in the posterior wall and then using a running suture of 0 Vicryl up both sides so that the anterior flap of bladder is placed between the two anterior walls of the reservoir (Fig. 26-6). In patients who cannot perform catheterization, the more distal portion of the ileal segment is left longer to bring it to the skin as an incontinent stoma, usually in the right iliac fossa. Patients in whom urethra closure is required need ileocecal augmentation using a reinforced ileocecal valve or the appendix as a continent neourethra for catheterization. Alternatively, if availability or mobility of the ileum is limited, left or right colon can be used. For ileocecocystoplasty, the right colon and ileum are mobilized and prepared as for an Indiana pouch. As first described by Sinaiko in 1956,8 gastrocystoplasty is a suitable option for patients with cloacal exstrophy or metabolic acidosis from renal insufficiency.9 Simultaneous pubovaginal slings can also be performed in patients with intrinsic sphincter deficiency, and urethra closure can be carried out in patients with urethral erosion. Overall, whether ileum, colon, or other segments are used, the goal is to ensure a low-pressure, high-volume reservoir with a low incidence of postoperative incontinence.4,10–12

Figure 26-1 The ileoplasty is fashioned from 25 to 30 cm of ileum at least 15 cm from the ileocecal valve.
Complications of Gastrointestinal Bladder Augmentation
The type of metabolic complications that occurs after an enteric augmentation is directly related to the segment of bowel chosen and the amount of time that the urine spends in contact with the bowel mucosa.13–15 Because vitamin B12 is absorbed from the terminal ileum and is responsible for erythrocyte formation,16 ileocystoplasty can potentially lead to vitamin B12 deficiency and subsequent development of pernicious anemia. The chosen segment of ileum therefore should be selected from an area at least 15 to 20 cm proximal to the ileocecal valve. The interposition of bowel in the urinary tract can also lead to acid-base changes. Hyperchloremic metabolic acidosis can develop with the use of ileum or colon, and hypochloremic metabolic alkalosis can develop if stomach is used.17 Patients in chronic alkalotic states would therefore do better with an intestinal cystoplasty, and patients with chronic renal insufficiency or metabolic acidosis should be considered for gastrocystoplasty or composite grafts using stomach. Patients considered for gastrocystoplasty should be advised that up to one third of patients, especially those with a sensate bladder (up to 50%), may experience hematuria and dysuria syndrome.18–20 This has led to recommendations that this procedure not be performed in patients with intact perineal sensation or in incontinent patients because the acidic urine may lead to excoriation of skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree