Ulcerative colitis
Carlos Sierra Salinas MD
Javier Blasco Alonso MD
Introduction
Ulcerative colitis (UC) is a relapsing and remitting disease characterized by acute non-infectious inflammation of the colorectal mucosa. Crohn’s disease (CrD) and UC are the two main types of inflammatory bowel disease (IBD). While children and adults develop similar symptoms, children often present with more extensive disease.
Epidemiology
UC may appear at any age. Most of the children are between 10 and 18 years. The incidence of UC in children and adolescents per 100,000 children per year varies between 0.5 (France) and 4.3 (Norway). The incidence of UC in children has remained relatively stable. Multiple genes may contribute to the pathogenesis of UC; essential is the interaction with the environment. Among others factors, several authors have suggested the correlation with exposure to infections in the perinatal period or early life, the inverse relationship with breast-feeding, the administration of nonsteroidal anti-inflammatory drugs, and the inverse relationship with appendectomy before the age of 20 years.
Evidence of higher rates of UC in urban areas raises the issue of a transmissible agent that may be responsible for the disease expression or increased susceptibility. However, no specific infectious agent has been associated with the development of the disease.
Pathogenesis
The pathogenesis remains unknown. Recent literature reports an intensive search for the antigens that trigger the immune response in inflammatory bowel disease. One hypothesis is that these triggers are microbial pathogens, as yet unidentified with an appropriate but ineffective immune response to these pathogens. Another hypothesis affirms that there are some common dietary antigens or nonpathogenic microbial agents to which the patient mounts an abnormal immune response. The autoimmune theory postulates that an antigen is expressed on the patient’s own intestinal epithelial cells and there is an immune response to antigen and own epithelium which are thus destroyed by immune mechanisms.
Clinical features
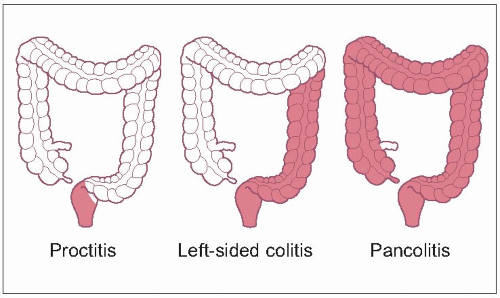
The presentation may vary depending upon the extent of colonic involvement and the severity of inflammation. According to the extent of the disease, three subgroups have been established (11.1):
Proctitis (25%): disease limited to the rectum.
Left-sided colitis (30%): involving the descending colon up to the splenic flexure.
Pancolitis (45%): involvement proximal to the splenic flexure, usually up to the caecum.
The predominant symptom is diarrhoea, which can be associated with frank blood in the stool. The patient has frequent bowel movements, which may be small in volume, as a result of irritability of the inflamed rectum. Other symptoms include abdominal or rectal pain related to defecation, fever, and weight loss (Table 11.1).
Proctitis may present with tenesmus, urgency, and the passage of semi-formed stool with blood and mucus. In contrast, left-sided colitis or pancolitis may present with bloody diarrhoea and significant abdominal pain. The majority of patients will present with a history of symptoms for several weeks. For this reason growth failure is much less frequent than in children with CrD. The extent of colonic mucosal involvement and severity of disease correlate with the clinical manifestations of UC (Table 11.2)
Differential diagnosis
The most difficult decision may be to establish whether the diagnosis is UC or CrD (Table 11.3). The infectious aetiologies should be investigated with stool cultures and stool test for Clostridium difficile toxins A and B. Identification of a pathogen, however, does not necessarily exclude a diagnosis of UC, as a first episode of UC may present after documented enteric infection (Table 11.4). In infancy it is important to exclude other causes of bloody diarrhoea such as allergic colitis and Hirschsprung’s colitis.
Physical examination is notably less informative than in CrD, except for the demonstrations of extraintestinal manifestations that may be associated with UC.
Table 11.1 Symptoms of ulcerative colitis | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree