Chapter 52 Adhesion Prevention
INTRODUCTION
The relevance of pelvic and peritoneal adhesions to the practice of reproductive endocrinology and infertility clearly relates to their association with infertility and chronic pelvic pain. In addition, postoperative adhesions are also responsible for significant complications, most notably adhesive bowel obstruction, and increase the difficulty of subsequent surgical procedures, which enhances the potential for intraoperative complications. Interestingly, the first case report of fatal intestinal obstruction caused by intra-abdominal adhesions was a woman who developed adhesions after removal of an ovarian tumor.1 Although the peritoneal cavity is of interest to the reproductive surgeon, postoperative adhesions also occur in other spaces, such as the pleural and pericardial cavities.
HISTORICAL PERSPECTIVE
Ancient Egyptians, known for their detailed descriptions of human anatomy, described pelvic adhesions several thousands years ago. Pleural adhesions were first described in the Babylonian Talmud in 440 A.D.2 Although adhesions caused by peritonitis have been recognized since the early 1700s, it was not until the widespread use of anesthesia in the mid-1800s when invasive abdominal procedures became more prevalent that the extent of the problems caused by intra-abdominal adhesions was realized.
By the 1880s, the first published reports describing the use of adjuvants for adhesion prevention began to appear in the surgical literature. Over the next 100 years, a plethora of scientific reports and anecdotal accounts described the use of everything from amniotic fluid, bovine cecum, gold-beater’s skin, shark peritoneum, fish bladder, vitreous of calf’s eyes, various gums, lubricants, fluids, gels, polymers, physical barriers, and a host of mechanical separation methods to prevent adhesions. Unfortunately, the results of most of these studies were equivocal, with no more than a small percentage of success. Even in this age of surgical sophistication and new operating room technology, our age-old nemesis, the intra-abdominal adhesion, remains a significant, long-term, and recurrent postoperative problem.3
DEFINITION, TYPE, AND EXTENT OF DISEASE
Intra-abdominal adhesions are strands or membranes of fibrous tissue that can be attached to the various intra-abdominal organs, sometimes connecting them together (Fig. 52-1). The term adhesion in the medical field refers to the abnormal joining of anatomic structures at sites where no such anatomic attachment should exist. Adhesions usually develop in conjunction with surgery at sites of adhesiolysis and other operative sites, but also occur at “distant” sites where no surgical procedure was done.
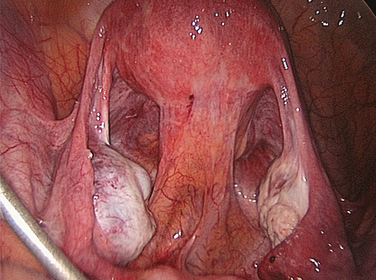
Figure 52-1 Pelvic adhesions involving the uterus and bowel. This patient had a previous myomectomy.
To accurately describe the extent of peritoneal adhesions during clinical investigations, various scoring systems have been developed. Systematic assessment of adhesions is mandatory to decrease interobserver variation and to provide quantitative data corresponding to their extent and clinical significance.4 Most of the available scoring systems incorporate adhesion location, vascularity, and type (thickness). However, the current scoring systems suffer from the lack of validation for outcomes such as fertility, pain, and bowel obstruction, which makes the interpretation of the results of research related to adhesion development and prevention difficult. Thus, the question is often asked that if a study demonstrates a significant change in an adhesion score, does that reflect true clinical relevance in the extent of adhesive disease?
PREVALENCE OF DISEASE
Despite the application of microsurgical technique and use of surgical adjuvants by experienced surgeons, the development of intraperitoneal postoperative adhesions is common. Currently, no serum marker or scanning technique is consistently able to identify adhesions, and a repeat operative procedure is required for evaluation.5
In a postmortem study of victims of motor vehicle accidents, intra-abdominal adhesions were encountered in 67% of individuals who had a history of abdominal operation.6 The prevalence among patients who had undergone major operations and multiple procedures was 81% and 93%, respectively. Most studies have shown that after an intra-abdominal operation, most patients developed adhesions. One study found that after merely one previous abdominal operation, 93% of patients had adhesions.7 On the other hand, intra-abdominal adhesions among patients who had never experienced a laparotomy were found in only 10.4%.
Within 1 year of laparotomy, 1% of patients develop adhesion-related intestinal obstruction;7 11% to 12% of them will suffer from recurrence later.8 In reports based on data from laparoscopies9 and autopsies,6 60% and 69% of women, respectively, had pelvic adhesions after previous abdominopelvic operations. Variation in the incidence of postoperative adhesions may be explained by differences in the extent of surgery, differences in the incidence or severity of prior surgery or other etiologic events, and in what each investigator considered to be a “significant” adhesion. It is important to emphasize that although some investigators believe all adhesions may not be clinically significant, others would emphasize that you cannot tell which adhesions will cause pain or contribute to bowel obstruction.
ECONOMIC IMPACT OF ADHESIONS
The economic impact of adhesions as a complication of surgery is enormous. In the United States, 446,000 procedures were performed annually to remove abdominopelvic adhesions.10 This included 347,000 operations to release peritoneal adhesions and approximately 100,000 procedures to liberate intestinal adhesions. The cost of morbidity associated with adhesions is large.11 Few studies have been conducted to evaluate the financial impact of adhesion-related problems on the medical budget, and many of the studies could have underestimated the actual financial impact of adhesive disease by not considering the costs of performing diagnostic tests, consultations with other services such as gastroenterology, the increase in operative time required to free adhesions, and the complications due to inadvertent injury to other vital structures while freeing adhesions. In addition, a significant number of planned laparoscopic surgeries are converted to laparotomy because of failure to safely enter the abdomen and achieve adequate pneumoperitoneum. Finally, there are costs associated with long-term morbidity such as adhesion-related infertility and repeated admissions for bowel obstruction. The psychological impact of adhesion-related conditions that lead to loss of work might add to the economic burden.
In the United States, an analysis of all hospitalizations for adhesions was performed using the 1988 National Hospital Discharge Survey. Of a total 281,982 hospitalizations, 51,100 were adhesion-related admissions. In total, there were more than 948,000 hospital-days of care, accounting for a cost of approximately $1.18 billion.10 In 1994, the same authors updated their database and found the annual overall cost to be approximately $1.3 billion. They also reported that lysis of adhesions was responsible for 1% of hospitalization in the United States.12
In a study that evaluated hospital discharge for adhesion-related bowel obstruction between 1990 and 1996, the total number of patients increased from 115,067 in 1990 with a total length of hospitalization of 962,642 days to 139,716 patients with a total length of hospitalization of 885,396 days in 1996.13 The total costs increased steadily from $924 million in 1990 to $1.4 billion in 1996. Among those who were treated medically, there were 88,601 hospitalizations in 1990 and 110,817 in 1996, with a parallel increase of cost from $261 million in 1990 to $386 million in 1996.
In the United Kingdom, Menzies and coworkers14 reviewed 110 hospital admissions resulting from adhesion-related small-bowel obstruction over a 2-year period. Of 110 admissions, surgical treatment was performed in 37% of patients and conservative management in the remaining patients. The total costs per admission were $7,521.28 (£4,677.41) and $2582.69 (£1,606.15) for the surgical and conservative treatment groups, respectively.
In Sweden, Holmdhal and Riseberg15 conducted a cost analysis study on adhesion-related admission among all general surgeons. Collection of data was performed after the authors analyzed the questionnaire sent to all department heads of Swedish surgical units. There were a total of 6200 patients requiring hospitalizations, accounting for 3.5% of all laparotomies. They found that the total cost for adhesion-related hospitalization was $6.1 million US annually or close to $1 million US per million Swedish inhabitants (the population of Sweden is 8.5 million).
Because of the difference in medical costs in various countries, meaningful comparisons are difficult. However, all studies suggest a huge financial impact of adhesion-related conditions to the healthcare system. Recently, Wilson16 calculated that a low-cost product with a 25% efficacy in preventing surgical adhesions could potentially generate a cost saving of £55 million over a 10-year period in the UK. In a prior study, they concluded that demonstrating the clinical effectiveness of adhesion reduction products in a randomized, controlled setting is unlikely to be feasible due to the large number of patients required. They suggested that products costing £200 (around $300 US) or more are unlikely to pay back their direct costs.17
COMPLICATIONS OF ADHESIONS
Postoperative adhesions develop after virtually every transperitoneal operation, ranging from minimal scarring present on serosal surface to dense agglutination of nearly all structures. However, postoperative adhesions are much more common than symptoms would suggest; therefore, most adhesions probably do not lead to acute symptoms or clinical sequelae.
In certain situations, adhesions may be of benefit. They may serve as adjuncts to the body’s natural defenses against intra-abdominal insults and can be lifesaving in the postoperative period by localizing leakage from suture lines, isolating an inflammatory collection, or preventing the spread of infection. Other potential benefits include neovascularization of ischemic structures such as anastomoses. However, adhesions are associated with significant morbidity such as infertility, pain, and bowel obstruction.18
Reproductive Problems
Adhesions play a significant role in the etiology of several reproductive disorders, including infertility, ectopic pregnancy, and recurrent pregnancy loss (intrauterine adhesions). From 15% to 20% of female infertility is caused by adhesions.19 Adhesions causing infertility or ectopic pregnancy may originate from endometriosis, infection such as pelvic inflammatory disease, appendicitis, or tuberculosis, as well as inflammatory bowel disease and surgery. More details on adhesions and infertility, ectopic pregnancy, and recurrent pregnancy loss are provided in other chapters of this text (see Chapters 34, 41, 47 and 48).
Intestinal Obstruction
Adhesive intestinal obstruction is the most serious complication associated with peritoneal adhesions (Fig. 52-2). In addition to the significant pain, the condition can be life-threatening and in some cases fatal. In the early 20th century, most of the cases of intestinal obstruction were due to strangulated external hernias. As abdominal and gynecologic surgeries began to be performed more routinely, the number of intestinal obstructions caused by postsurgical adhesions increased and now has surpassed those produced secondary to hernias. This statistic, however, only holds true for the western world. In poorer regions of the world, the percentage of obstruction from hernias is still greater than that caused by adhesions.20 In advanced countries, adhesions account for intestinal obstructions in 49% to 74% of cases.21 Intestinal surgeries involving the left side of the colon and rectum, appendectomies, and gynecologic procedures are the three most common surgical procedures accounting for adhesion-related intestinal obstruction.7
Both the extent and indication (e.g., cancer) of a gynecologic operation correlate significantly with the risk of postoperative intestinal obstruction. A Japanese group looked at the type of adhesions that caused intestinal obstruction and found that in 29% of cases, obstructive adhesions were small bowel to small bowel; in 48% the adhesions were small bowel to other abdominopelvic structures.22
Gynecologic malignancy increases the incidence of intestinal obstruction because more extensive operations are often required, and blockage by a tumor mass can occur. A report on 283 gynecologic patients treated for mechanical small-bowel obstruction showed that 175 (61.8%) were due to a primary or recurrent gynecologic malignancy, almost exclusively arising from the ovary.23 However, the second most common cause of obstruction was postoperative adhesions (41 patients, 14.5%), most of which followed an operation performed for a gynecologic cancer.23 Intestinal obstruction occurring in the immediate postoperative period and those that follow treatment for early-stage ovarian cancer usually are related to adhesions, whereas delayed obstruction, especially that which occurs in the presence of advanced disease, is usually tumor-related, particularly if radiotherapy is administered.24
Although small-bowel obstruction on a gynecology service occurs most frequently in women with ovarian cancer, it can occur after other extensive pelvic operations, particularly ones associated with significant pelvic infection, such as surgery for tubo-ovarian abscess. It has been suggested that the two structures most commonly involved in adhesions associated with gynecologic surgery are the omentum and the distal small intestine.18 Short, obese women have a particular tendency to develop omental and small-bowel postoperative adhesions, perhaps in part related to longer, more difficult operative procedures.6 Because colonic adhesions are less common and the restricted mesentery can preclude twisting and kinking of the lumen, the colon is involved in adhesive obstruction only 2% to 10% as frequently as the small bowel.6 Among gynecology patients colonic obstruction usually is related to recurrent or persistent pelvic tumor causing extrinsic compression of the rectosigmoid colon.23,24
Adhesive intestinal obstruction after previous surgery can be early or late. According to the general surgery literature, 17% to 29% of intestinal obstruction cases occur within 1 month,25,26 whereas the rest of the cases develop later, from 1 month to several decades after the surgery. After definitive operative management of an intestinal obstruction, the incidence of recurrence is approximately 14%. The factors contributing to occurrence or recurrence of intestinal obstruction are poorly understood.26,27
Fevang and colleagues studied a series of patients that included 500 patients who had a median follow-up of 10 years and a maximum follow-up time of 40 years after adhesive small-bowel obstruction.28 The cumulative recurrence rate for patients operated once for adhesive intestinal obstruction was 18% after 10 years and 29% at 30 years. For patients admitted several times for adhesive intestinal obstruction, the relative risk of recurrent adhesive intestinal obstruction increased with increasing number of prior episodes. The cumulative recurrence rate reached 81% for patients with four or more admissions. Other factors influencing the recurrence rate were the method of treatment of the last previous adhesive intestinal obstruction episode (conservative versus surgical) and the number of abdominal operations before the initial adhesive intestinal obstruction operation. Most recurrent adhesive small-bowel obstruction episodes occurred within 5 years after the previous one, but a considerable risk is still present 10 to 20 years after an adhesive small-bowel obstruction episode.28
The Conundrum of Chronic Pain Syndromes and Adhesions
The issue of adhesion-related pain, including chronic pelvic and abdominal pain, dysmenorrhea, and dyspareunia, has been the subject for intense debate.29 There are three important questions that need to be addressed: Do adhesions cause pain? If yes, does the extent of adhesions correlate with the nature and severity of pain? Does adhesiolysis relieve adhesion-related pain?
Adhesions May or May Not Cause Pain
The question as to whether or not adhesions cause pain does not have an entirely satisfactory answer. In favor of this relationship are the findings that adhesions contain nerve fibers30 and are innervated with substance P-containing sensory neurons, suggesting that adhesions themselves are capable of generating pain stimuli and perhaps finally suggesting a mechanism to explain the pain associated with adhesions.31 However, some have criticized reports such as this because of the potential for “tenting” of normal peritoneum during adhesion excision, such that the nerves may have been in normal peritoneum. Additionally, the apparent absence of pain in some patients with massive adhesions in contrast to claims of intense pain by patients with only minimal adhesive disease has led many clinicians to doubt that adhesions alone are “enough” pathology to “cause” pain.
The magnitude of the problem is great. As many as 20% of patients with acute pelvic inflammatory disease will have chronic pain, much of which is felt to be associated with adhesions.32 It is possible that adhesions that restrict the free movement of pelvic organs would be implicated as a cause of chronic pelvic pain.33 Approximately 20% to 50% of patients with chronic pain have pelvic adhesions.33,34
Adhesion Extent Does Not Correlate with Nature and Severity of Pain
Although several studies have suggested a significant association between adhesions and chronic pelvic pain, and the location of pain to reflect the site of adhesions, most of these studies failed to show a significant correlation between the extent of adhesions and the severity of pain.20 Similar observations have been made for the relationship between endometriosis and pain.
Adhesiolysis Does Not Always Relieve Adhesion-Related Pain
Lysis of adhesions has been proposed as the therapeutic modality of choice for patients suffering from pelvic pain in association with adhesions, and some investigators report the resolution of chronic pain in individuals after lysis of adhesions, whereas others have not noted this effect consistently or have noticed only a very short period of benefit.35,36 Obviously, the “gold standard” study to determine the utility of adhesiolysis for pain relief would be a double-blinded, randomized trial with a control arm, which would control for adhesion reformation and de novo adhesion formation, and follow-up occurring past the point of the expected placebo effect of adhesiolysis surgery. Not surprisingly, such a study would be difficult to execute because of the need to recruit a large number of patients, to perform a second-look procedure to ascertain whether adhesion reformation occurred in those patients having pain relapse after adhesiolysis, and to debate the method to use to quantify patient pain.20
Probably the closest to this ideal study are reports by Swank and colleagues,37,38 who conducted both laparotomy and laparoscopy. Neither of these studies was able to demonstrate a significant benefit of adhesiolysis to the patient population as a whole, although trends were identified. Although each of these studies was randomized, the length of follow-up was limited, and neither included second-look laparoscopy so as to allow correction for new or persisting adhesions.
Other Problems Complicating Adhesions
There are several other clinical implications of adhesions, including interference with intraperitoneal therapeutics and difficult repeat surgery. In an effort to improve both the response rates and the overall survival of patients with ovarian carcinoma, investigators have explored the safety and efficacy of antineoplastic agents delivered intraperitoneally for this malignancy. A major impediment to this innovative therapy is inadequate intraperitoneal distribution of drugs whenever extensive adhesions are present.39 Other adhesion-related complications of gynecologic surgery that do not affect fertility have not been well-studied. Voiding dysfunction, ureteral obstruction, and nonspecific gastrointestinal complaints may also be related to postoperative adhesion development.
PATHOPHYSIOLOGY OF ADHESION FORMATION
Peritoneal Cavity Repair
The abdominal cavity is lined by the peritoneum, which consists of a single layer of mesothelial cells, supported by a basement membrane and an underlying sheet of connective tissue. When it covers the abdominal wall it is called the parietal peritoneum and when it covers viscera it is called the visceral peritoneum.
Peritoneal trauma results in mesothelial damage and is accompanied by inflammation. Mesothelial cells balloon and detach from the basal membrane, thereby creating denuded areas.40 Peritoneal injury due to surgery, irradiation, infection, or irritation initiates an inflammatory reaction that increases peritoneal fluid, including proteins and cells. This fibrinous exudate leads to formation of fibrin41 by activation of the coagulation cascade.42 Within this fibrinous exudate, polymorphonuclear cells, macrophages, fibroblasts, and mesothelial cells migrate, proliferate, or differentiate (Table 52-1).
Table 52-1 The Temporal Relationship of Different Cell Types and Products in the Peritoneal Cavity (Days) after Surgical Injury
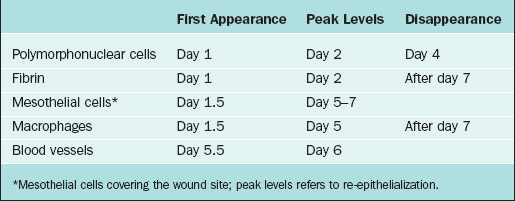
Macrophages increase in number and change functions from mainly phagocytosis into secretion of a variety of substances that cause differentiation of progenitor cells into mesothelial cells on the injured surface. Mesothelial cells form islands throughout the injured area, proliferate, and cover the denuded area in short periods of time, usually estimated to be within 5 to 7 days of injury.43 It is important to realize that this process occurs, not just at the edge of the denuded peritoneum, but throughout the surface of the injured area. All these cells, as well as fibroblasts that migrate from underlying tissues, release a variety of substances such as plasminogen system components, arachidonic acid metabolites, reactive oxygen species, cytokines, and growth factors such as interleukins, tumor necrosis factor-α, and transforming growth factors α and β. These factors modulate the process of peritoneal healing and adhesion development at different stages.44
Abnormal Repair
Fibroblasts will invade the fibrin matrix with extracellular matrix deposition, leading to peritoneal adhesions. In addition to fibroblast invasion and extracellular matrix deposition, the formation of new blood vessels has been universally claimed to be important in adhesion development as a means of resupplying oxygen and nutrients and removing metabolic waste.44
During peritoneal healing, cell–cell interactions between mesothelial cells, macrophages, and fibroblasts contribute to the healing of the peritoneum. Adhesion fibroblasts have developed a specific phenotype. Compared with normal peritoneal fibroblasts, adhesion fibroblasts have increased basal levels of collagen I, fibronectin, and other adhesion substances and decreased levels of tPA.45 Readers with greater interest in this area of investigation are referred to a more detailed review.46
To conclude, the balance between fibrin deposition and degradation in the initial days after surgery is critical in determining normal peritoneal healing or adhesion development. If fibrin is completely degraded, remesothelialization leading to normal peritoneal healing without adhesions will occur. In contrast, if fibrin is not completely degraded, it will serve as a scaffold for fibroblast ingrowth with subsequent extracellular matrix deposition and angiogenesis. After abdominal surgery and infection, however, the equilibrium between coagulation and fibrinolysis is disturbed in favor of the coagulation system.47–50
Risk Factors for Developing Adhesions
As mentioned earlier, peritoneal repair and adhesion development is the net result of a balance between fibrin deposition as an outcome of the inflammatory process associated with peritoneal injury and fibrinolysis. Fibrinolysis plays a central role in the resolution of the inflammatory exudate, thereby minimizing the risk of adhesion development. This process has primarily been thought to be initiated by mesothelial cells in the region of tissue injury because fibrinolytic activity has been documented within normal mesothelium.51 However, tPA occurs in fibroblasts from human peritoneum and adhesions as well.52,53 Adequate blood supply is critical for normal fibrinolysis to occur. Peritoneal injury associated with ischemia interferes with fibrinolysis and leads to organization rather than resolution of the fibrin–cellular matrix.43 In the absence of ischemia, even large denuded areas of peritoneum usually will heal normally without developing adhesions.54,55
Agents that compromise blood flow within the area of tissue injury increase adhesion development. Thermal injury,56 infection,57 foreign body reaction (i.e., suture),57,58 radiation-induced endarteritis,59 and any other impediment to fibrin degradation increase intraperitoneal adhesions. The effect of electrocautery devoid of significant thermal injury or incomplete hemostasis on fibrinolysis and ultimately on adhesion development has not been adequately studied. Thus, the necessity to control small bleeding vessels and the optimal method to do such (cautery or suture) has yet to be defined. Only conflicting reports concerning these issues exist in the infertility literature.56,60 Fibrinolysis in the abdominal cavity is even more depressed in the presence of infection.61
Intraoperative tissue damage, infections, tissue ischemia, and intra-abdominal presence of foreign material, blood, or bile62,63 all have been shown to be potent causes of peritoneal adhesions. Foreign materials, such as glove powder,64 fluff from surgical packs (gauze lint),65 sutures,58,66 and material extruded from the digestive tract, cause a peritoneal inflammatory reaction, hence increasing the chance of adhesions.67
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









