Anatomy of the Pelvic Viscera
Geoffrey W. Cundiff
BACKGROUND
Value of Surgical Anatomy
As in all surgical specialties, the reconstructive pelvic surgeon is frequently faced with situations that are best addressed by applying a clear understanding of the pertinent anatomy. Ideally, the art of surgery should involve the application of a repertoire of surgical techniques to the given pathology. However, given the phenotypic and pathophysiologic variations that exist in nature, a firm understanding of anatomical variation is paramount to good surgical outcomes. Often, when faced with a challenging case, what separates a great surgeon from an average surgeon is a confidence in the given anatomy that allows for informed actions. In short, anatomical understanding is the foundation of sound surgical technique.
Many of you who read this book are more than reconstructive surgeons. As investigators, the mastery of three-dimensional anatomy provides a framework for understanding the complex pathophysiology of pelvic floor dysfunction. This in turn provides insight that allows us to teach female pelvic medicine and surgery in a meaningful way.
General Considerations
There are a number of factors that make the study of pelvic anatomy particularly challenging. These include gender differences, physical constraints due to a surrounding bony pelvis, and challenging three-dimensional relationships. In this context it is wise to begin our tour of the pelvic anatomy by reviewing some underlying principles. First, all of the pelvic viscera, including the uterus, function primarily as storage units with a secondary role of the timely release of the stored material. The function of the pelvic organs places certain constraints on their physical form. Towards achieving these constraints, the pelvic viscera uniformly comprise a hollow viscus capable of significant distention, as well as a sophisticated closure mechanism. Moreover, the mouth or opening of the viscus is generally well anchored with a three-dimensional tether, while the distensible body of the viscus is relatively mobile to facilitate the increased volume of distention.
ANATOMY OF SUPPORT
Bony Pelvis
In considering the functions of the bony pelvis, the skeletal roles, provision of a supportive base for the osseous framework surrounding the viscera of the thorax, and a stable point of articulation for the lower extremities, should not overshadow the important functions that the bony pelvis provides for the pelvic viscera. These roles become apparent when considering experiments of nature, and phenotypic variation that can have a negative impact on pelvic floor function.
The skeletal anomalies associated with bladder exstrophy offer a dramatic example. Affected women have a wide transverse inlet, shortened anterior posterior pelvic diameter, and absent symphysis pubis. These variations have such an impact on support that nearly 100% of affected women develop pelvic organ prolapse (1). Less severe versions of the skeletal anomalies found in bladder exstrophy are associated with the development of pelvic floor disorders in women without congenital anomalies. Two matched case-control studies showed that women with prolapse and other pelvic floor disorders, when compared to controls, have wider transverse inlets and narrower anterior-posterior diameters (2,3). Even subtle variations in
the orientation of the bony pelvis appear to affect function. Loss of lumbar lordosis that results in a less vertically oriented pelvic inlet, for example, is also associated with pelvic organ prolapse (4,5). These morphologic variations may provide a larger hiatus for abdominal pressure transmission. Alternatively, these skeletal variations may predispose women to maternal soft-tissue injury during parturition (2). Recognizing the impact of these morphological variations highlights the central function of the bony pelvis in pelvic support, namely serving as points of attachment for the pelvic floor musculature and connective tissue supports.
the orientation of the bony pelvis appear to affect function. Loss of lumbar lordosis that results in a less vertically oriented pelvic inlet, for example, is also associated with pelvic organ prolapse (4,5). These morphologic variations may provide a larger hiatus for abdominal pressure transmission. Alternatively, these skeletal variations may predispose women to maternal soft-tissue injury during parturition (2). Recognizing the impact of these morphological variations highlights the central function of the bony pelvis in pelvic support, namely serving as points of attachment for the pelvic floor musculature and connective tissue supports.
The coxal or innominate bones, commonly known as the hip bones, articulate posteriorly with the sacrum at the sacroiliac joints and anteriorly with each other at the pubic symphysis. Developmentally, the coxal bone forms as a fusion of three constituent bones: the ilium superiorly, the ischium inferiorly and posteriorly, and the pubic bone inferiorly and anteriorly. These smaller bones fuse to create the acetabulum and articulate with the paired coxal bone at the pubic symphysis.
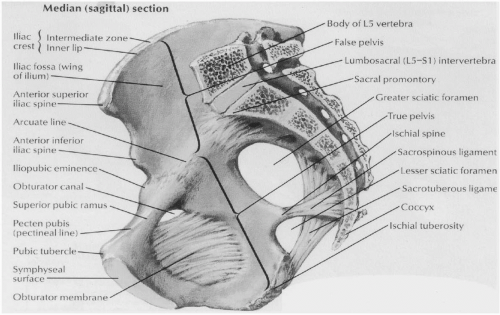
Taken together, the coxal bones and sacrum create an angulated cylinder, or stove pipe cavity. The superior portion is the inlet to the true pelvis, circumscribed by the linea terminalis. It is described by the posterior pubic symphysis, the inner aspects of the superior pubic rami, also known as the arcuate line of the ilium, as well as the alar portions and promontory of the sacrum. In the standing female, this inlet lies in a plane 60 to 65 degrees from the horizontal plane. This pelvic orientation places the anterior iliac spines and pubic tubercule (the anterior edge of the symphysis pubis) in the same vertical plane. Similarly, the anterior border of the greater sciatic foramen is almost vertical in this orientation (Fig. 1.1).
The pelvic outlet is diamond-shaped, with the apices defined by bony landmarks—the symphysis pubis anteriorly, the ischial tuberosities laterally, and the tip of the coccyx posteriorly. The diamond can be further dissected into two triangles, with the anterior triangle defined by the symphysis and two tuberosities and the posterior triangle defined by the coccyx and two tuberosities (Fig. 1.2).
These triangles lie in different planes. In the standing position, the anterior triangle is horizontal, while the posterior triangle is angled posteriorly at approximately 130 degrees. The anterior triangle provides the exit point for the bladder and
urethra and is called the urogenital triangle. Similarly, the posterior triangle is the exit point for the anus and is called the anal triangle. The lateral edges of the anteior triangle are the ischiopubic rami, while the lateral edges of the posterior triangle are the sacrotuberous ligaments (see Fig. 1.1). The sacrotuberous ligaments travel medially and superiorly from the ischial tuberosities to the lateral and posterior aspects of the lower half of the sacrum. These ligaments form the posterior border of the pelvic outlet and perineum.
urethra and is called the urogenital triangle. Similarly, the posterior triangle is the exit point for the anus and is called the anal triangle. The lateral edges of the anteior triangle are the ischiopubic rami, while the lateral edges of the posterior triangle are the sacrotuberous ligaments (see Fig. 1.1). The sacrotuberous ligaments travel medially and superiorly from the ischial tuberosities to the lateral and posterior aspects of the lower half of the sacrum. These ligaments form the posterior border of the pelvic outlet and perineum.
Ischial Spine
The anterior border of the greater sciatic foramen ends in a blunt projection pointing medially, called the ischial spine. In the standing pelvis, the ischial spine is about 2 to 3 cm above the level of the pubic crest. This orientation provides an almost horizontal relationship between the posterior aspect of the pubic bone and ischial spine. The sacrospinous ligament travels medially and posteriorly from the ischial spine to the lateral and anterior aspects of the lower portion of the sacrum and the coccyx. Lying superior to the sacrotuberous ligament, this ligament transects the greater sciatic notch, creating the greater and lesser sciatic foramen (see Fig. 1.1).
The greater and lesser sciatic foramen, as well as the obturator foramen, serve as conduits for muscles, vasculature, and nerves that enter and exit the true pelvis. Knowledge of these structures’ spatial relationships helps to avoid surgical injuries. Because the ischial spine is easily palpated, it serves as an excellent surgical reference point, and consequently, a surgeon is well served by a three-dimensional understanding of the anatomy surrounding the ischial spine (Fig. 1.3). This invaluable landmark indicates the normal axis of the vagina, as the arcus tendineus fascia pelvis ends at the spine. The pelvic ureter leaves the sidewall 1 to 2 cm from the spine to pass medially on the pubocervical fascia before entering the inferior bladder wall. The pudendal nerve and vessels exit the pelvis through the greater sciatic foramen only to course beneath the ischial spine and sacrospinous ligament before re-entering the lesser sciatic foramen. The ischial spine is consistently found beneath the intermediate portion of the uterosacral ligament, although its location with respect to the anterior and posterior edges is variable (6).
