Vascular Interventional Radiology: Introduction
Interventional uroradiologic procedures can be divided into two major groups: vascular and percutaneous nonvascular. Percutaneous nonvascular interventional procedures are discussed elsewhere. The intravascular route is used, as the therapy of choice, for the embolization of arteriovenous fistulas (AVFs) or malformations, and for bleeding sites. Transcatheter embolization is used for tumor embolization, for the ablation of renal function, for the treatment of testicular vein and ovarian vein varices, and for the treatment of high-flow priapism (Ginat et al, 2009). Balloon angioplasty and stenting of stenotic renal arteries are frequently performed endovascular techniques for the treatment of ischemic nephropathy and secondary hypertension. Renal artery aneurysms may also be treated using catheter-directed techniques such as stent grafting and selective embolization. Occasionally, fibrinolytic agents are delivered via an endovascular catheter to thrombosed renal arteries. Mechanical devices are also available for endovascular treatment of thrombosed renal vessels. This chapter will review these intravascular interventions.
*The authors wish to thank Dr. Anthony Verstandig, Hadassah University Hospital, Jerusalem, Israel, for providing the clinical information and images of the patient depicted in Figures 7–4A and 7–4B.
Transcatheter Embolization
Transcatheter embolization is the treatment of choice for renal AVFs, which may be congenital, spontaneous, or acquired. Iatrogenic AVFs are the type most commonly treated by transcatheter embolization. These occur as a complication of such procedures as percutaneous renal biopsy (Libicher et al, 2006), nephrostomy placement, and pyelolithotomy. Trauma or surgery can also result in AVFs. AVF occurring in the transplant kidney is successfully managed by embolization. The classical angiographic finding of spontaneous or acquired AVF is a feeding artery with an early draining vein. Ancillary findings include pseudoaneurysm and extravasation of contrast material. Congenital AVMs (AV malformations) consist of a group of multiple coiled communicating vessels that may be associated with enlarged feeding arteries and draining veins.
The modes of clinical presentation include hematuria; retroperitoneal or intraperitoneal hemorrhage; and congestive heart failure, cardiomegaly, or both. Hypertension can occur as a consequence of ischemia secondary to venous shunting of blood away from the affected area. A bruit may be heard on physical examination. Duplex Doppler ultrasound is the most useful diagnostic study, performed before angiographic intervention.
Successful intervention requires the angiographic identification, selective catheterization, and embolization of the feeding artery (Figures 7–1A, B). Using a transfemoral approach, an abdominal aortogram is performed to identify the arterial supply to the bleeding kidney. In the case of a renal transplant, an initial pelvic angiogram is performed in a steep oblique projection. The artery supplying the bleeding site is selectively catheterized. A 3 French (3F) coaxial microcatheter is then used for subselective catheterization and embolization of the feeding artery. The use of a microcatheter allows accurate placement of the embolic material. Microcoils are used for the occlusion of iatrogenic AVFs because they can be deployed very precisely, thereby minimizing the loss of renal parenchyma due to resultant ischemia (Figures 7–2A through C). The procedure is usually performed without significant complications. Very rarely, inadvertent nontarget embolization or thrombosis of the renal artery can occur.
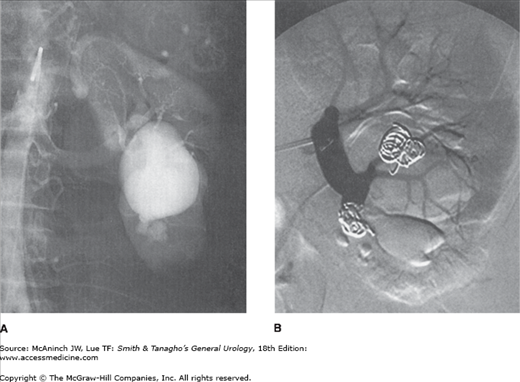
Figure 7–1.
Transcatheter embolization of a large arteriovenous malformation (AVM) in a 64-year-old woman with hematuria. A: A conventional film midstream aortogram. An enlarged left renal artery is seen. There is a large serpiginous AVM arising from the lower pole renal artery branch with aneurysmal dilatation of the draining renal vein. B: Selective left renal digital subtraction arteriogram (DSA) after coil embolization shows cessation of flow in the AVM. Coils have been placed in the terminal portion of the lower pole artery and within the AVM. Embolization resulted in resolution of the hematuria.
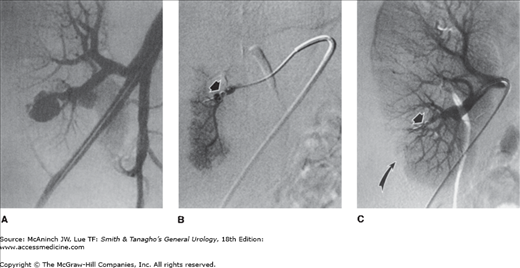
Figure 7–2.
Transcatheter embolization of a postbiopsy arteriovenous fistula (AVF) in a 14-year-old boy with hypertension and prior renal transplantation. A bruit was heard on examination. A: Pelvic arteriogram (DSA) shows an AVF arising from a lower pole branch artery. There is aneurysmal dilatation of the draining vein. B: DSA shows that the renal artery has been selectively catheterized, and a 3F coaxial catheter is positioned peripherally within the lower pole branch artery supplying the AVF. Several microcoils have been placed (arrow) and no flow is seen in the AVF. C: Completion DSA of the main renal artery shows absent flow in the AVF (arrow) with minimal devascularization of lower pole parenchyma (curved arrow).
Transcatheter embolization plays a key role in the management of hemorrhage in the urinary tract originating in the kidney, ureter, bladder, and pelvis (Ginat et al, 2009). Acute life-threatening hemorrhage can occur as a consequence of trauma, instrumentation, and tumors. Chronic intractable hemorrhage is associated with radiation cystitis, tumors, prostatectomy, and infiltrative disorders. Hemodynamically stable patients undergo a noninvasive diagnostic study such as contrast-enhanced computed tomography (CT), before embolization.
Pelvic fractures resulting in life-threatening hemorrhage require embolization for control if resuscitation and external pelvic fixation have been ineffective. Embolization has been shown to be very effective at arresting hemorrhage. Using a transfemoral approach, the practitioner performs a nonselective pelvic arteriogram before selective catheterization and embolization of the hypogastric arteries. Because of contralateral crossover blood supply, pelvic lesions are treated by bilateral embolization. Gelfoam pledgets are frequently used. They can be deployed rapidly, are immediately effective if the patient has a normal coagulation profile, and produce temporary vascular occlusion. Gelfoam sponge is easily cut into pieces appropriate to the caliber of the vessel to be embolized. Coils may be used with, or instead of, Gelfoam. However, if used, they may hamper future access to the hypogastric artery in the event of rebleeding. Small embolic materials such as Gelfoam powder or Ivalon particles are not used to treat hemorrhage from pelvic trauma. They produce very peripheral occlusion of small vessels, thereby risking ischemia of nontarget organs. Complications specific to pelvic embolization are extremely uncommon. Nontarget embolization is rare.
Primary renal cell carcinoma (RCC) is treated by surgical excision. In some cases, preoperative occlusive embolization of the renal artery is used as an adjunct to surgery. Embolization reduces intraoperative hemorrhage and allows immediate ligation of the renal vein. It is used in patients with very large tumors and also in tumors supplied by many parasitized vessels. Embolization accentuates cleavage planes and therefore facilitates nephrectomy. The optimal time delay between embolization and surgery is probably 1 day. Embolization may also favorably impact patient survival (Zielinski et al, 2000). A new application is to use selective embolization of a renal tumor as an adjunctive measure prior to radiofrequency or cryoablation of the tumor (Yamakado et al, 2006).
Palliation of nonresectable disease that causes pain and hematuria can be achieved by transcatheter embolization (Munro et al, 2003). Patients with bilateral RCC, and those with RCC in a single kidney, can undergo subselective embolization as an alternative to surgery, thereby sparing normal parenchyma. Embolization of RCC metastases to bone is performed before surgical resection to decrease intraoperative blood loss (Chatziioannou et al, 2000). CT or magnetic resonance imaging (MRI) may be used for tumor evaluation before and after intervention.
A transfemoral aortogram and selective arteriogram are performed to determine the blood supply to the kidney and tumor. An occlusive balloon catheter may be placed within the vessel and inflated before embolization to prevent reflux of embolic material and inadvertent nontarget embolization. However, many physicians use a simple selective catheter. Gelfoam pledgets are used for preoperative embolization (Figures 7–3A, B). Coils are not used because they can be dislodged during surgery when the kidney is manipulated. Absolute ethanol is the preferred embolic material for ablative palliative embolization of nonresectable tumor. Bone metastases are embolized by positioning a microcatheter in the vessel(s) supplying the tumor and injecting particles of polyvinyl alcohol (PVA) or other embolic agents such as embospheres until maximal obliteration of the angiographic tumor stain is achieved.
