Chapter 91A Vascular isolation
Overview
Bleeding and subsequent blood transfusions remain important causes of death and morbidity with hepatectomies. Evidence also shows that blood transfusion may be associated with an increased risk of recurrence of malignancy through impairment of the patient’s immune response (Asahara et al, 1999; Tung-Ping Poon et al, 2000). Vascular clamping, irrespective of its modality, minimizes the risk of bleeding during liver resection. Liver cell injury induced by ischemia and reperfusion is the major drawback of clamping. Overall, normal liver tolerates up to an hour of warm ischemia, but diseased liver with fibrosis, steatosis, inflammation, and vascular or biliary disease requires much shorter periods of ischemia. Indeed, the vast majority of liver resections are performed in such diseased livers, including resections of hepatocellular carcinoma (HCC) (see Chapter 70A, Chapter 70B, Chapter 81A ) and of liver metastases, which are more often performed after chemotherapy and can induce parenchymal changes (chemotherapy-associated steatohepatitis, sinusoidal obstruction syndrome) (see Chapters 65 and 81A).
With technical improvements in liver surgery, patients with various underlying liver conditions—such as fibrosis, steatosis, or chemotherapy-induced injury—are undergoing complex and extensive liver resections (Belghiti et al, 2000; Poon et al, 2002). In this regard, pedicular intermittent clamping, which alternates short periods of clamping with intervals of restoration of blood flow, has been shown to be the best tolerated clamping modality, especially in patients with diseased liver parenchyma (Belghiti et al, 1999; Man et al, 1997). Although a real advantage in clinical practice was not demonstrated (Gurusamy et al, 2009), ischemic preconditioning that initiates a short period of clamping and restoration of blood flow followed by continuous clamping is an attractive concept (Clavien et al, 2000). On the other hand, better understanding of vascular anatomy, particularly of the venous tributaries; better anesthesiologic management with perioperative low filling (restrictive fluid administration); and the development of modern tools of transection and coagulation, such as the ultrasonic dissector associated with bipolar coagulation, have made possible even major liver resection without vascular clamping or transfusion. Therefore if vascular clamping must be applied, balancing its efficacy to control bleeding with the potential side effects of ischemic liver injury is vital.
Anatomic Basis for Vascular Control
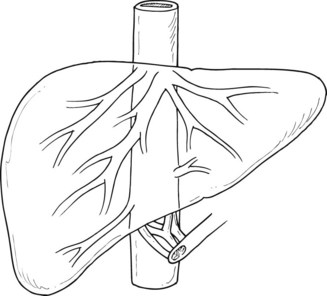
Three large hepatic veins lie posterosuperior to the liver just below the diaphragm and form the major drainage of the liver (Fig. 91A.1). The right hepatic vein is a short, wide trunk formed by the convergence of an anterior trunk situated in the right portal fissure, which drains mainly segments V and VI, and a posterior trunk, which drains mainly segment VII. The right hepatic vein also drains part of segment VIII. The middle hepatic vein is situated in the plane of principal portal fissure; it drains the entire central sector and receives the veins from segments V and VIII at its right border and the veins of segment IV at its left border, thus forming the major drainage vein of segment IV and part of segments V and VIII. The left hepatic vein arises from the confluence of the segment II and III veins. It often receives drainage from the posterior part of segment IV, and it terminates as a short common trunk with the middle hepatic vein in the majority. In 10% to 20% of cases, a significant right inferior hepatic vein may be found (>5 mm diameter), which mainly drains segment VI. In addition to these, there are two groups of accessory hepatic veins, the right and the left. The right accessory veins drain the posterior part of the dorsal sector. On the left, they are formed by the veins of the caudate lobe. In half of the cases, a large solitary vein terminates in the inferior vena cava (IVC); in the other half, two or three veins are present, and they end in a staged fashion in the left border of the IVC. These anatomic variations are important in the context of vascular clamping, as the presence of large drainage veins can result in the inability to achieve complete vascular control during the clamping procedure (see Chapter 1B).
Hemodynamic Response to Different Types of Clamping
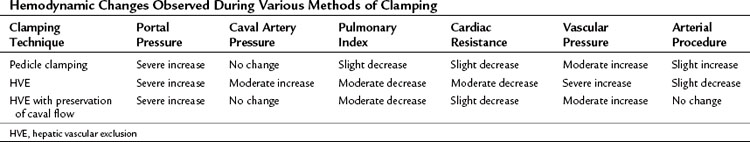
Hemodynamic changes are proportional to the type and extent of vascular interruption. These changes are also related to several factors, including the level of anesthesia, quantity and rapidity of bleeding, vascular filling, and spontaneous adaptation of the circulatory system to the reduction of venous return. Pedicular clamping is nearly always well tolerated, but the addition of caval clamping is more likely to be followed by major hemodynamic consequences (Table 91A.1).
Hemodynamic Response to Pedicle Clamping
The pedicular clamping, which leads to a moderate decrease in cardiac preload with a 5% decrease in pulmonary artery pressure and a 10% decrease in cardiac index, is paradoxically associated with a 10% increase in mean arterial pressure because of a sympathetic reflex after arterial clamping that induces a significant increase in systemic vascular resistance (Delva et al, 1987). Therefore isolated pedicle clamping is usually well tolerated and does not require specific anesthetic management. During the period of declamping, blood pressure is restored to normal or even shows an increase from the baseline; however, it is a frequently observed phenomenon that, as the cycle of clamping and declamping progresses, declamping causes more significant hypotension. This phenomenon, which can be observed when the cumulative period of clamping lasts 1 hour, may be attributed to a reperfusion-like syndrome as a result of the long-term ischemia of liver parenchyma and splanchnic release of toxic vasodilators; therefore it is recommended to increase the duration of declamping during each cycle, if the cumulative duration is prolonged more than 1 hour, especially in patients with diseased liver (Imamura et al, 2003).
Hemodynamic Consequences and Limitations of Hepatic Vascular Exclusion
The hemodynamic consequences of the addition of total caval clamping to pedicular clamping is more profound (see Table 91A.1). Hepatic vascular exclusion (HVE), which leads to a severe decrease in cardiac preload with 25% decrease in pulmonary artery pressure and 40% to 50% decrease in cardiac index, is associated with a 10% decrease in mean arterial blood pressure despite a 50% increase in heart rate and a very significant increase in systemic vascular resistance. Reduced venous return produces a marked reduction in left ventricular and diastolic volume that could be precisely monitored by transesophageal echocardiography (Eyraud et al, 2002). The sequence of HVE includes initial inflow occlusion followed by infrahepatic caval clamping and then suprahepatic caval clamping. The compensatory cardiac response to maintain blood pressure requires approximately 5 minutes and is facilitated by “preloading” the patient with intravenous fluids. A fall in mean arterial pressure less than 80 mm Hg suggests intolerance to HVE and should lead to consideration of caval declamping. Ventricular dimensions could be monitored by transesophageal echocardiography (Eyraud et al, 2002).
Anesthetic Considerations (See Chapter 22)
Low Central Venous Pressure Anesthesia and Limited Filling
The CVP directly influences the occurrence of back bleeding during liver inflow occlusion. In a retrospective study, Smyrniotis and colleagues (2004) showed that the Pringle maneuver at a CVP of 6 mm Hg or more is associated with greater blood loss than the maneuver performed at a CVP of 5 mm Hg or less. Thus the concept of low CVP anesthesia during hepatectomy has emerged. Maintaining a low CVP during hepatic transection reduces the distension of hepatic veins and thus significantly decreases bleeding (Jones et al, 1998). It also avoids vena caval distension and thus facilitates safe dissection of the retrohepatic vena cava and major hepatic veins. As the blood loss resulting from a vascular injury is proportional to the pressure gradient across the vessel wall and to the fourth power of the radius of the injury, lowering the CVP to one fifth will decrease the blood loss by a factor greater than 5 (Melendez et al, 1998).
Low CVP during liver transection is consistently associated with reduced blood loss (Chen et al, 2000; Cunningham et al, 1994; Eid et al, 2005; Jones et al, 1998; Melendez et al, 1998; Wang et al, 2006). Moreover, in retrospective studies, low CVP tends to be associated with lower postoperative morbidity and reduction of hospital stay (Chen et al, 2000; Smyrniotis et al, 2004).
The potential drawbacks of low CVP anesthesia include perioperative occurrence of air embolism, requirement for pressor agents, and postoperative renal dysfunction. The incidence of gas embolism varies according to the approach and the surgical technique used for parenchymal transection. During a laparoscopic approach, transesophageal echocardiography detects, in nearly all cases, small volumes of air embolism (Schmandra et al, 2002, 2004). During liver resection using ultrasonic devices, air embolism was detected in all the patients who underwent liver resection with an ultrasonic surgical dissector (Koo et al, 2005). Although in the previous study, nearly half of the patients had air embolism filling more than half the right heart diameter, the incidence of clinically relevant accidents is rarely defined. Zhou and colleagues (2008) found an incidence of three cases in 110 liver resections performed with inflow occlusion, and liver surgery complicated by gas embolism accounted for 4% of the patients treated in a referral center for hyperbaric treatment (Bessereau et al, 2010).
Gas embolism usually originates in the venous system from hepatic vein injury through the parenchymal resection stump. Venous gas embolism can lead to arterial paradoxical embolism favored by a patent foramen ovale or intrapulmonary arteriovenous pulmonary shunting (Lee et al, 2002). During hepatic surgery, gas embolism is usually recognized by a sudden drop in end-tidal expiratory carbon dioxide, followed by a subsequent drop in arterial blood pressure or sudden cardiac arrest (Adachi et al, 2006). Arterial systemic embolism can cause arterial ischemia in cerebral, myocardial, spinal, or limb circulation (Lee et al, 2002). Gas embolism is considered a medical emergency, and treatment includes interruption of the embolic procedure, an attempt to extract intravascular gas, external cardiac massage, and immediate oxygenation. Despite an absence of high-level evidence, hyperbaric oxygen therapy is recommended in case of cardiac arrest or in any patient with an unexpected neurologic abnormality following a risky procedure (Blanc et al, 2002; Trytko & Bennett, 2008). But it should be kept in mind that hyperbaric therapy can be limited by the location of hyperbaric chambers, necessitating the transfer of critically ill patients; the ability of those chambers to be used to care for critically ill patients during the therapy; and the risk of hyperoxic seizures and barotrauma (Bessereau et al, 2010; Edsell & Kirk-Bayley, 2009).
The risk of postoperative renal failure linked to low-CVP anesthesia has been suggested in the setting of liver transplantation (Schroeder & Kuo, 2008). During liver resection, the incidence of postoperative renal dysfunction related to low intraoperative volemia has not been clearly established (Melendez et al, 1998). The ability of patients to tolerate fluid restriction in terms of renal function with improved recovery has led some authors to use a restrictive fluid policy in liver surgery. It has been shown in living donor resection that CVP monitoring did not reduce blood loss when a low-infusion policy was routinely applied (Niemann et al, 2007).
Maintaining Low Venous Backflow (See Chapter 22)
The anesthesiologist can maintain a low venous backflow by several methods. Fluid restriction during induction and liver transection is the most commonly used method. Intravenous fluids are given at a rate of 0.5 to 1 mL/kg/h, until the hepatic resection is complete. The patient is brought back to normovolemia at the end of surgery, and hemostasis is ensured. Other methods commonly used are the use of anesthetic gases such as isoflurane, which has systemic vasodilatory properties and results in minimal cardiac depression (Gatecel et al, 2003), and the use of certain drugs that produce vasodilatory effects. Although low tidal volume ventilation was considered to reduce the backflow bleeding, no evidence is available to support that this maneuver reduces the quantity of blood lost during the hepatic transection phase (Hasegawa et al, 2002). The surgeon can decrease the backflow bleeding by partially or totally clamping the infrahepatic IVC. This technique, which decreases venous return, has been shown to have no deleterious effect on renal function, even with a clamping time of up to an hour (Otsubo et al, 2004). The ideal tool for hemodynamic monitoring under these circumstances remains to be determined, although transesophageal echocardiography and pulmonary artery catheterization can be used (Eyraud et al, 2002). Intraoperative monitoring of fluid responsiveness could also be implemented noninvasively, using respiratory variations in arterial pulse pressure or monitoring of peripheral venous pressure (Choi et al, 2007; Solus-Biguenet et al, 2006). In experienced centers, CVP monitoring did not show any significant advantage (Niemann et al, 2007).
Special Considerations During Hepatic Vascular Exclusion
Application of vascular isolation techniques mandates a high level of anesthetic expertise. Intraoperative management of patients undergoing vascular exclusion should include the use of pulmonary artery catheterization and occasionally of transesophageal echocardiography. When a major hepatectomy performed under HVE is planned, anesthetic management is adjusted to anticipate the reduction in venous return, sudden decrease in cardiac output, and increase in afterload. Volume expansion is usually required for patients undergoing HVE. This is achieved by rapid infusion of 500 mL of colloids before cross clamping of the vena cava. In patients who do not tolerate caval cross clamping, even after volume expansion, vasopressor agents such as noradrenaline are added (Redai et al, 2004). Persistent hypotension and/or low cardiac index, which can occur in 10% to 20% of patients, should be considered intolerance to HVE and is an indication to unclamp the vena cava or to consider the use of venovenous bypass (Redai et al, 2004).
Surgical Aspects of Vascular Clamping
Inflow Vascular Clamping
The hepatic pedicle clamping (Pringle maneuver), which interrupts the arterial and portal venous inflow to the liver, is a standard in hepatic surgery. According to the Cochrane database, in elective resection, intermittent portal triad clamping seems better than continuous clamping, especially in patients with diseased parenchyma; therefore intermittent triad clamping could be recommended as the gold standard method of clamping (Gurusamy et al, 2007).
Total Inflow Control
Inflow control implies an encircling of the hepatic pedicle (Fig. 91A.2). Adhesions to the gallbladder are freed, and the lesser omentum is opened at the level of the pars flacida, taking care to avoid injury to the right gastric pedicle. A finger or a blunt dissector may thereafter be easily passed through the foramen of Winslow, and the hepatoduodenal ligament is encircled with tape. Clamping is easily achieved by a vascular clamp or tourniquet, which should be closed until the pulse in the hepatic artery distal to the clamp is stopped; excessive closure should be avoided, as it may otherwise result in arterial or biliary injury. Care should be taken to avoid lymph nodes of the hepatoduodenal ligament, as these may be large in cirrhotic patients or in patients with a long-standing cholestasis. A search for a left hepatic artery originating from the left gastric artery is mandatory to prevent persistent bleeding during parenchymal transection. When a left hepatic artery exists, simultaneous occlusion of this vessel should be performed to complete the vascular inflow control.
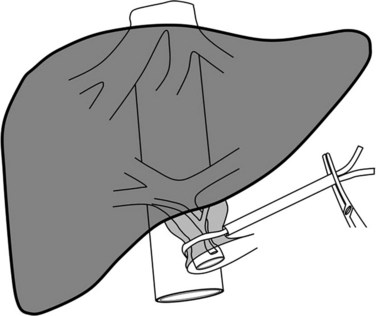
FIGURE 91A.2 Hepatic pedicle clamping (Pringle maneuver) occludes the arterial and portal inflow of the liver.