Obturator Foramen
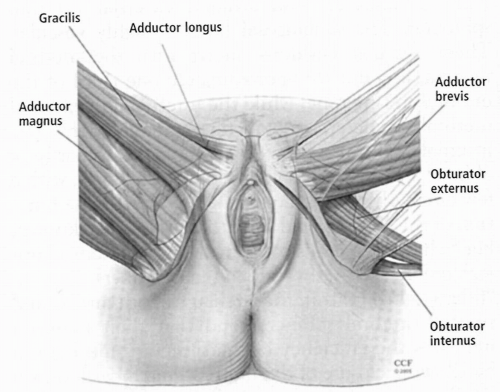
Recent surgical advances have utilized the obturator membrane and surrounding muscles to anchor implanted grafts. For many pelvic surgeons, this surgical approach is unfamiliar, necessitating the acquisition of new anatomical knowledge of the obturator compartment.
The obturator foramen is a large oval window bounded by the pubic ramus and ischium. The obturator membrane covers this opening. The obturator
internus muscle originates from the entire bony margin of the obturator foramen on the pelvic side of the obturator membrane. This broad origin allows the muscle to compose most of the lateral pelvic sidewall. The tendon of the obturator internus muscle exits the lesser sciatic foramen on its way to insert onto the greater trochanter, providing for external rotation of the femur. Anteriorly and lateral to the edge of the obturator foramen is a groove in the body of the pubic bone. The obturator
membrane’s attachment here creates the obturator canal, through which pass the obturator vessels and nerve as they course anteriorly from the posterior aspect of the pelvic sidewall.
internus muscle originates from the entire bony margin of the obturator foramen on the pelvic side of the obturator membrane. This broad origin allows the muscle to compose most of the lateral pelvic sidewall. The tendon of the obturator internus muscle exits the lesser sciatic foramen on its way to insert onto the greater trochanter, providing for external rotation of the femur. Anteriorly and lateral to the edge of the obturator foramen is a groove in the body of the pubic bone. The obturator
membrane’s attachment here creates the obturator canal, through which pass the obturator vessels and nerve as they course anteriorly from the posterior aspect of the pelvic sidewall.
The obturator compartment lies on the outside of the obturator membrane. The adductor muscles of the lower extremity find their origin in this region. With the patient in the lithotomy position the adductor muscles originate on the ischiopubic ramus and course along the inner aspect of the thigh. Most superficial, from anterior to posterior, are the adductor longus, gracilis, and adductor magnus. Deep to these muscles are the adductor brevis anteriorly and the obturator externus posteriorly (Fig. 1.4). The adductor muscles are innervated by the obturator nerve, which emerges from the obturator canal between the adductor longus and adductor brevis, and beneath the gracilis. The nerve then bifurcates into anterior and posterior divisions. Some authors have described a similar course for the branches of the obturator artery, although recent cadaver work from Whiteside suggests variable courses for these branches (7). Regardless, the medial aspect of the obturator foramen is relatively safe between the level of the clitoris anteriorly and the anus posteriorly.
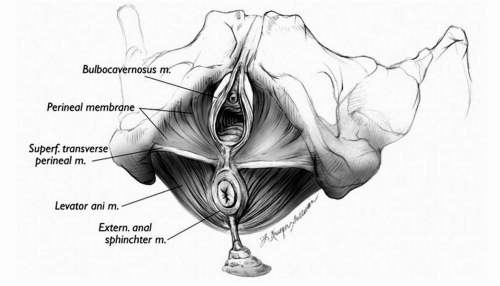
Pelvic Floor Musculature
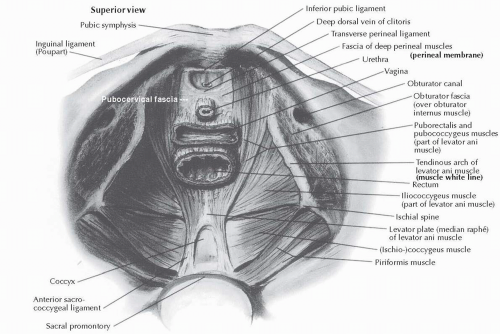
Within the bony pelvis is a basin open at the pelvic inlet but closed beneath, except for the levator hiatus, by a muscular lining composed of the pelvic musculature. Anteriorly, this group of skeletal muscles includes the obturator internus muscles, which originate on the pubic ramus lateral to the symphysis pubis and cross over the inner aspect of the obturator membrane. Posteriorly, the piriformis muscles originate from the anterior and lateral aspects of the sacrum in its middle to upper portion. They then course laterally through the greater sciatic foramen to insert on the greater trochanter beside the obturator internus tendon. Inferiorly, the pelvic diaphragm, a group of paired muscles that include the levator ani and coccygeus muscles, creates the pelvic floor (Fig. 1.5).
The levator ani muscles are subdivided, from medial to lateral, into the puborectalis, pubococcygeus, and iliococcygeus muscles. The puborectalis and pubococcygeus muscles originate from the inner aspect of the pubic rami on either side of the midline at the level of the pubic symphysis. The muscle fibers pass laterally to the vagina and rectum, creating a U-shaped sling surrounding the genital hiatus medially. The muscle fibers of the iliococcygeus
muscles pass laterally to the pubococcygeus muscles, fanning out to create the pelvic floor posteriorly and laterally.
muscles pass laterally to the pubococcygeus muscles, fanning out to create the pelvic floor posteriorly and laterally.
The iliococcygeus muscles are unique in their origin from a curvilinear thickening of the parietal fascia overlying the obturator internus muscle known as the arcus tendineus levator ani or muscle white line (see Fig. 1.5). This tendinous muscle origin runs on top of the parietal surface of the obturator internus muscle, from the posterior symphysis pubis to the ischial spines. The iliococcygeus muscles insert on the lower aspect of the lateral sacrum.
The muscles of the pelvic diaphragm are composed of a unique type of striated muscle that contains a majority of type I (slow twitch) muscle fibers that maintain a constant resting tone over time. Each muscle group also contains a smaller proportion of type II (fast twitch) fibers, permitting them to respond quickly during sudden increases in intra-abdominal pressures (8). Contraction of the pelvic diaphragm closes the genital hiatus and provides a horizontal levator plate on which the pelvic viscera lie.
Orientation of the Pelvic Viscera
The urethra, lower vagina, and anus all exit the pelvic outlet via the levator hiatus. The puborectalis and pubococcygeus muscles bound this muscular opening in the pelvic floor. The constant resting tone of the puborectalis and pubococcygeus not only closes the genital hiatus but also pulls the distal vagina and anorectal junction toward the pubic symphysis, creating a near-right angle between the anal and rectal canals. This angle is referred to as the anorectal angle. The posterior deflection is also present in the urethra and vagina. The acuity of the angle results from the opposing forces of the baseline contraction of the pelvic diaphragm, actively pulling anteriorly, countered by the passive force of the posterior connective tissue attachments, which maintain the upper portion of the pelvic viscera deflected posteriorly. This results in consistent anatomical relationships between the vaginal apex, the ischial spines, and the sacrum in women with normal support. A recent study defined these relationships based on magnetic resonance imaging of the pelvis in nulliparous adult females who had a normal gynecologic examination. In the standing female patient, the bladder, the upper two thirds of the vagina, and the rectum lie in a horizontal axis over the muscular levator plate (9). As the vaginal canal courses past the ischial spines toward the sacrum, the posterior fornix or vaginal apex normally lies anterior to S2, about 4 to 5 cm medial, 1 to 2 cm anterior, and 1 to 2 cm superior (cranial) to the ischial spines (10) (Fig. 1.6).
