Treatment of Liver Cysts
T. Peter Kingham
Ronald P. DeMatteo
Introduction
Hepatic cysts can be divided into neoplastic and non-neoplastic categories. Non-neoplastic cysts are may be further subdivided into parasitic and non-parasitic cysts, with the latter group comprised of simple hepatic cysts and polycystic liver disease. Benign or simple hepatic cysts are likely a result of congenital malformation of intrahepatic biliary ducts that gradually enlarge over time. Approximately 4% to 7% of the general population has simple hepatic cysts, the majority of which cause no symptoms and rarely affect liver function. Polycystic liver disease is an inherited disorder, commonly associated with polycystic kidney disease, and often causes symptoms that require intervention. Hydatid disease, the most clinically relevant parasitic cystic lesion, is uncommon outside of endemic areas of the world and is the result of infestation with Ecchinococcus granulosus or, less commonly, Ecchinococcus multilocularis. Biliary cystadenoma or cystadenocarcinoma are the most common neoplastic cystic diseases of the liver but are extremely uncommon. Cystadenomas are benign but premalignant tumors that must be resected completely; it is critical, therefore, to distinguish them from simple cysts. In addition, it is important to recognize that some malignant liver lesions may have a large cystic component but are not typically considered as hepatic cysts (Fig. 28.1).
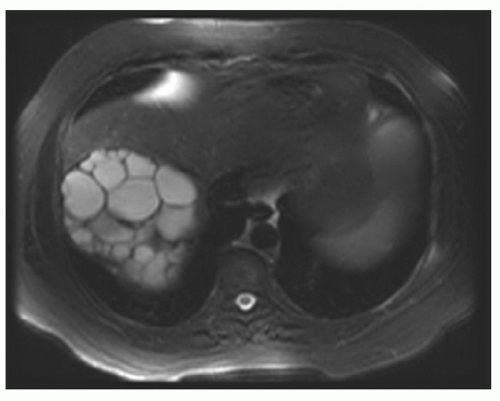
Treatment of cystic liver lesions varies and is critically dependent on the diagnosis and the presence or absence of symptoms. Imaging plays a central role in diagnosis and establishing the most appropriate therapy. Simple cysts, the most common diagnosis encountered in clinical practice, are generally sharply demarcated from the surrounding liver parenchyma. Simple cysts are comprised of thin, clear fluid, usually clear in color and appear as homogeneous hypodense lesions on CT (Fig. 28.2A). Other imaging modalities, however, particularly US and MRI, provide more useful for evaluating cystic lesion. On US, simple cysts are characteristically thin walled, with a uniform appearance of the intracystic contents and posterior acoustic shadowing (Fig. 28.2B). On MRI, simple cysts are uniformly hyperintense on T2-weighted images (Fig. 28.2C) and show no evidence of perfusion on the post-gadolinium sequences (Fig. 28.2D). The classic imaging appearance of simple cysts may be altered, however, by changes in the cyst contents. Intracystic hemorrhage, in particular, can result in accumulation of proteinaceous debris that results in a complex appearance on imaging (i.e., heterogeneous, thick walled, internal septae Fig. 28.3A, B), that is difficult to distinguish from biliary cystadenoma (Fig. 28.4). Polycystic liver disease and hydatid disease are both associated with multiple cysts. Hydatid disease is characterized by multiple, clustered, thick-walled daughter cysts (Fig. 28.5); the
diagnosis is confirmed with a history of exposure in an endemic area and elevated ecchinococcal titers. Polycystic liver disease, on the other hand, appears as diffuse involvement of the liver with innumerable simple cysts (Fig. 28.6).
diagnosis is confirmed with a history of exposure in an endemic area and elevated ecchinococcal titers. Polycystic liver disease, on the other hand, appears as diffuse involvement of the liver with innumerable simple cysts (Fig. 28.6).
 Figure 28.1 Primary leiomyosarcoma of the liver with a large cystic component. Note the irregular cyst wall. |
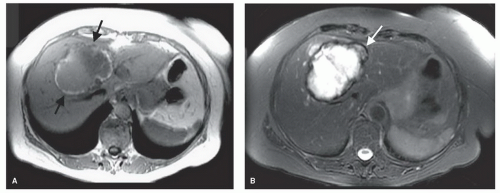 Figure 28.3 MRI of cyst demonstrates intracystic hemorrhage with thick-walled rim (arrows, A). MRI of cyst with hemorrhage and a heterogeneous appearance of the cyst (arrow, B). |
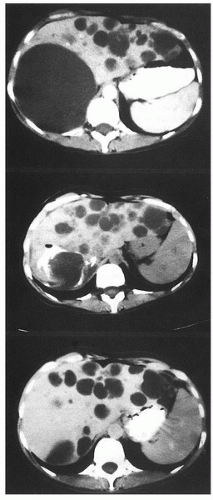 Figure 28.6 Demonstration of polycystic liver disease (from Blumgart, Surgery of the Liver, Biliary Tract and Pancreas, 4th Edition, Saunders, 2007, with permission). |
Treatment of cystic lesions include:
Aspiration
Sclerosis
Enucleation
Fenestration
Resection
When indicated, primarily for symptoms, unroofing or fenestration of simple cysts is the procedure of choice. Unroofing or fenestration of hepatic cysts was first described
in 1968. More recently, minimally invasive techniques have been utilized for laparoscopic unroofing. Before one proceeds with cyst fenestration as the definitive procedure, one must exclude other entities. Cystadenoma or cystadenocarcinoma are the most common confounding diagnoses and must be resected rather than opened; hydatid disease rarely causes diagnostic confusion, as discussed above. One option in such cases is laparoscopic or open excisional biopsy of the cyst wall with frozen section histology, which can usually distinguish simple from neoplastic cysts. Percutaneous drainage and sclerosis of simple cysts has been described, but reaccumulation of cyst fluid is common, and this procedure is currently reserved for patients with an infected cyst or patients who cannot tolerate general anesthesia. Extreme care must be taken to prove that there are no cyst-biliary tree connections before introducing a sclerosant.
in 1968. More recently, minimally invasive techniques have been utilized for laparoscopic unroofing. Before one proceeds with cyst fenestration as the definitive procedure, one must exclude other entities. Cystadenoma or cystadenocarcinoma are the most common confounding diagnoses and must be resected rather than opened; hydatid disease rarely causes diagnostic confusion, as discussed above. One option in such cases is laparoscopic or open excisional biopsy of the cyst wall with frozen section histology, which can usually distinguish simple from neoplastic cysts. Percutaneous drainage and sclerosis of simple cysts has been described, but reaccumulation of cyst fluid is common, and this procedure is currently reserved for patients with an infected cyst or patients who cannot tolerate general anesthesia. Extreme care must be taken to prove that there are no cyst-biliary tree connections before introducing a sclerosant.
 INDICATIONS/CONTRAINDICATIONS
INDICATIONS/CONTRAINDICATIONSNon-parasitic cysts:
Indications for treatment include:
Infection
Jaundice
Cyst rupture and hemorrhage
Early satiety
Pain
Contraindications include:
Asymptomatic cysts
High concern for neoplastic diagnosis
 PREOPERATIVE PLANING
PREOPERATIVE PLANINGThere are several important preoperative investigations that assist in diagnosing and surgical planning, both generally and specifically related to cystic lesions (see also Chapter 18):
History: Polycystic kidney disease, abdominal pain, early satiety
Clinical examination: Jaundice, abdominal tenderness, stigmata of portal hypertension
Laboratory evaluations: Bilirubin, alkaline phosphatase, AST, ALT, serology if concern for hydatid disease, tumor markers (CEA, CA 19-9)
Radiologic work-up:
US: Evaluates the patency of main hepatic pedicles and veins, the location of the cyst, the degree of biliary dilatation. Ultrasound is perhaps the most useful modality for assessing the cyst wall and cyst contents (Fig. 28.7).
CT scan: Useful to determine the location of the cyst within the liver, the volume of the normal liver, whether a laparoscopic or open approach is appropriate (Fig. 28.8A, B).
MRI: Provides additional information if there is a question on the CT scan as to the etiology of the cyst (Fig. 28.9).
 SURGICAL TECHNIQUE
SURGICAL TECHNIQUEUnroofing of a Simple Cyst
Open or laparoscopic approaches can be utilized for unroofing of a simple cyst. Laparoscopic approaches are ideal for the majority of simple hepatic cysts. Open approaches may be required for cysts deep within the liver or in the posterior sector.
 Figure 28.7 Preoperative ultrasound of a right lobe hepatic cyst (arrow points to cyst). Note the single simple septum and smooth border of the cyst. |
 Figure 28.8 Preoperative CT scan in axial (A) and coronal (B) sections of a right lobe hepatic cyst with hemorrhagic debris (arrow points to debris). |
 Figure 28.9 Preoperative MRI of a right lobe hepatic cyst hyperintense on T1 imaging with a single simple septum. |
 Figure 28.10 Port placement site for deroofing of the right hepatic lobe cyst demonstrated in Figures 28.7
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|