Fig. 29.1
Continent ileostomy. (a) Three limbs of small bowel are measured, and the bowel wall is sutured together. (b) After opening the bowel (see the dotted lines in a), the edges are sewn together to form a two-layered closure. (c) A valve is created by intussuscepting the efferent limb into the pouch and fixing it in place with a linear noncutting stapler (inset: staples in place on valve). (d) The valve is attached to the pouch sidewall with the linear noncutting stapler (a cross section of the finished pouch is shown). (e) After closure of the last suture line, the pouch is attached to the abdominal wall, and a catheter is inserted to keep the pouch decompressed during healing
Intussusception of the terminal 15 cm of ileum into the pouch is performed to construct a valve.
The intussusception is secured with multiple nonabsorbable sutures and staples.
The stoma is sutured flush with the skin and the pouch firmly anchored to the posterior rectus sheath.
A wide plastic tube with large openings is placed into the pouch to allow gravity drainage of the pouch in the early postoperative period.
This tube is occluded for progressively longer periods beginning 10 days after surgery until it can be removed for 8 h without distress.
Postoperative Complications
Nipple valve slippage occurs because of the tendency of the intussuscepted segment to slide and extrude on its mesenteric aspect.
Nipple valve slippage results in difficult pouch catheterization, chronic outflow tract obstruction, and incontinence. It remains the most common complication (30 %).
Pouchitis refers to nonspecific inflammation that develops in the reservoir and is thought to result from stasis and overgrowth of anaerobic bacteria. It occurs in 25 % of patients:
Pouchitis patients present with a combination of increased ileostomy output, fever, weight loss, and stomal bleeding.
The diagnosis is made by history and confirmed by pouch endoscopy.
Pouchitis usually responds to a course of antibiotics and continuous pouch drainage.
Other complications include intestinal obstruction (5 %) and fistulas (10 %).
Fistulas most commonly originate in the pouch itself or at the base of the nipple valve.
90 % of patients eventually have total continence after one or more procedures.
Barnett modification of the Kock pouch (Fig. 29.2) uses the afferent limb of small bowel to construct the nipple valve and wraps a portion of the residual efferent limb around the nipple valve.
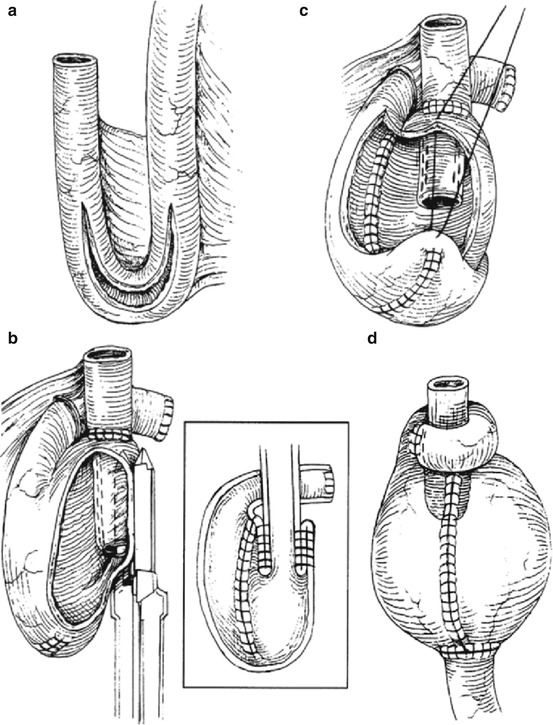
Fig. 29.2
Barnet continent ileostomy reservoir (BCIR). (a) Two limbs of small intestine are sewn together and opened. (b) The afferent limb is intussuscepted to form a valve, and the valve is stapled to the side of the reservoir. (c) The pouch is folded back and sutured closed. Inset shows cross section of pouch. (d) Completed BCIR. The afferent limb of bowel has been divided and reattached to the apex of the pouch, and the efferent limb is wrapped around the valve to form a collar
There are no controlled data to suggest that this modification is any better than the standard procedure.
Ileorectal Anastomosis (IRA)
IRA is mainly considered in patients with indeterminate colitis (IC), in high-risk or older patients who are not good candidates for IPAA, or if there is mild rectal disease where rectal compliance remains adequate.
The operation may also be indicated in the teenager or young adult in order to rapidly regain good health, avoid a stoma, and return to school or work quickly.
In addition, it can also be considered in young females in an attempt to preserve fertility.
Contraindications to IRA include a very diseased and noncompliant rectum, dysplasia or nonmetastatic cancer, perianal disease, and a severely compromised anal sphincter.
Postoperative Complications
Mortality is low, particularly when it is performed as an elective procedure.
Anastomotic leak occurs in less than 10 %, and major sepsis is very uncommon.
Sexual function is well preserved.
Most patients pass between two and four semiliquid stools a day. Nocturnal defecation is common, but true incontinence is rare.
The overall risk of cancer developing in the rectum after IRA approximates 6 %.
Most cancers appear 15–20 years after operation.
Patients being offered IRA must realize the need for semiannual sigmoidoscopy with multiple biopsies to detect dysplasia, polyps, or invasive cancer.
The rectal stump may be the site of recurrent or persistent inflammation in 20–45 % of patients.
Clinical features include severe diarrhea, tenesmus, bleeding, and urgency.
Rectal excision is needed in those cases that do not respond to topical or systemic therapies.
About one-quarter of patients require proctectomy after IRA for severe proctitis.
Ileal Pouch–Anal Anastomosis
The anorectal sphincter mechanism must be intact to prevent leakage of watery ileal contents.
Laparoscopic ileal pouch surgery is associated with longer operating time and less blood loss but may have short-term benefits such as diminished postoperative pain, reduced narcotic requirements, and shorter hospital stay compared to open surgery (Figs. 29.3, 29.4 and 29.5).
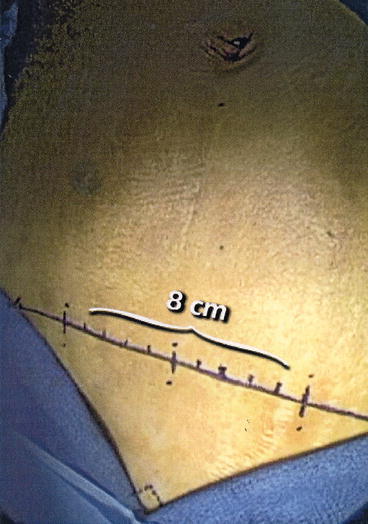
Fig. 29.3
Hand-assisted colectomy begins with 8 cm Pfannenstiel or lower midline incision. Note how positioning of towels from the root of penis or top of the introitus to the anterior superior iliac spine creates a right angled triangle, assuring a straight transverse incision
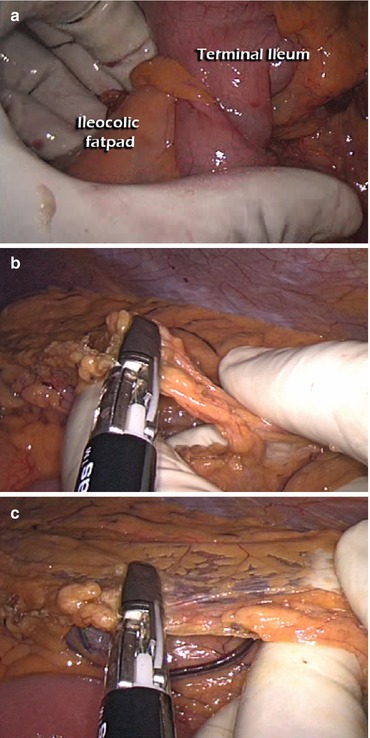
Fig. 29.4
Technical maneuvers during hand-assisted laparoscopic total colectomy. (a) Traction of the ileocolic fat pad with traction towards the right lower quadrant will facilitate identification and preservation of the ileocolic artery. The omentum and transverse colon mesentery are divided either together (b) or separately after entry into the lesser sac (c)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