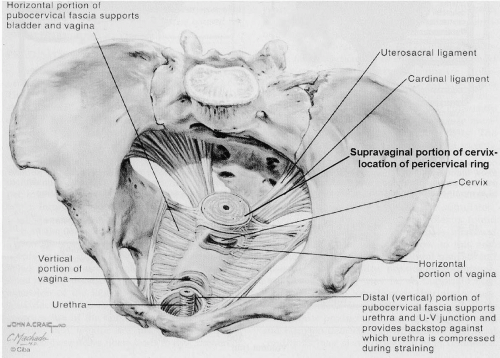 FIGURE 1.6 ● Orientation and connective tissue support of the vagina. (From Retzky SS, Rogers RM. Urinary incontinence in women. In: Clinical symposia. Summit, NJ: Ciba-Geigy Corp, 1995;47(3), adapted from Plate 3, p. 7. Copyright © 1995 Icon Learning Systems, LLC. A subsidiary of MediMedia, USA, Inc. All rights reserved.) |
Connective Tissue Support
The connective tissue support of the pelvis arises from both the parietal fascia covering the pelvic musculature and the visceral fascia investing the pelvic viscera. The visceral fascia surrounds and mechanically supports the pelvic viscera as well as enveloping the supplying vasculature, nerves, and lymph channels. This visceral web runs from the pelvic brim along the upper sidewalls and back wall of the pelvis to the anatomic level of the ischial spine, where the network then proceeds horizontally (in the standing patient) to the obturator internus muscles laterally, and the pubic bones and perineal body inferiorly. This support network is continuous and interdependent within the three-dimensional muscular pelvic basin. Importantly, these visceral connective tissues vary in composition, thickness, strength, and elasticity, depending on the mechanical and physiologic support requirements in each particular location within the network.
The parietal fascia covering the pelvic musculature is a mechanically dense matrix of connective tissue consisting predominantly of collagen fibers coalescing into thick bundles that are then interwoven into a strong, three-dimensional sheet (11). The vascular supply is limited, and active fibroblasts are few in number within this dense connective tissue. In contrast, visceral fascia, also referred to as the endopelvic fascia, is a loose, three-dimensional meshwork of collagen, elastin, and smooth muscle with a richer vascular supply. The term fascia is ambiguous as this fibromuscular tissue layer lacks the dense collagen usually associated with the term, but it includes a soft ground substance with different connective tissue cells, including fibroblasts, smooth muscle cells, and elastin in addition to type III collagen, all loosely arrayed to create an elastic fibromuscular layer (11). This meshwork surrounds and peripherally supports the viscera in both the abdominal and pelvic cavities. It is flexible and elastic within limits, as this visceral connective tissue mechanically stretches within limits, but beyond these limits, it breaks.
The endopelvic fascia serves two important roles. The first is the provision of flexible conduits and physical supports for the vasculature, visceral nerves, and lymph tissue that service the viscera. The visceral fascial capsules envelop the bladder,
urethra, cervix, vagina, rectum, and anal canal (12). They are intimately attached to the surrounding smooth muscle coat of each viscus. Within these capsules are the vasculature, visceral nerves, lymph nodes and channels, and adipose tissue (areolar tissue). The fascial covering of each hollow viscus provides support during storage, distention, and evacuation.
urethra, cervix, vagina, rectum, and anal canal (12). They are intimately attached to the surrounding smooth muscle coat of each viscus. Within these capsules are the vasculature, visceral nerves, lymph nodes and channels, and adipose tissue (areolar tissue). The fascial covering of each hollow viscus provides support during storage, distention, and evacuation.
The second role of the visceral fascia is to suspend the viscera mechanically over the pelvic floor. The horizontal orientation of the pelvic viscera over the pelvic diaphragm creates a flap-valve mechanism that prevents prolapse of the pelvic viscera through the genital hiatus. Increased intra-abdominal pressure, such as with Valsalva straining, generates force perpendicular to the longitudinal axis of the vagina and pelvic viscera, compressing these organs against the simultaneously contracting levator plate.
While the connective tissue support of the pelvis provides a seamless system of meshwork support for the pelvic viscera, the system is more easily comprehended when broken up into constituent parts. DeLancey introduced the concept of dividing the connective tissue support in the pelvis into three levels, with levels I, II, and III representing apical, middle, and distal vaginal support, respectively (13) (Fig. 1.7). Level I support of the paracolpium and parametrium is provided by the cardinal and uterosacral ligaments, which suspend the vaginal vault. Level II is the support of the midvagina, produced by the lateral attachments of the anterior and posterior endopelvic fascia to the pelvic sidewalls. Level III support results from the fusion of these same sheets with the pubic symphysis anteriorly and perineal body posteriorly. Although assigning these levels artificially divides what is actually a continuum of connective tissue in the pelvis, the levels can provide a useful anatomical tool to understand normal support and loss of support at different levels.
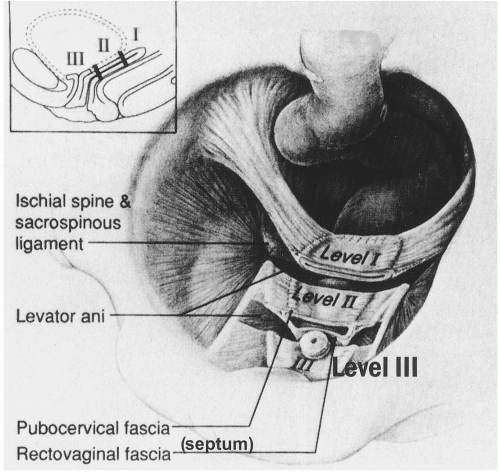 FIGURE 1.7 ● Levels of pelvic support. (From DeLancey JOL. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 1992;166:1719, with permission.) |
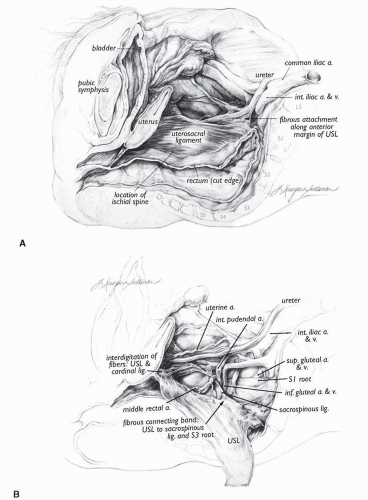
The origin of the uterosacral ligament is fanlike at the sacrum, narrowing to its smallest width just proximal to the cervix. Although some texts report the uterosacral ligament to have its origin only from S2-4, anatomical investigations show the uterosacral ligament to be attached broadly to S1, S2, and S3 and variably to S4, with additional attachments to the sacral periosteum and sacrospinous ligament (6,14). This broader attachment disperses the suspensory forces acting on the uterosacral ligament (see Fig. 1.3A).
Campbell identified three distinct histological regions of the uterosacral ligament (14). The superior third, which attaches to the sacrum, is composed of loose strands of connective tissue and intermingled fat, with few vessels, nerves, or lymphatics. The intermediate portion has denser connective tissue with a few scattered smooth muscle fibers, nerve elements, and blood vessels. At the cervical attachment, the uterosacral ligament coalesces into closely packed bundles of smooth muscle with abundant medium-sized and small blood vessels and nerve bundles. The
uterosacral ligament is, therefore, densest where it inserts into the paracervical ring. However, the distal uterosacral ligament attachments to the cervix also extend down the posterior lateral aspects of the vagina (6,14). Together these attachments draw the cervix posteriorly towards the hollow of the sacrum (10) (see Fig. 1.6).
uterosacral ligament is, therefore, densest where it inserts into the paracervical ring. However, the distal uterosacral ligament attachments to the cervix also extend down the posterior lateral aspects of the vagina (6,14). Together these attachments draw the cervix posteriorly towards the hollow of the sacrum (10) (see Fig. 1.6).
This direction is balanced by the lateral tension of the cardinal ligaments. The fan-shaped cardinal ligament creates a sheath that envelops the uterine artery and vein, fusing with the paracervical ring medially. The internal iliac artery courses along this border and helps to establish the cardinal ligament sheath. The fibers of the uterosacral and cardinal ligaments intermingle at the cervical portion to create a smaller, fanlike insertion with fibers extending anteriorly above the internal cervical os and posteriorly down onto the proximal third of the vagina. Together the cardinal and uterosacral ligaments create the paracervical ring of connective tissue surrounding the cervix at the vaginal apex. This is also the attachment for the endopelvic fascia of the anterior and posterior vaginal walls. The cervix, with its surrounding paracervical ring, therefore, acts like the hub of a wheel for the connective tissue support of the vagina (see Fig. 1.6).
There are two prominent lateral connective tissue structures that play a key role in both muscular and connective tissue support of the pelvis: the arcus tendineus levator ani and the arcus tendineus fascia pelvis. Arising as condensations of the parietal fascia of the obturator internus and levator ani muscles, these dense aggregations of connective tissue contain more organized fibrous collagen than the visceral or endopelvic fascia (15). As previously discussed, the arcus tendineus levator ani provides the anchorage for the origin of the levator ani muscles, the iliococcygeus and pubococcygeus muscles. Anteriorly, the arcus tendineus levator ani inserts at the pubic rami and then crosses over the obturator internus muscle to insert posteriorly at the ischial spine (Fig. 1.8).
The arcus tendineus fascia pelvis is a condensation of the parietal fascia of the obturator internus muscle and the visceral fascia enveloping the anterior and posterior vagina. The arcus tendineus fascia pelvis is medial to and runs nearly parallel to the arcus tendineus levator ani. It inserts at the anterior pubic rami, adjacent to the pubic symphysis and slightly anterior to the arcus tendineus levator ani. Posteriorly, the arcus tendineus fascia pelvis joins with the arcus tendineus levator ani to insert at or just above the ischial spine (see Fig. 1.8). The arcus tendineus fascia pelvis provides the lateral anchoring sites for the anterior vaginal wall and posterior vaginal wall.
Anteriorly, the fibromuscular layer of the anterior vaginal wall, known as the pubocervical fascia, bridges the two arcus tendineus fascia pelvi, providing support for the bladder and urethra. The fibromuscular layer of the posterior vaginal wall is also known as Denonvilliers’ fascia or the rectovaginal septum. It arises from fusion of the two walls of the embryological peritoneal cul-de-sac (16). This creates a fibromuscular sheet that spans the posterior vaginal wall and coalesces with surrounding structures. Recent histological work demonstrates that this layer is synonymous with the vaginal muscularis of the posterior vaginal wall (17). Superiorly it thins out centrally and attaches to the cervix and the cardinal uterosacral support of the vaginal apex. Laterally the rectovaginal fascia attaches to the pelvic sidewall (18). In the upper vagina the lateral attachment coalesces with the lateral support of the anterior vaginal wall at the arcus tendineus fascia pelvis. The lower half of the rectovaginal fascia fuses with the aponeurosis of the levator ani muscle along a line referred to as the arcus tendineus fascia rectovaginalis (18) (Fig. 1.9). It converges with the arcus tendineus fasciae pelvis at a point approximately midway between the pubic symphysis and the ischial spine to form a Y configuration on the sidewall of the pelvis. The point of convergence of the two lines is at the point along the tube of the vagina where the pelvic floor becomes wider than the vagina. Superior to this point the fascia endopelvina bridges the gap between the vaginal tube and the pelvic sidewall (12) (Fig. 1.10). This web of connective tissue coalesces with the fascia of the obturator internus muscle to create the arcus tendineus fascia pelvis, as well as with extensions of the uterosacral ligaments. The fascia endopelvina in the upper vagina, and separate attachments of the pubocervical fascia and rectovaginal septum posteriorly, result in different cross-sections of the vagina at different levels. The anatomical attachments are reflected on coronal magnetic resonance imaging (MRI) images that show a characteristic H shape to the vaginal lumen distally, as compared with an oval shape superiorly.
Urethral Support
Distally, the pubocervical fascia has fascial and muscular attachments that provide passive and active support of the distal third of the urethra. This is the only portion of the urethra that is fixed to the pubic bone. The passive support sometimes referred to as a hammock of support (19) results from a connective tissue bridging of the pubocervical fascia and its distal lateral attachments, often termed pubourethral ligaments (Fig. 1.11). The
active support results from the attachment to the arcus tendineus levator ani. A separate structure, the pubovesical “ligament” or muscle, composed of smooth muscle, extends from the detrusor muscle to the arcus tendineus fascia pelvis and pubic bone (Fig. 1.12). The pubovesical ligament is distinct from the urethral supports and is an extension of the smooth muscle of the detrusor of the bladder. It may assist in opening the bladder neck during micturition (20).
active support results from the attachment to the arcus tendineus levator ani. A separate structure, the pubovesical “ligament” or muscle, composed of smooth muscle, extends from the detrusor muscle to the arcus tendineus fascia pelvis and pubic bone (Fig. 1.12). The pubovesical ligament is distinct from the urethral supports and is an extension of the smooth muscle of the detrusor of the bladder. It may assist in opening the bladder neck during micturition (20).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree