- Patients should be considered for liver transplantation if they have evidence of fulminant hepatic failure, a life-threatening systemic complication of liver disease, or a liver-based metabolic defect.
- Organ allocation is currently based on a risk-projection system using the Model for End-stage Liver Disease (MELD) score, which accurately predicts short-term mortality of patients while waiting for a transplant.
- Transplantation of patients with low MELD score (<15) has been associated with higher mortality than would be expected without transplantation and is not the ideal use of donor organs.
- Evaluation includes a detailed assessment to make sure that transplantation is technically feasible, medically appropriate, and in the best interest of both the patient and society.
End-stage liver disease (ESLD) is a major health problem worldwide. It has become clear over the last two decades that liver transplantation (LT) is an effective and life-saving intervention for patients with ESLD. Thomas E. Starzl performed the first liver transplantation in 1963, in a 3 year old with biliary atresia.1,2 Since that landmark case, continuous advances in surgical techniques, intensive care, and immunosuppression, have permitted LT to evolve into an effective and widely accepted therapy for adults and children with ESLD. The advent of cyclosporine A in 1978 transformed the field and allowed LT to become standard-of-care therapy for patients with end-stage liver failure. The survival outcome of LT recipients has significantly improved over the last decade. According to the US Organ Procurement and Transplantation Network (OPTN)/Scientific Registry of Transplant Recipients (SRTR) data, the 1-year patient survival rate is 83–91%, and 5-year patient survival is also excellent, ranging from 82 to 84%. The Studies in Pediatric Liver Transplantation (SPLIT) Research Group is another important source of data regarding pediatric LT in North America, now representing 46 pediatric LT centers across the USA and Canada and reflects the results of programs with a strong pediatric emphasis. According to the SPLIT data, patient and graft survival mirrors OPTN/SRTR results, with the most recent review of the SPLIT database revealing patient survival rates of 91.4% and 86.5% at 1 and 5 years post pediatric LT, respectively.
As a result of the excellent survival outcome, the number of patients awaiting LT had grown proportionally. The transplant community is currently faced with a major organ shortage, which has led to the establishment of guidelines for selection of the candidates keeping in view that LT is potentially a life-saving operation yet with limited resources. This chapter will provide an overview of the indications and contraindication for LT for both adults and children.
Indications for Liver Transplantation in Adults
Patients should be considered for LT only if the procedure is considered to extend their life expectancy beyond the natural history of the liver disease. Today organ allocation is essentially based on a risk-projection system using the Model for End-stage Liver Disease (MELD) score or Pediatric End-stage Liver Disease (PELD) score for candidates younger than 12 years.3 This mathematical regression model, which incorporates serum creatinine, bilirubin, and prothrombin time (INR), allows accurate prediction of short-term mortality of the patients waiting for a transplant. The formula for the MELD score and 3-month mortality is available on the Internet at www.mayoclinic.org/meld/mayomodel6.html. Calculated MELD scores range from 6 to 40. Transplantation of patients with low MELD score (<15) has been associated with higher mortality after transplantation than would be expected without transplantation on the waiting list, indicating that transplantation of patients with low MELD score is not the ideal use of the donor organs.4
Since the MELD score is based on short-term mortality risk, it might not be appropriate for some patients who are not at imminent risk of death but nonetheless derive benefit from LT. The best example is the patient with compensated cirrhosis and hepatocellular carcinoma (HCC). Although the risk of death within 6 months might be quite low, the chance that the tumor might progress and therefore preclude LT is reasonably high. Thus, patients with stage T2 HCC are provided an exception score that offers them a reasonably high chance of receiving an organ offer before their tumor progresses to a point that would require them to be removed from the transplant waiting list.
Patients should be considered for LT if they are thought to be capable of surviving the perioperative period, that is have no competing comorbidities and complying with the follow-up post LT, including refrain from addictive behavior such as recidivism of alcohol or drug abuse. To qualify for listing, the patients expected survival rate should be 90% or more within the first year post LT. Referral for LT evaluation should be considered for irreversible hepatic failure regardless of cause, complications of decompensated cirrhosis, liver cancers, or liver-based metabolic conditions causing systemic disease. As a general rule, the following complications of cirrhosis warrant LT:
- recurrent variceal bleeding
- intractable ascites
- following first episode of spontaneous bacterial peritonitis
- refractory encephalopathy
- hepatorenal syndrome.
The common etiologies and indications for LT in adults are presented in Table 9.1. Cirrhosis accounts for more than 80% of transplants performed in adults. The most important indications for LT in the North America are hepatitis C (30%), alcoholic liver disease (10–20%), cholestatic liver disease including primary biliary cirrhosis and sclerosing cholangitis (17%). Other indications are chronic hepatitis B, generally only when complicated by HCC, autoimmune hepatitis, metabolic disease (Wilson disease, hereditary hemochromatosis, and α1-antitrypsin deficiency), vascular disease (Budd–Chiari syndrome), fulminant hepatic failure (5–6%), and non-metastatic HCC.
Table 9.1 Indication for liver transplantation in adults
| Primary diagnosis | Frequency (%) |
| Viral hepatitis (not complicated by HCC) hepatitis C virus hepatitis B virus | 30–40 |
| Alcohol | 10–15 |
| Non-alcoholic steatohepatitis (NASH) | 10 |
| Cholestatic liver diseases Primary sclerosing cholangitis, primary biliary cirrhosis | 15 |
| Metabolic disease Wilson disease, α1-antitrypsin deficiency, tyrosinemia, cystic fibrosis, etc. | 5 |
| Acute liver failure | 10 |
| Liver tumors | 10 |
| Other | 10 |
For alcoholic liver disease, the prerequisites for transplantation in most centers are alcohol abstinence for at least 6 months, assessment by an addiction specialist, and active treatment for alcohol dependency prior to transplantation.5 The rational for requiring a period of 6 months abstinence before liver transplantation is based on: (1) ensuring that the patient’s liver will not recover sufficient function as a result of abstaining from alcohol; and (2) identifying the patients who are at high risk for recidivism.
In patients who experience a relapse, the pattern of drinking post transplantation is variable, but patients who return to occasional drinking rarely experience graft loss. A minority of patients return to abusive drinking, which may result in graft loss and decreased survival.6
Hepatitis C virus (HCV) remains a leading cause of end-stage liver disease but recurrence following LT is universal and often follows an accelerated post-transplant course and the issue of retransplanting patients with graft failure remains controversial. As a result, long-term survival of patients who undergo transplantation for chronic hepatitis C is inferior to that of patients who undergo transplantation for other indications. Patients can be treated for HCV after LT; however, the rate of response to antiviral therapy is usually lower than when instituted pretransplantation.
In contrast, availability of prophylactic therapies for hepatitis B virus has revitalized liver transplantation for this indication. Viremic individuals with cirrhosis due to hepatitis B were not eligible for transplantation in the past because of the high risk of recurrence after transplantation, with consequent rapid graft loss. Since the availability of antiviral medication, all degrees of viremia are treatable and transplantation has become a more realistic option with excellent graft and patient survival, which is even superior to that of many other indications. In those with chronic hepatitis B, liver transplant is almost always needed for complicating HCC now that their “hepatitis” can be controlled.
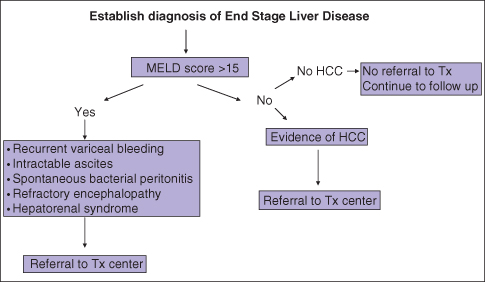
Fulminant hepatic failure or rapid onset of coagulopathy, jaundice, hepatic encephalopathy leading to coma, in patients without history of liver diseases is an indication for LT after the onset of stage 2 encephalopathy. Transplantation indications are usually based on King’s College criteria,7 and/or Clichy8 criteria. Timely referral of these patients to the transplant center is critical since death from sepsis and/or cerebral edema may occur within days of onset of stage 3 or 4 hepatic encephalopathy (Fig. 9.1).
Fig. 9.1 Proposed algorithm for referral of the patient with end-stage liver disease to a transplant center.
Contraindications for Liver Transplantation in Adults
Table 9.2 provides some absolute and relative contraindications to LT accepted by most programs. Absolute contraindications are conditions where the outcomes of liver transplantation are so poor that it should not be offered. Relative contraindications are conditions that have a negative impact on survival, but not to the extent that the patient should be categorically withheld.
Table 9.2 Contraindication for liver transplantation in adults
| Absolute contraindications |
| Uncontrolled systemic sepsis |
| Severely advanced cardiopulmonary disease |
| Extrahepatic malignancy |
| Active alcohol or substance abuse |
| Inability to comply with immunosuppression protocols due to psychosocial situation |
| Multisystem organ failure |
| Relative contraindications (needing individual evaluations) |
| Advanced age > 70 years |
| Infection with human immunodeficiency virus (HIV) |
| Significant anatomic anomalies such as portal vein thrombosis extending throughout the mesenteric venous system |
Advanced age (>70 years old) and individuals infected with HIV in the absence of acquired immune deficiency syndrome are currently considered as relative contraindication for liver transplantation.
Indications for Liver Transplantation in Children
The most common clinical presentations prompting transplant evaluation in children are:9,10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







