and Andrea Bischoff1
(1)
Pediatric Surgery, Colorectal Center for Children Cincinnati Children’s Hospital, Cincinnati, OH, USA
26.1 The Kraske Operation
26.7 Urethral Tumors
26.9 Rectal Tumors
26.10 Presacral Masses
26.11 Surgical Technique
26.1 The Kraske Operation
Early in our experience with the posterior sagittal approach, used for the repair of anorectal malformations (1980), we frequently heard colleagues/surgeons saying that the approach that we were using was not different from what a German surgeon by the name of Kraske had done many years before during the nineteenth century. In reality, when we started using the posterior sagittal approach to repair anorectal malformations, we had not heard of such a procedure, and we were not familiar with the name Kraske. Driven by curiosity, years later, we decided to go into the old medical and surgical literature looking for the original publication of Dr. Kraske [1, 2]. Our findings in such a review were totally unexpected.
We found multiple old papers referring to different types of “posterior approaches” used to treat prostatic and rectal rumors. However, many of them were not midline transsphincteric. In other words, many surgeons made a parasacral incision and dissected the rectum laterally to have access to the urogenital tract.
Table 26.1 shows a summary of our findings. In 1874, a doctor by the name of Verneuil proposed a coccygectomy in order to resect rectal tumors [3]. In 1875, Kocher supported the idea of Verneuil [4]. Then, to our surprise, we found the publication of Dr. Cripps in 1876, obviously the first comprehensive paper on the resection of 36 malignant rectal tumors using a posterior sagittal incision, dividing the entire sphincter mechanism [5, 6]. This means that if we want to use an eponym for the posterior sagittal approach, we should rather use the name Cripps who deserves the credit for the first midline transsphincteric incision.
Table 26.1
History of the posterior approach
Verneuil | [3] | 1874 | Coccygectomy |
Kocher | [4] | 1875 | Supported the idea |
Cripps | 1876 | Division sphincters (36 cases, CA) | |
Allingham | [7] | 1879 | Same plus colostomy |
Kraske | 1885 | Same plus partial removal of sacrum | |
Bevan, Arthur | 1917 | United States, complete division of sphincters |
Subsequently, Allingham in 1879 proposed the same incision, for the treatment of tumors, plus the use of a colostomy [7]. Interestingly, the name Kraske appeared much later in the literature in 1885 [1, 2], but actually even when he supported the use of a posterior incision, he actually used a paramedian one, resecting part of the sacrum and did not propose to divide the entire sphincter mechanism; therefore, the Kraske approach is not a real posterior sagittal transsphincteric incision.
In 1917, Dr. Arthur Bevan from Chicago proposed for the first time in the United States a complete division of the sphincters in order to resect rectal tumors [8, 9].
Table 26.2 shows a list of surgeons that used the transsphincteric approach to the rectum for the treatment of rectal tumors through history [5–20]. The names Cripps, Bevan, Kilpatrick, and Mason are underlined, because they presented the most comprehensive series of cases. Kilpatrick apparently was a urologist, who worked together with Dr. York Mason in England, and they have the largest series of transsphincteric approach used in adults.
Table 26.2
Transsphincteric posterior approach to the rectum
Cripps | 1876 | England | |
Bevan | 1917 | United States | |
David | [10] | 1943 | United States |
Larkin | [11] | 1959 | United States |
Kilpatrick | [12] | 1969 | Urol. England |
Beneventi | [13] | 1971 | Urol. New York |
Oh | [14] | 1972 | New York |
Mason | [15] | 1972 | England |
Dahl | [16] | 1974 | Urol., Salt Lake |
Henderson | [17] | 1981 | Urol., Salt Lake |
Criado | [9] | 1981 | Baltimore |
Westbrook | [18] | 1982 | Arkansas |
Madsen | [19] | 1987 | Denmark |
Jorge | [20] | 1987 | Pennsylvania |
It is important to mention that all of these authors were adult surgeons that used the transsphincteric approach for the treatment of rectal tumors. We could not find a publication prior to ours, in 1982, indicating that this approach has been used for children and/or for the treatment of anorectal malformations. Apparently the posterior transsphincteric approach for the treatment of tumors is no longer popular, most likely due to the fact that those patients suffered from a significant morbidity, and in addition, modern techniques allowed to treat those conditions in a less invasive manner and with less morbidity.
Because of our experience with the posterior sagittal approach, some colleagues referred to us patients suffering from different problems, unrelated to anorectal malformations. These included urogenital sinus with and without adrenal hyperplasia, vaginal or urethral fistula, and different kinds of sequelae from trauma. What all those conditions had in common was the fact that the location of the defect or tumor was difficult to access through the abdomen or through the perineum. We thought that a possible alternative could be a posterior sagittal, transsphincteric, trans-anorectal approach that will give us access to the urogenital tract. Prior to trying this approach in human beings, we performed an experimental study to be sure that this surgical approach will not affect the bowel control of the patients, since most of them had normal anorectum and normal bowel control [21]. The study in animals demonstrated that the trans-anorectal approach did not affect bowel control.
26.2 Urogenital Sinus with Normal Rectum
This particular malformation occurs more often associated to adrenal hyperplasia. Our experience has been mainly in cases without adrenal hyperplasia. This is a rather infrequent condition. Figure 26.1 shows a diagram of the sagittal view of a patient suffering from this malformation. The rectum is normal, is well located, and has a normal sphincter mechanism. The vagina is connected to the urethra, creating a urogenital sinus of different lengths. The malformation occurs in the form of a spectrum. In other words, we have seen patients with a very short common channel (low implantation of the vagina) (Fig. 26.1a) as well as cases with a higher junction of the vagina and urethra (Fig. 26.1b), including connections directly into the bladder, or even more complex, creating a single vesicovaginal chamber. Figure 26.2a shows a radiologic study consisting of the injection of contrast material into the bladder and into the vagina. Figure 26.2b, c shows and MRI study of a urogenital sinus. The length of the common channel, as mentioned when cloacas are discussed, can only be measured accurately endoscopically (cystoscopy).
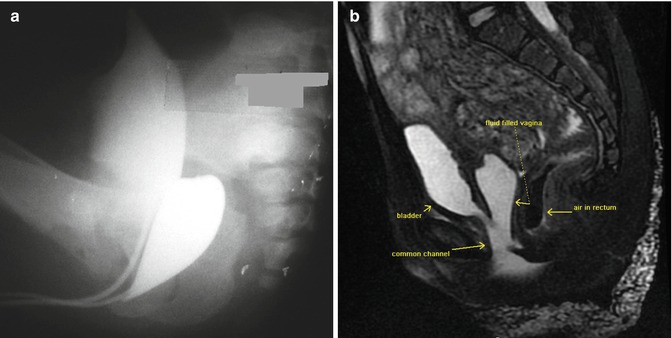
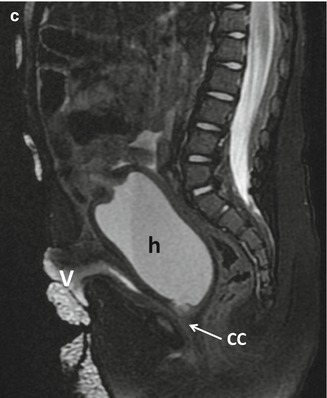
Fig. 26.1
Diagram shows a urogenital sinus with normal rectum. (a) Short common channel. (b) Long common channel
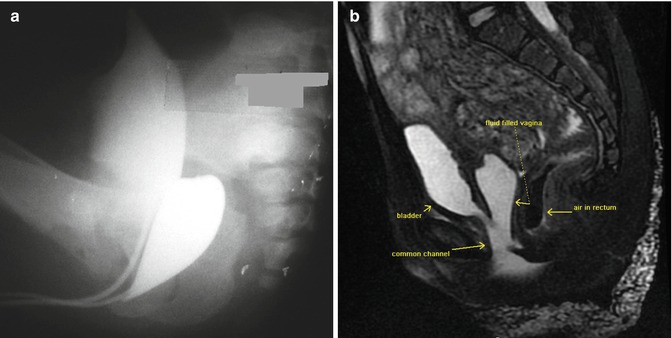
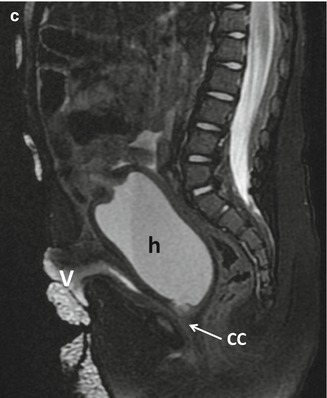
Fig. 26.2
Cystovaginogram of a patient with a urogenital sinus. (a) Short common channel. (b) MRI study of a urogenital sinus with long common channel. (c) MRI study of a urogenital sinus with hydrocolpos, h hydrocolpos, v vesicostomy, cc common channel
There are many publications describing different ways to repair urogenital sinus. Most publications are related to cases of adrenal hyperplasia. Significant contributions were made by very distinguished surgeons [22–30]. Those techniques are still useful, mainly to repair urogenital sinus with a short common channel (less than 3 cm).
The trans-anorectal approach is an excellent way to expose areas of the pelvis that are otherwise difficult to approach abdominally or perineally [31–33]. Figure 26.3 shows the incision that we used for the trans-anorectal approach of a urogenital sinus. In the figure, the patient is placed in the prone position, and the incision runs from the middle portion of the sacrum, passing through the anus itself, and continues all the way down to the single urogenital orifice. Figure 26.4 shows the external appearance of the perineum of a patient with a urogenital sinus in the prone position. A midsagittal incision is performed using a needle-tip cautery, changing from cutting to coagulation, to provide meticulous hemostasis. The incision continues through the skin, subcutaneous tissue, parasagittal fibers, muscle complex, and levator mechanism until we identify the posterior rectal wall. The posterior rectal wall is divided, placing silk temporary sutures, one in front of the other, in corresponding locations of the rectum edges in order to identify them during the reconstruction of the rectum and the sphincter mechanism. The incision continues dividing the anterior rectal wall and the sphincter mechanism, anterior to the anal opening, and runs all the way to the single orifice in the perineum until we identify the posterior wall of the urogenital sinus. Figure 26.5 shows a diagram of the incision, and the arrows show the posterior and anterior limits of the anal sphincter. Figure 26.6 shows an intraoperative view of the same stage of the operation, and again, the arrows show the anterior and posterior limits of the sphincter. The posterior wall of the urogenital sinus is divided exactly in the midline to expose the common channel, the urethral orifice, and the vaginal orifice. A Foley catheter is introduced into the bladder. Figure 26.7 shows a diagram of the anatomic findings. Figure 26.8 shows a photograph of the intraoperative findings after the urogenital sinus has been opened.

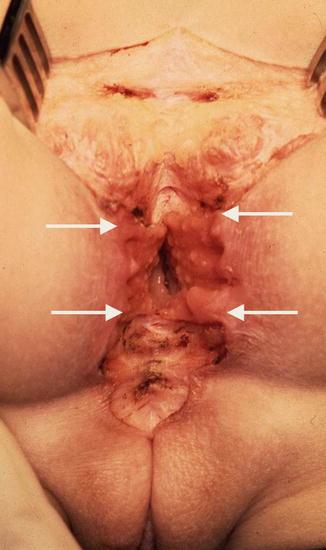
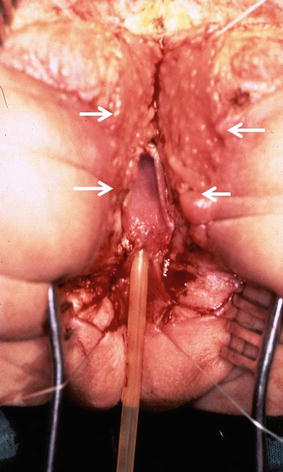
Fig. 26.3
Diagram showing the incision used for the trans-anorectal approach of a urogenital sinus

Fig. 26.4
External appearance of the perineum of a patient with a urogenital sinus
Fig. 26.5
Diagram showing the trans-anorectal incision (the arrows show the anterior and posterior limits of the sphincter)
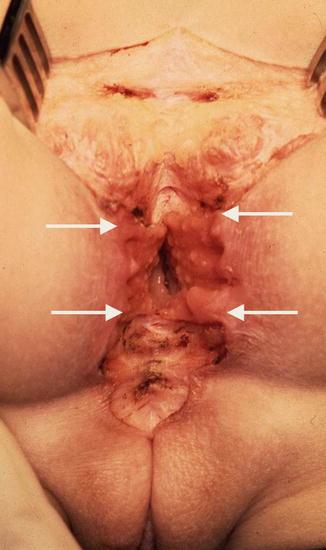
Fig. 26.6
Intraoperative appearance of the trans-anorectal approach (the arrows show the anterior and posterior limits of the sphincter), the arrows show the limits of the sphincter
Fig. 26.7
Diagram showing the anatomy of the urogenital sinus, after the posterior wall of the sinus has been divided, a Foley catheter is introduced through the urethra. Arrows show the limits of the sphincter
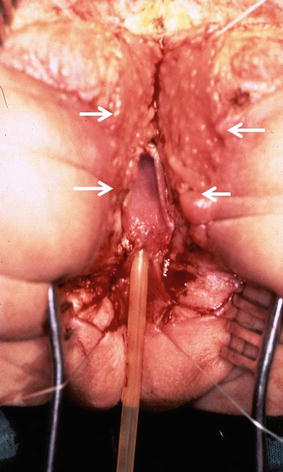
Fig. 26.8
Intraoperative view of the anatomy. Arrows show the limits of the sphincter
Prior to the use of the maneuver called “total urogenital mobilization,” the repair of this defect consisted in separating the vagina from the urinary tract (Figs. 26.9 and 26.10). Once the vagina was separated and mobilized enough to reach the labia with no tension, the urethra was reconstructed, using what used to be the common channel (Fig. 26.11). The vagina was pulled down behind the urethra and sutured to the neolabia. The anorectum and anterior and posterior sphincter mechanism are reconstructed (Fig. 26.12).
Fig. 26.9
Diagram showing the separation of the vagina from the urinary tract
Fig. 26.10
Vagina completely separated from the urinary tract and mobilized enough to reach the perineum. (a) Diagram. (b) Operative
Fig. 26.11
Diagram showing the urethra reconstructed using the original common channel
Fig. 26.12
Diagram showing the reconstructed vagina, perineal body, sphincter mechanism anterior to the rectum, and anterior rectal wall. The posterior rectal wall was closed using two layers of interrupted long-term absorbable sutures. The sphincter mechanism posterior to the anus is meticulously re-approximated
In 1997, we described a maneuver called “total urogenital mobilization” [34], in an attempt to simplify the repair of cloacas. This maneuver turned out to be very useful to repair cloacas with common channels shorter than 3 cm. As a natural consequence of this, we decided to repair urogenital sinuses with a normal rectum, using a transanal approach combined with the total urogenital mobilization (see Chap. 16, Sect. 16.1.1.4 on cloacas).
The total urogenital mobilization was well received by many surgeons [35–39]. However, as expected, some surgeons, mainly urologists, voiced their concerns about the trans-anorectal approach. Consequently, some of them decided to do the total urogenital mobilization, but not perform the full trans-anorectal approach, but rather to divide only the anterior portion of the sphincter and anorectum [40, 41] or perform the mobilization without touching the anus [42, 43]. Also, a limited urogenital mobilization was described [44]. We agree with the basic idea of being as less invasive as possible, but we also believe that we should not hesitate to divide the rectum and anus, in order to achieve our goal of performing an adequate anatomic repair.
Figure 26.13 shows the operative field of a urogenital sinus. We started that particular case with an incision that included the sphincter mechanism located anterior to the anus. We tried to mobilize the urogenital sinus, as much as possible without opening the rectum (Fig. 26.13a). We then found that exposure was not good enough to achieve a satisfactory mobilization, and therefore we elected to divide the entire anorectum in the midline. Figure 26.13b shows the improved exposure achieved with the full trans-anorectal approach. The total urogenital mobilization is performed with a magnificent exposure. The suspensory ligaments of the urethra and vagina are divided. By doing that, we gained enough length to bring the urethra and vagina down (Fig. 26.13c, d). What used to be the common channel is divided in the midline, creating two flaps that will be sutured to the neolabia. The urethral meatus is sutured a few millimeters behind the clitoris (Fig. 26.13e). Figure 26.14 shows the final external appearance.

Fig. 26.13
Intraoperative view of the repair of a urogenital sinus. (a) An attempt is made to mobilize the urogenital sinus, with a limited incision, trying not to open the rectum. The exposure is limited. (b) Improved exposure after extending the incision through the anus and rectum. R divided rectum, u urogenital sinus. (c) Operative picture of a case with a short common channel. It was possible to mobilize the urogenital sinus without dividing the rectum. (d) Operative picture showing a total urogenital mobilization. The urethra and vagina have been fully mobilized. (e) Operative picture. The urethral meatus is sutured a few millimeters behind the clitoris

Fig. 26.14
Final external appearance
We must always keep in mind that we are dealing with a spectrum of defects, and therefore, the surgeon must be prepared to implement different surgical maneuvers, adequate for each one of the anatomic variants of the malformation that we deal with. For very low vaginal-urethral confluence, the surgeon can use any technique, because the repair is relatively easy. On the other hand, for cases with extremely high implantations of the vagina, such as vaginovesical communication, the transabdominal approach represents the ideal way to do it. In the middle of those extremes are malformations shown in these diagrams with common channels that vary from 2 to 4 cm.
The size of the vagina is also another important factor. Some patients with this type of urogenital sinus also have hydrocolpos, like in the patients with cloacas. The presence of hydrocolpos, of course, must alert the surgeons about the possibility of megaureters and hydronephrosis (see chapters on cloacas). However, the presence of hydrocolpos also means that the surgeon has more vaginal tissue to work with and more chances to bring the vagina down. Patients with very small vaginas and long common channels represent a challenge and may require a partial vaginal replacement.
The first trans-anorectal operations performed by us included a protective colostomy. Subsequently, as we gained confidence in these kinds of techniques, we performed the same operations without a colostomy. We followed the same strict rules of bowel preparation (see chapter on bowel preparation). The patients remained 7–10 days with nothing by mouth, receiving parenteral nutrition; our patients did not have infections, dehiscence, or other kinds of complications.
Our current way to approach these patients is to determine the length of the common channel endoscopically. For those that are extremely long common channels (vaginovesical fistula), we prepare the patient to be approached through the perineum and also through the abdomen. In addition some of those patients may require a partial vaginal replacement. If we believe that the patient can be treated trans-anorectally without a laparotomy (common channel between 2 and 4 cm), we prepared the bowel as described and take the patient to the operating room. We start by making an incision running from the anus to the urogenital sinus, trying not to open the rectum and see if it is possible to do the total urogenital mobilization without dividing the anterior rectal wall or the posterior rectal wall (Fig. 26.13a). Sometimes this is feasible, but if we feel uncomfortable about the exposure, we do not hesitate to divide first the sphincter mechanism located anterior to the anus or even the posterior rectal wall and the posterior sphincter mechanism (Fig. 26.13b).
The trans-anorectal approach consists in dividing the anus and the rectum exactly in the midline. By doing that, we obtain a magnificent exposure to the urogenital tract. However, the procedure requires a meticulous bowel preparation or a colostomy, followed by a delicate, scrupulous technique with special attention to details.
Our experience with the repair of a urogenital sinus with normal rectum includes 16 cases. We are extremely happy, because bowel control has been normal in all of them. The patients also showed evidence of urinary control. None of our patients reached the age of sexual function, and therefore, we cannot comment on that. However, we expect them to have an examination under anesthesia at the age when they expect to become sexually active. We will not be surprised to find that they may need an external introitoplasty like we do in patients with cloaca, because they have a ringlike fibrous band that may interfere with satisfactory sexual activity and may require a small operation to take care of that.
26.3 Urogenital Sinus with Normal Rectum and Adrenal Hyperplasia
We have used the same approach in patients with adrenal hyperplasia. However, we must admit that these groups of patients (with virilization) are more difficult to repair. First of all, they require a clitoral recession. In spite of doing that procedure, one deals with the presence of hypertrophic corpora that makes the operation technically more difficult. In addition, the vagina in those types of patients is usually much smaller, both in length and diameter. All of that makes the operation technically more demanding. Our experience with this group of patients is limited to three cases, and therefore, we cannot claim that this is the ideal way to repair this malformation.
26.4 Acquired Urethral Atresia
Male patients, who suffer from severe pelvic trauma, frequently have severe urethral injuries that result in an acquired atresia of the posterior urethra. These represent a surgical challenge, not only to be able to reconnect both ends of the posterior urethra, but also to try to obtain urinary control after the repair.
Traditional approaches to this problem include perineal operations [45–49] or transpubic approach [50–56]. We have a modest but significant experience with the trans-anorectal approach that has also been used by others [57–60].
Six patients have been referred to us suffering from this type of problem. These patients underwent several previous attempts to repair, using a perineal approach, and all of them were unsuccessful. Figure 26.15a shows a cystogram and urethrogram of one of these patients. The gap between the blind ends measures over 3 cm. This study was done injecting contrast material through a suprapubic tube and simultaneously through the urethral meatus. This was an adult patient who suffered a very severe pelvic trauma that destroyed the posterior urethra. The patient was ejaculating through the suprapubic tube and had three previous failed attempts to repair the problem. Figure 26.15b shows a diagram trying to show the anatomy of the same patient. In addition to the disruption of the posterior urethra, the patient also had a mild stenosis of the penile urethra. The subset of the figure shows the trans-anorectal incision used to approach this urethra.
Fig. 26.15
Disrupted posterior urethra, a mild penile urethral stricture and the trans-anorectal incision. (a) Diagram. (b) Contrast study – injection of contrast done through a suprapubic tube and through the penis
A posterior sagittal trans-anorectal incision is done, dividing, as previously mentioned, the sphincter mechanism posterior to the anus, as well as the anterior one, dividing also the posterior and anterior rectal walls. Figure 26.16 shows a picture of the intraoperative aspect of the trans-anorectal incision. Both posterior and anterior rectal walls have been divided. Figure 26.17 is a diagram showing both blind ends of the urethra deep in the operative field. Multiple fine silk sutures are placed in each end of the urethra in order to apply uniform traction and mobilize them to be able to create a non-tense end-to-end anastomosis. Figure 26.18 shows both urethral ends already open and with the silk sutures placed. The gap between both ends is about 3 cm, and therefore both sides require a significant mobilization. Figure 26.19 shows after the mobilization both urethral ends come together, the anterior wall has been already sutured, a Foley catheter is passed through the penis into the bladder, and the final step is the reconstruction of the posterior urethral wall. Reconstructing the perineal body as well as the rectum will complete the operation (Fig. 26.20). Figure 26.21 shows the reconstruction suturing of the anterior rectal wall with two layers of fine, long-term absorbable sutures. The reconstruction of the anterior rectal wall must be done simultaneously with the reconstruction of the sphincter. Figure 26.22 shows the completion of the urethral suturing, perineal body reconstruction, as well as the sphincter mechanism and rectum. The perineal body is already reconstructed, as well as the sphincter mechanism anterior to the rectum and the anterior rectal wall. The next step will be to suture the posterior rectal wall and to approximate meticulously the sphincter mechanism posterior to the anus and rectum. Figure 26.23 shows a diagram of the completed operation. The patient shown in this diagram has urinary control, as well as sexual function. However, when dealing with this kind of severe pelvic trauma, one cannot guarantee good functional results in all patients because each patient suffers from a trauma of a different magnitude. Two of our six patients suffered from postoperative urinary incontinence and required another type of urinary reconstruction, including the closure of the bladder neck. More recently, the anatomy of these complex conditions can be elucidated better by the use of a three-dimensional rotational scan, which provides excellent images, like one shown in Fig. 26.24. That patient was also approached trans-anorectally, and Fig. 26.25 shows the intraoperative findings, as well as the reconstruction of the urethra. The patient also has urinary control.

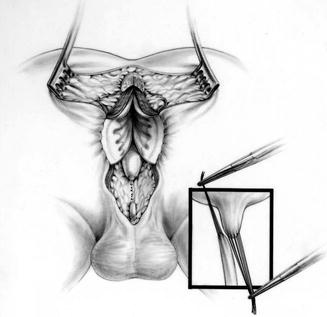
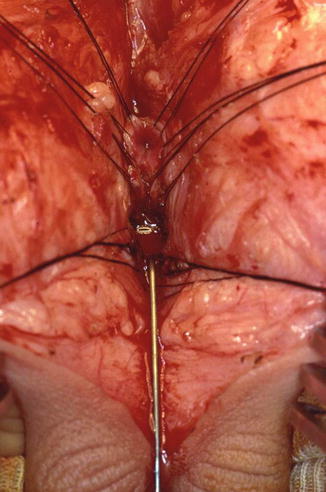

Fig. 26.16
Intraoperative aspect of the trans-anorectal approach. Both posterior and anterior rectal walls have been divided. The urethral ends will be found deep in the incision
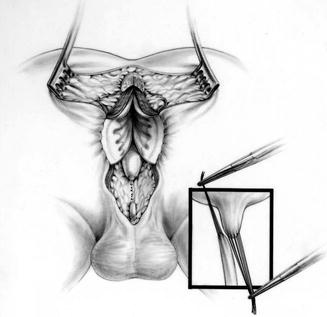
Fig. 26.17
Diagram showing both urethral blind ends. Multiple fine silk sutures are placed in both ends to mobilize them
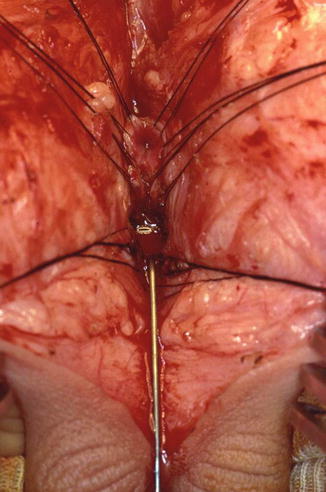
Fig. 26.18




Operative field showing both urethral ends open. The distal one has a metallic sound
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