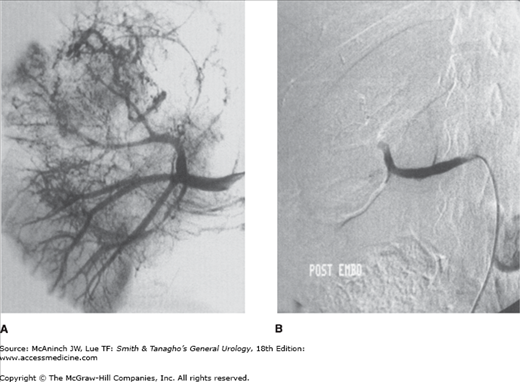
Figure 7–3.
Preoperative embolization of a large right renal cell carcinoma (RCC) in a 28-year-old woman. A: Digital subtraction arteriogram (DSA) of the right renal artery shows a large hypervascular mass involving most of the right kidney. There is tumor thrombus within the renal vein. B: Completion DSA of the right renal artery after Gelfoam embolization shows complete cessation of flow within the tumor and kidney. Contrast is seen within the main renal artery only.
Tumor embolization is a safe procedure. Complications such as puncture-site hematoma and inadvertent nontarget embolization occur in <2% of patients. Almost all patients, however, experience postembolization syndrome (PES). PES consists of severe pain, nausea and vomiting, fever, and leukocytosis. It is probably caused by tissue necrosis that results from successful embolization. Transient ileus, transient hypertension, sepsis, and reversible renal failure have also been described. PES occurs within a few hours of the procedure and may last for several days. Its occurrence should not delay surgical intervention. Tissue swelling and tissue gas formation are seen on imaging studies. The severity of PES is related to the quantity of infarcted tissue. Analgesics and antibiotics are used for treatment. Administration of steroids and antibiotics before embolization may reduce the severity of PES.
Selective embolization has proved to be an effective method of controlling hemorrhage from benign renal lesions while preserving normal parenchyma (Kothary et al, 2005). This technique has been used in the treatment of active bleeding from angiomyolipoma and for the elective prevention of hemorrhage, especially if the tumors are multiple or bilateral, as in patients with tuberous sclerosis. Current guidelines suggest electively embolizing any tumors that are larger than 4 cm in diameter. The procedure is effective in decreasing tumor size and in preventing or treating hemorrhage in 85–90% of patients. CT can clearly identify the fat component of the tumor and is therefore used for diagnosis before intervention and for follow-up (Halpenny et al, 2009).
The technique for embolization is similar to that described for RCC. Through a transfemoral approach, angiography is used to define the arterial supply to the kidney and tumor. The feeding vessels are then selectively catheterized using a coaxial microcatheter. The tumor volume is estimated, and an equal amount of absolute ethanol admixed with iodized oil is carefully injected until the flow ceases. Ethanol is easy to handle, is inexpensive, and produces permanent occlusion of the vascular bed. Iodized oil is radiopaque and therefore is useful for visualizing the flow of the embolic material during the embolization. It remains within the tumor, thereby allowing measurement of tumor response on follow-up CT. An occlusion balloon is reserved for more proximal embolization in a main renal artery when the risk of nontarget embolization is greatest.
The reported complications are similar to those seen after RCC embolization. Recurrence of tumor hemorrhage occurs in approximately 10–15% of patients and is treated by repeat embolization. A short-term tapered dose of prednisone may reduce PES after the procedure (Bissler et al, 2002).
Total renal infarction using transcatheter embolization may be indicated in certain circumstances: namely, abolition of urine production to assist in healing or palliation of terminal patients with urinary fistulas; prevention of excessive proteinuria; management of uncontrollable hypertension; rarely for benign obstructive uropathy in patients who are poor surgical candidates (De Baere et al, 2000; Toussi et al, 2001); and for ablation of failed renal allografts causing the graft intolerance syndrome (Delgado et al, 2005). For patients with end-stage renal disease and intractable hypertension or nephrotic syndrome, the advantages of ablation must be weighed against the loss of production of vitamin D3 and erythropoietic factors and, occasionally, the loss of the ability to eliminate some water. Total renal ablation must be achieved so that perfusion of surviving parenchyma via pericapsular branches cannot occur. The embolic agent must perfuse the entire renal substance but be safe if it passes through the kidney into the venous circulation. The technique is applicable in adults and children and in both native and allograft kidneys. Renal ablation appears to be a safe procedure, which is successful in most patients (De Baere et al, 2000).
Initially, a midstream aortogram is performed to identify the arterial supply to the kidneys. This is followed by renal artery catheterization and selective arteriography. An occlusion balloon catheter is placed in the vessel and contrast medium is injected to measure the volume of embolic agent needed to fill the vascular tree of the kidney. Absolute ethanol is the embolic agent of choice for the reasons mentioned above. An equal volume is carefully injected with the balloon inflated to prevent reflux to nontarget regions. The contents are then aspirated and an angiogram is performed to assess flow. The procedure is repeated as many times as necessary until complete cessation of blood flow is achieved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree