Vesicoureteral Reflux: Introduction
Under normal circumstances, the ureterovesical junction allows urine to enter the bladder but prevents urine from regurgitating into the ureter, particularly at the time of voiding. In this way, the kidney is protected from high pressure in the bladder and from contamination by infected vesical urine. When this valve is incompetent, the chance for development of urinary infection is significantly enhanced, and pyelonephritis may occur. In significant cases especially in children, pyelonephritis—acute, chronic, or healed—is secondary to vesicoureteral reflux (VUR).
Anatomy of the Ureterovesical Junction
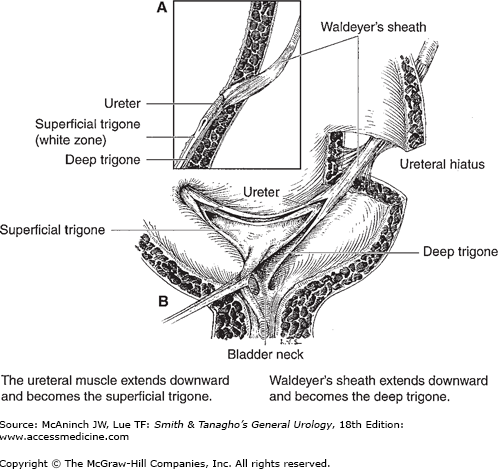
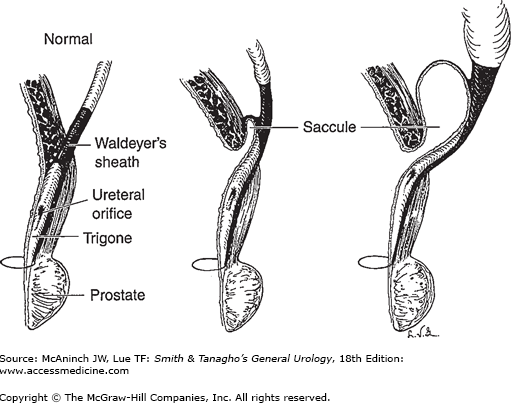
An understanding of the causes of VUR requires knowledge of the anatomy of the ureterovesical valve. Anatomic studies performed by Hutch (1972) and by Tanagho and Pugh (1963) (Figure 13–1) are incorporated into the following discussion.
Figure 13–1.
Normal ureterotrigonal complex. A: Side view of ureterovesical junction. Waldeyer’s muscular sheath invests the juxtavesical ureter and continues downward as the deep trigone, which extends to the bladder neck. The ureteral musculature becomes the superficial trigone, which extends to the verumontanum in the male and stops just short of the external meatus in the female. B: Waldeyer’s sheath is connected by a few fibers to the detrusor muscle in the ureteral hiatus. This muscular sheath, inferior to the ureteral orifices, becomes the deep trigone. The musculature of the ureters continues downward as the superficial trigone. (Redrawn and modified, with permission, from Tanagho EA, Pugh RCB: The anatomy and function of the ureterovesical junction. Br J Urol 1963;35:151.)
The mesodermal component, which arises from the Wolffian duct, is made up of two parts that are innervated by the sympathetic nervous system:
The smooth musculature of the renal calyces, pelvis, and extravesical ureter is composed of helically oriented fibers that allow for peristaltic activity. As these fibers approach the vesical wall, they are reoriented into the longitudinal plane. The ureter passes obliquely through the vesical wall; the intravesical ureteral segment is thus composed of longitudinal muscle fibers only and therefore cannot undergo peristalsis. As these smooth-muscle fibers approach the ureteral orifice, those that form the roof of the ureter swing to either side to join those that form its floor. They then spread out and join equivalent muscle bundles from the other ureter and also continue caudally, thus forming the superficial trigone. The trigone passes over the neck of the bladder, ending at the verumontanum in the male and just inside the external urethral meatus in the female. Thus, the ureterotrigonal complex is one structure. Above the ureteral orifice, it is tubular; below that point, it is flat.
Beginning at a point about 2–3 cm above the bladder, an external layer of longitudinal smooth muscle surrounds the ureter. This muscular sheath passes through the vesical wall, to which it is connected by a few detrusor fibers. As it enters the vesical lumen, its roof fibers diverge to join its floor fibers, which then spread out, joining muscle bundles from the contralateral ureter and forming the deep trigone, which ends at the bladder neck.
The vesical detrusor muscle bundles are intertwined and run in various directions. As they converge on the internal orifice of the bladder, however, they tend to become oriented into three layers.
The internal longitudinal layer continues into the urethra submucosally and ends just inside the external meatus in the female and at the caudal end of the prostate in the male.
The middle circular layer is thickest anteriorly and stops at the vesical neck.
The muscle bundles of the outer longitudinal layer take a circular and spiral course about the external surface of the female urethra and are incorporated within the peripheral prostatic tissue in the male. They constitute the true vesicourethral sphincter.
The vesical detrusor muscle is innervated by the parasympathetic nerves (S2–S4).
Physiology of the Ureterovesical Junction
Although many investigators had suspected that normal trigonal tone tended to occlude the intravesical ureter, it remained for Tanagho et al (1965) to prove it. Using nonrefluxing dogs, they demonstrated the following:
Interruption of the continuity of the trigone resulted in reflux. An incision was made in the trigone 3 mm below the ureteral orifice, resulting in an upward and lateral migration of the ureteral orifice with shortening of the intravesical ureter. Reflux was demonstrable. After the incision healed, reflux ceased.
Unilateral lumbar sympathectomy resulted in paralysis of the ipsilateral trigone. This led to lateral and superior migration of the ureteral orifice and reflux.
Electrical stimulation of the trigone caused the ureteral orifice to move caudally, thus lengthening the intravesical ureter. This maneuver caused a marked rise in resistance to flow through the ureterovesical junction. Ureteral efflux of urine ceased. Intravenous injection of epinephrine caused the same reaction. On the other hand, isoproterenol caused the degree of occlusion to drop below normal. If the trigone was incised, however, electrical stimulation of the trigone or the administration of epinephrine failed to increase ureteral occlusive pressure.
During gradual filling of the bladder, intravesical pressure increased only slightly, whereas pressure within the intravesical ureter rose progressively—owing, apparently, to increasing trigonal stretch. A few seconds before the expected sharp rise in intravesical pressure generated for voiding, the closure pressure in the intravesical ureter rose sharply and was maintained for 20 seconds after detrusor contraction had ceased. This experiment demonstrated that ureterovesical competence is independent of detrusor action and is governed by the tone of the trigone, which contracts vigorously just before voiding, thus helping to open and funnel the vesical neck. At the same time, significant pull is placed on the intravesical ureter so that it is occluded during the period when intravesical pressure is high. During the voiding phase, there is naturally no efflux of ureteral urine.
One may liken this function to the phenomenon of the Chinese thimble: The harder the finger (trigone) pulls, the tighter the thimble (intravesical ureter) becomes. Conversely, a deficient pull may lead to incomplete closure of the ureterovesical junction.
It was concluded from these experiments that normal ureterotrigonal tone prevents VUR. Electrical or pharmacologic stimulation of the trigone caused increased occlusive pressure in the intravesical ureter and increased resistance to flow down the ureter, whereas incision or paralysis of the trigone led to reflux. The theory that ureterovesical competence was maintained by intravesical pressure compressing the intravesical ureter against its backing of detrusor muscle was thereby disproved.
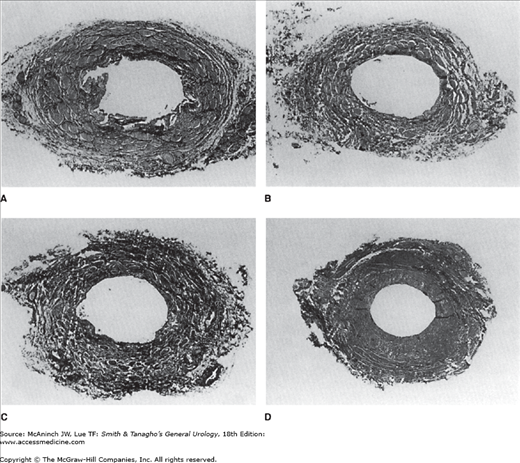
Biopsy of the trigone (and the intravesical ureter) in patients with primary reflux revealed marked deficiency in the development of its smooth muscle (Figure 13–2). Electrical stimulation of such a trigone caused only a minor contraction of the ureterotrigonal complex. This work led to the conclusion that the common cause of reflux, particularly in children, is congenital attenuation of the ureterotrigonal musculature.
Figure 13–2.
Histology of the trigone in primary reflux. Top: Normal trigone demonstrating wealth of closely packed smooth-muscle fibers. Bottom: The congenitally attenuated trigonal muscle that accompanies vesicoureteral reflux. Note the absence of inflammatory cell. (Reproduced, with permission, from Tanagho EA et al: Primary vesicoureteral reflux: Experimental studies of its etiology. J Urol 1965;93:165.)
Vesicoureteral Reflux
The major cause of VUR is attenuation of the trigone and its contiguous intravesical ureteral musculature. Any condition that shortens the intravesical ureter may also lead to reflux, but this is less common. Familial VUR has been observed by a number of authors. It appears to be a genetic trait.
Trigonal weakness is by far the most common cause of ureteral reflux. It is most often seen in young children, more common in girls than in boys. Reflux in adults—usually women—probably represents the same congenital defect. Weakness of one side of the trigone leads to a decrease in the occlusive pressure in the ipsilateral intravesical ureter. Diffuse ureterotrigonal weakness causes bilateral reflux.
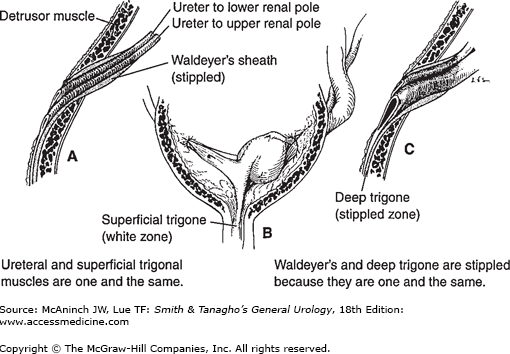
It is postulated that ureteral trigonal weakness is related to the development of the ureteral bud on the mesonephric duct. It is known that the ureter acquires its musculature from its cranial end caudally so that if a segment is muscularly deficient, it is deficient in its most caudal part. It is also postulated that if the ureter is too close to the urogenital sinus on the mesonephric duct, it will join the latter relatively early in embryonic life, before acquiring adequate mesenchymal tissue around itself to be differentiated later into proper trigonal musculature as well as lower ureter. This embryologic hypothesis explains all the known features of refluxing ureters: their muscular weakness, their lateral placement on the bladder base with a very short submucosal segment, and their usual association with weak ureteral musculature and gaping ureteral orifices (which, in severe cases, ensures a golf-hole endoscopic appearance at their junction with the bladder wall). It also explains why, in duplicated systems, if there is only one refluxing unit, it is the upper orifice (which originated closer to the urogenital sinus on the mesonephric duct and thus has the least muscular development).
In the normal state, the intravesical ureterotrigonal muscle tone exerts a downward pull, whereas the extravesical ureter tends to pull cephalad (Figure 13–3). If trigonal development is deficient, not only is its occlusive power diminished but the ureteral orifice tends to migrate upward toward the ureteral hiatus. The degree of this retraction relates to the degree of incompetence of the junction (Figure 13–4). If the ureteral orifice lies over the ureteral hiatus in the bladder wall (so-called golf-hole orifice), it is completely incompetent. The degree of incompetence is judged by the findings on excretory urography and cystography and the cystoscopic appearance of the ureteral orifices.
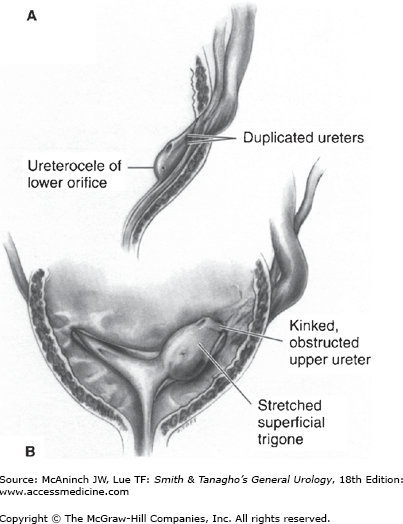
Figure 13–3.
A: Small ureterocele developing in a duplicated system (where it always involves a lower ureteral orifice). B: Expansion of submucosal segment leads to lifting and angulation of ipsilateral lower pole ureteral orifice. Duplicated system ureteroceles are rarely so small. (Diagrammatic representation.) (Reproduced, with permission, from Tanagho EA: Ureteroceles: Embryogenesis, pathogenesis and management. J Cont Educ Urol 1979;18:13.)
Figure 13–4.
Histology of the various grades of submucosal muscular weakness of the ureteral orifice. (See also Figure 13–9.) A: Normal. Minimal deficiency. (Cone orifice.) B: More marked muscular weakness. (Stadium orifice.) C: Marked muscular deficiency. (Horseshoe orifice.) D: Extreme muscular deficiency. Only a few muscle fibers can be seen; the rest is collagen tissue.
There appears to be genetic predisposition for reflux. The reported prevalence of VUR among siblings of index patients with reflux has ranged from 4.7% to 51%, which is significantly higher than the incidence of reflux in the general population (1%) (Ataei et al, 2004). In addition, the incidence of reflux varies among nationalities and races. Studies involving genotype screening of specific subgroups of patients suggest that there is heterogeneity in the genetics of VUR (reviewed by Carvas et al, 2010). Several genes have been associated with VUR, including uroplakin-3, SLIT2/ROBO2, and TGF-β. In addition, several chromosomal regions (on chromosomes 1, 2, 3, 5, 13, and 18) have also been identified. Despite extensive analysis, the exact form of genetic transmission has yet to be delineated.
The intravesical portion of the ureter to the upper renal segment is usually of normal length, whereas that of the ureter to the lower pole is abnormally short; this orifice is commonly incompetent. However, Stephens (1957) demonstrated that the musculature of the superiorly placed orifice is attenuated, which further contributes to its weakness.
Figure 13–5.
Ureteral duplication and ureterocele as causes of vesicoureteral reflux. A: Ureteral duplication showing juxtavesical and intravesical ureters encased in common sheath (Waldeyer’s). The superior ureter, which always drains the lower renal pole, has a shorter intravesical segment; in addition, it is somewhat devoid of muscle. It therefore tends to allow reflux. B: Duplication with ureterocele that always involves caudal ureter, which drains upper renal pole. Pinpoint orifice is obstructive, causing hydroureteronephrosis. Resulting wide dilatation of ureter and ureteral hiatus shortens the intravesical segment of the other ureter, often causing it to reflux. C: Resection of ureterocele allows reflux into that ureter.
Single ureter or one of a pair may open well down on the trigone, at the vesical neck, or in the urethra. In this instance, VUR is the rule. This observation makes it clear that the length of the intravesical ureter is not the sole factor in reflux. Such intravesical ureteral segments are usually devoid of smooth muscle. Thus, they have no occlusive force.
A ureterocele involving a single ureter rarely allows reflux, but this lesion usually involves the ureter that drains the upper pole of a duplicated kidney. Because the ureteral orifice is obstructed, the intramural ureter becomes dilated. This increases the diameter of the ureteral hiatus, further shortening the intravesical segment of the other ureter, which therefore may become incompetent. Resection of the ureterocele usually causes its ureter to reflux freely as well.
Abnormal voiding habits have been associated with reflux. Toilet-trained children, in particular girls, may alter their bladder function by inhibiting their urge to void. This can result in abnormally high voiding pressure, bladder overactivity, and poor bladder compliance. These changes in bladder dynamics can either induce the development of primary reflux or prevent its resolution (Greenfield and Wan, 2000). In addition, alterations in the bowel function (eg, constipation) can cause further deterioration in bladder function and consequently the development or persistence of primary reflux (Bower et al, 2005).
Occasionally, a heavily trabeculated bladder may be associated with reflux. The causes include spastic neurogenic bladder and severe obstruction distal to the bladder. These lesions, however, are associated with trigonal hypertrophy as well; the resultant extra pull on the ureterotrigonal muscle tends to protect the junction from incompetence. In a few such cases, however, the vesical mucosa may protrude through the ureteral hiatus just above the ureter to form a diverticulum, or saccule (Figure 13–6). The resulting dilatation of the hiatus shortens the intravesical segment; reflux may then occur.
Figure 13–6.
Development of ureteral saccule, seen occasionally in cases of primary reflux but more commonly in obstructed or neurogenic bladders with marked trabeculation. Note that the vesical mucosa herniates through the ureteral hiatus, pulling the ureteral orifice upward with it. The orifice may ultimately open in the saccule rather than in the bladder.
As noted previously, valves vary in their degrees of incompetence. A “borderline” junction may not allow reflux when the urine is sterile, but valvular function may be impaired when cystitis causes associated edema involving the trigone and intravesical ureter. In addition, the abnormally high voiding pressure may lead to reflux, in which case, secondary pyelonephritis may ensue. After cure of the infection, cystography again reveals no reflux. It is believed that a completely normal junction will not decompensate even under these circumstances.
It has been shown that pyelonephritis of pregnancy is associated with VUR. Many patients give a history of urinary tract infections during childhood. The implication is that they “outgrew” reflux at puberty, but if bacteriuria becomes established during pregnancy, their “borderline” valves may become incompetent. This condition may be aggravated by the hormones of pregnancy, which may contribute to a further loss of tone of the ureterotrigonal complex. After delivery, reflux is usually no longer demonstrable (Hutch and Amar, 1972).
The Eagle–Barrett syndrome is a relatively rare condition in which there is failure of normal development of the abdominal muscles and the smooth muscle of the ureters and bladder. Bilateral cryptorchidism is the rule. At times, talipes equinovarus and hip dislocation are also noted. Because the smooth muscle of the ureterotrigonal complex is deficient, reflux is to be expected; advanced hydroureteronephrosis is therefore found.
Certain operative procedures may lead to either temporary or permanent ureteral regurgitation.
With any type of prostatectomy, the continuity of the superficial trigone is interrupted at the vesical neck. If the proximal trigone moves upward, temporary reflux may occur. This mechanism may account for the high fever (and even bacteremia) that is sometimes observed when the catheter is finally removed. Fortunately, in 2–3 weeks, the trigone again becomes anchored and reflux ceases.
Preexisting trigonal hypertrophy (due to prostatic obstruction) helps to compensate for the effect of trigonal interruption; thus, reflux may never occur.
Wedge resection of the posterior vesical neck, often ill advised when performed in conjunction with plastic revision of the vesical neck for supposed vesical neck stenosis or dysfunction, may also upset trigonal continuity and allow reflux.
Extensive ureteral meatotomy may be followed by reflux. Fortunately, however, limited incision of the roof of the intravesical ureter divides few muscle fibers, since the fibers have left the roof to join muscle fibers on the floor. Wide resection for treatment of vesical cancer is often followed by ureteral reflux.
If the ureteral hiatus is widely dilated, this procedure is often followed by reflux.
A bladder that is contracted secondary to interstitial cystitis, tuberculosis, radiotherapy, carcinoma, or schistosomiasis may be associated with ureteral reflux.
VUR damages the kidney through one or both of two mechanisms: (1) pyelonephritis and (2) hydroureteronephrosis.
VUR is one of the common contributing factors leading to the development of cystitis, particularly in females. When reflux is present, bacteria reach the kidney and the urinary tract cannot empty itself completely, so infection is perpetuated. Pyelonephritis is discussed in more detail in Chapter 14.
Dilation of the ureter, renal pelvis, and calyces is usually observed in association with reflux (Figure 13–7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree