CHAPTER 66 Treatment of Gallstone Disease
MEDICAL TREATMENT
Medical treatment of gallstone disease was first proposed by Schiff in Italy in 1873.1 Dabney of Virginia first reported the effective treatment of gallstones with bile acids in 1876, an observation later confirmed by Rewbridge of Minnesota in 1937.2,3 Despite these initial reports, the use of medical dissolution treatment did not gain acceptance until large clinical series were reported in the 1970s. Contact dissolution of gallstones with solvents and percutaneous cholecystolithotomy techniques also have been reported, but these modalities have not proved superior to oral dissolution, shock-wave lithotripsy, or laparoscopic cholecystectomy and have been abandoned. The mainstay of current nonsurgical treatment of gallstone disease is oral dissolution with ursodeoxycholic acid, with or without extracorporeal shock-wave lithotripsy.
Although nonsurgical treatment of gallstones has proved effective in carefully selected patients, only a limited number of patients are candidates for this treatment option. Nonsurgical treatments are effective only in patients with small, cholesterol gallstones. Significant admixtures of pigment or calcium salts make stones indissoluble. In addition, long-term success with medical treatment of gallstones occurs only in patients in whom the lithogenic disturbance that led to gallstone formation is transient. For most patients, gallstone formation represents an imbalance in biliary lipid excretion, gallbladder stasis, or infection of the bile (see Chapter 65). In these patients, successful dissolution is usually followed by recurrence of gallstones in 30% to 50% of patients within five years.4–7 Therefore, the proper choice of treatment must take into account the type and severity of symptoms, the physical characteristics of the stones, gallbladder function, and the characteristics and preference of the patient.
DISSOLUTION THERAPY
The rationale for oral dissolution therapy is the reversal of the condition that led to formation of cholesterol gallstones, namely, the supersaturation of bile with cholesterol (see Chapter 65). Cholesterol stones dissolve if the surrounding medium is capable of solubilizing the cholesterol in the stones. Both chenodeoxycholic acid and ursodeoxycholic acid dissolve gallstones by decreasing biliary cholesterol secretion and desaturating bile. These agents encourage the removal of cholesterol from stones via micellar solubilization, formation of a liquid crystalline phase, or both. Chenodeoxycholic acid was the first bile acid used for gallstone dissolution but has been abandoned because of side effects, including diarrhea and increased serum aminotransferase and cholesterol levels. Ursodeoxycholic acid is well tolerated and is currently used in oral dissolution regimens. In randomized comparisons, ursodeoxycholic acid was just as effective as chenodeoxycholic acid alone or in combination with ursodeoxycholic acid.8–10
The rate of stone dissolution is a function of (1) thermodynamic forces, including the degree of bile desaturation and the concentration of ursodeoxycholic acid in bile; (2) kinetic forces, including stirring of bile; and (3) the surface-to-volume ratio of the stones. Oral dissolution targets the thermodynamic forces.11 Because small stones have a smaller surface-to-volume ratio, they respond more quickly and reliably to oral dissolution therapy.
The use of oral dissolution therapy does not address the problem of gallbladder stasis.12 Although prokinetic agents, including alpha-adrenergic antagonists and clarithromycin, have been shown to increase gallbladder motility, their use in preventing and treating gallstones has not been studied.13,14
Patient Selection
Selection of patients for oral dissolution therapy is a function of the stage of gallstone disease, gallbladder function, and the characteristics of the stones. Selection criteria are summarized in Table 66-1. Oral dissolution therapy should be considered for patients with uncomplicated gallstone disease, including those with mild, infrequent biliary pain. Patients with severe or frequent biliary pain and patients with complications of gallstones, including cholecystitis, pancreatitis, and cholangitis, should not be treated with oral dissolution therapy; these patients should be referred for surgery. In addition, the gallbladder must function and the cystic duct must be patent to allow unsaturated bile and stones to clear from the gallbladder. The patency of the cystic duct is usually evaluated by oral cholecystography. More recently, stimulated cholescintigraphy and functional ultrasonography have been used. These latter modalities assess cystic duct patency as well as gallbladder function.
Table 66-1 Selection Criteria for Oral Bile Acid Dissolution Therapy
| Stage of gallstone disease | Symptomatic (biliary pain) without complications |
| Gallbladder function* | |
| Stone characteristics |
* Either stimulated cholescintigraphy or functional ultrasonography may be done.
The characteristics of the stones play an important role in determining the efficacy of dissolution treatment. Oral dissolution therapy works only on cholesterol stones. Although verifying the composition of gallstones can be difficult, the appearance of stones on plain films or computed tomography (CT) images can be useful. Cholesterol stones are radiolucent on conventional radiographs, and they are hypodense or isodense to bile and lack stone calcification on CT images.15 During oral cholecystography, the specific gravity of cholesterol stones is less than or equal to that of contrast-enriched bile, thereby resulting in stone buoyancy.16 The number of stones does not influence the success of oral dissolution therapy; however, only patients with stones that occupy less than one half of the gallbladder volume should be considered for treatment. Although oral dissolution therapy has been effective in stones up to 10 mm in diameter, results are best in stones less than 5 mm in size.17,18 The ideal stones for oral dissolution treatment are shown in Figure 66-1.
Therapeutic Regimens
Ursodeoxycholic acid (ursodiol) is the preferred drug for oral dissolution treatment. It is taken in a dose of 10 to 15 mg/kg of body weight per day. Nighttime dosing is more effective and is associated with better patient compliance than mealtime dosing.19 Unlike chenodeoxycholic acid (chenodiol), ursodeoxycholic acid is well tolerated and has no important side effects. Treatment should continue until stone dissolution is documented by two consecutive negative ultrasonograms at least one month apart. Treatment should be stopped if the patient does not tolerate the drug or experiences a complication of gallstones during therapy or if the stones fail to dissolve after six months or dissolve only partially after six months with lack of progression to complete dissolution by two years.
Efficacy
With ursodeoxycholic acid, complete dissolution is achieved in 20% to 70% of patients. The variability in the reported response rates is a function of differences in patient selection, doses of bile acid, treatment times, and diagnostic techniques used to document stone dissolution.9,10,20,21 A meta-analysis of all randomized trials of dissolution treatment showed stone dissolution in 37% of patients.9 The frequency of stone dissolution was 29% for stones larger than 10 mm, 49% for stones smaller than 10 mm, and 70% for stones less than 5 mm. The time to resolution varies among patients, with a median rate of 0.7 mm per month.11 Improvement in symptoms occurs before stones have dissolved completely. In addition, long-term treatment has been reported to decrease the risk of biliary pain and acute cholecystitis, independent of gallstone dissolution.18 Despite initial dissolution of stones in properly selected patients, the rate of gallstone recurrence after oral dissolution therapy is 50% after five years, with most recurrences within the first two years.5,7 The risk is lower in patients with a solitary stone than in those with multiple stones.
EXTRACORPOREAL SHOCK-WAVE LITHOTRIPSY
The application of extracorporeal shock-wave lithotripsy to the treatment of gallstones was first applied to patients by Sauerbruch in 1985.22 The rationale for shock-wave lithotripsy is to diminish the surface-to-volume ratio of a stone, thereby increasing the efficacy of oral dissolution and decreasing stone size to allow small stones and debris to pass directly from the gallbladder into the intestine without causing symptoms. The technique involves the delivery of focused high-pressure sound waves to gallstones. Three types of lithotripters have been developed: underwater spark-gap, piezoelectric crystals, and electromagnetic membrane lithotriptors.23 Regardless of the energy source, the shock waves from the lithotriptor are delivered from an underwater source to the soft tissue. Passage of the shock wave through the soft tissue does not diminish the energy wave significantly. Passage of the shock wave through the anterior and posterior walls of the stone liberates compressive and tensile forces and causes cavitation at the anterior surface of the stone, thereby leading to stone fragmentation. Factors that influence fragmentation include the size, microcrystalline structure, and architecture of the stone. Although the composition of the stone does not influence successful lithotripsy, only cholesterol stone fragments are dissolved effectively by bile acid therapy.
Patient Selection
Because shock-wave lithotripsy is usually combined with oral dissolution therapy, patient selection criteria for shock-wave lithotripsy are similar to those for oral dissolution treatment and are summarized in Table 66-2. Gallbladder function and cystic duct patency are required and are demonstrated by oral cholecystography, functional ultrasonography, or stimulated cholescintigraphy (see Chapter 65). Lithotripsy should be considered only for patients with mild, uncomplicated biliary pain. Pregnant patients and patients on anticoagulants should not undergo lithotripsy. Shock-wave lithotripsy is reserved for patients with a solitary stone, measuring less than 2 cm in size.6,24 Because only cholesterol stones are reliably cleared by the addition of oral dissolution therapy, stones should have radiographic features, such as radiolucency, suggestive of cholesterol stones.
Table 66-2 Selection Criteria for Extracorporeal Shock-Wave Lithotripsy
| Stage of gallstone disease | Symptomatic (biliary pain) without complications |
| Gallbladder function* | |
| Stone characteristics |
* Either stimulated cholescintigraphy or functional ultrasonography may be done.
Therapeutic Approach
Patients usually are given sedatives and analgesics or are anesthetized and placed in the prone position to minimize the distance between the energy source and the stones and to eliminate interference from intestinal gas and the costal margin. Targeting and monitoring for fragmentation are accomplished with ultrasonography. Multiple treatment sessions are often required to achieve sufficient pulverization. Factors that predict the success of lithotripsy include the degree of fragmentation and gallbladder emptying.25–27 Fragmentation depends on stone characteristics and the dose of the shock wave. Important stone characteristics include the size and number of stones as well as their structure and the presence of calcification.25,28,29 The energy of shock waves, number of shock waves per session, and number of sessions also influence the success rate.30,31 Ursodeoxycholic acid, 10 to 15 mg/kg of body weight per day, is administered orally to dissolve stone fragments, especially when residual stone fragments are larger than 2 mm in size, gallbladder function is poor, or the gallbladder has not cleared small fragments within three to six months of lithotripsy.32 An example of successful combined treatment is shown in Figure 66-2.
Efficacy
The percentage of patients who are free of stones after 6 and 12 months is 47% to 77% and 68% to 84%, respectively.24,25,33–37 Follow-up data reveal 27%, 41%, and 54% cumulative recurrence rates at 3, 5, and 10 years, respectively.38 Recurrence is most often related to the presence of lithogenic bile and gallbladder dysmotility, rather than patient variables such as gender, age, and weight. Factors that predict higher rates of treatment failure include stones larger than 16 mm in size, multiple stones, and stones with a CT density of greater than 84 Hounsfield units.39 Recurrent stones are usually small and multiple and cause recurrent biliary pain. Maintenance therapy with ursodeoxycholic acid after lithotripsy is not cost effective and has not been shown to be effective.7,40
Side effects of lithotripsy include petechiae of the skin at the site of shock-wave delivery (8%), hematuria (4%), and liver hematomas (<1%). No long-term liver biochemical abnormalities have been noted. Biliary pain develops in approximately one third of patients; cystic duct obstruction develops in 5%; and complications of stone passage, such as biliary pancreatitis, develop in less than 2%.25
Lithotripsy is more cost-effective in the elderly than in the young and less cost-effective in patients with multiple stones than in those with a single stone. When combined with ursodeoxycholic acid, lithotripsy is at least as cost-effective as open cholecystectomy for patients with small stones and less cost-effective for those with large stones.41,42 When lithotripsy is compared with laparoscopic cholecystectomy, patients who undergo laparoscopic cholecystectomy experience a greater incremental improvement in quality of life at six months, whereas those who undergo lithotripsy have higher rates of recurrent stones and biliary symptoms.43
Bile Duct Stones
Extracorporeal shock-wave lithotripsy has also been used in the management of choledocholithiasis. Intracorporeal electrohydraulic lithotripsy has been shown to be effective in this setting as well. These treatment options are reserved for patients who fail conventional endoscopic measures (see Chapter 70), mechanical lithotripsy, or surgical treatment of choledocholithiasis. Appropriate indications for shock-wave lithotripsy are large stones impacted in the bile duct that are not amenable to endoscopic extraction, intrahepatic stones, stones above a biliary stricture, cystic duct remnant stones, and bile duct stones associated with Mirizzi’s syndrome (compression of the common hepatic duct) (see Chapter 65). Selection of patients for shock-wave treatment of bile duct stones is similar to that for treatment of uncomplicated gallbladder gallstones.
The success rate for treatment of bile duct stones is 70% to 90%.44–49 Most patients require endoscopic extraction of large stone fragments following treatment. Mild, transient hemobilia occurs in 10% of patients, and biliary sepsis develops in 4% following the procedure. Other complications are similar to those seen after lithotripsy for gallbladder stones. Because of the potential for septic complications, preprocedure endoscopic, nasobiliary, or percutaneous biliary drainage is performed. Antibiotics are given to minimize the risk of biliary sepsis.
SURGICAL TREATMENT
Approximately 700,000 cholecystectomies are performed for gallstone disease in the United States each year. Currently, the vast majority of these operations are performed using laparoscopic techniques. For example, 7888 cholecystectomies were performed in Utah in 2005; 96% of these operations were laparoscopic cholecystectomies, and 4% were open procedures. A review of the National Hospital Discharge Database from 1998 to 2001 showed that 25% of cholecystectomies were performed by an open approach. Of the remaining 75% done laparoscopically, the rate of conversion to open cholecystectomy was 5% to 10%.50 Patients with complicated gallstone disease, including acute cholecystitis, gallstone pancreatitis, and choledocholithiasis, are more likely than those with uncomplicated disease to require an open cholecystectomy or conversion from a laparoscopic to an open approach.50 Despite the increased reliance on minimally invasive techniques in the care of these patients, open cholecystectomy continues to play an important role in the management of complications of gallstones.
OPEN CHOLECYSTECTOMY
Karl Langenbuch, a surgeon in Berlin, is credited with performing the first cholecystectomy in 1882. Since then, cholecystectomy has remained the main therapeutic option for the management of patients with gallstones, largely because of its remarkable success in relieving symptoms and its low morbidity. In prospective studies, 90% to 95% of patients who undergo cholecystectomy experience substantial or complete relief of their symptoms.51,52 Cholecystectomy is more effective in relieving biliary pain than in relieving dyspepsia and flatulence, which are less strongly correlated with gallstone disease.
Results
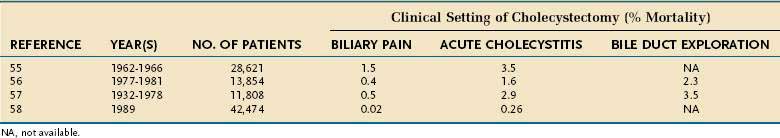
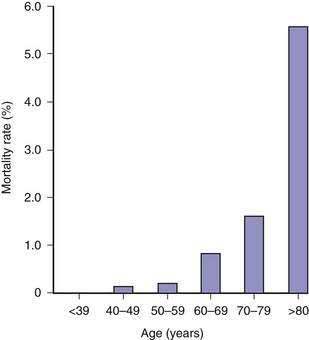
The risk of open cholecystectomy has declined over the years. The overall mortality rate of cholecystectomy in 35,373 patients operated on before 1932 was 6.6%.53 This rate decreased to 1.8% by 1952.54 Since then, the overall mortality rate for cholecystectomy has averaged about 1.5%. The mortality rate is considerably lower in patients operated on electively for biliary pain, with an average of less than 0.5% (Table 66-3).55–57 The risk of death is several-fold higher when cholecystectomy is performed as an emergency for acute cholecystitis and when bile duct exploration is required (see Table 66-3). Additionally, the mortality rate is directly proportional to the patient’s age (Fig. 66-3). In a report of the entire Danish experience with cholecystectomy from 1977 to 1981, patients under the age of 50 years had a risk of death of 0.028% from elective cholecystectomy56; the rate rose to 5.56% in patients older than 80 years of age. The experience in the United States has been similar. Of 11,808 patients who underwent cholecystectomy at the New York Hospital–Cornell Medical Center between 1932 and 1978, the risk of death from elective cholecystectomy for chronic cholecystitis was 0.1% in patients less than age 50 years and 0.8% in those 50 years of age or older.57 In a later series, the overall mortality rate of 42,474 patients who underwent cholecystectomy in 1989 in California and Maryland was 0.17%.58 In this series, the mortality rate in patients less than 65 years of age was 0.03%, compared with more than 0.5% in patients 65 years of age and older. Likewise, the morbidity rate, mean length of hospital stay, and average hospital charges were significantly higher in the older patients than in the younger group. Most mortality following cholecystectomy is related to cardiac disease, particularly myocardial infarction.
Major complications after open cholecystectomy are rare. In a large survey of 28,621 patients who underwent cholecystectomy in the 1960s, complications occurred in 4.0%.55 Subsequent studies have confirmed a 4.0% to 5.0% rate of perioperative morbidity.59–61 Most complications are relatively minor, such as wound infections or seromas, urinary retention or infection, and atelectasis. Complications related specifically to cholecystectomy include bile leaks, bile duct injury, and acute pancreatitis. Of these complications, bile duct injury is the most serious and often requires endoscopic therapy and, in some cases, complicated and technically difficult surgical repair (see Chapter 70). Alternatively, bile duct injury can lead to benign biliary stricture formation and bile duct obstruction with secondary biliary cirrhosis and liver failure. The rate of bile duct injury during open cholecystectomy is not known precisely but has been estimated to be 1 in 200 to 600 cases.62,63 Two ductal injuries occurred in 1200 cholecystectomies at the Cedars-Sinai Medical Center in Los Angeles from 1982 to 1988,64 and no bile duct injuries occurred in 1252 patients who underwent elective cholecystectomy at two large North American and European centers.65 In general, bile duct injuries are preventable complications and are commonly the result of inadequate surgical training, unrecognized variations in bile duct anatomy, or misidentification of normal anatomy. Unusual amounts of bleeding, severe inflammation, and emergency operations do not play as great a role in these injuries as might be supposed.
LAPAROSCOPIC CHOLECYSTECTOMY
Technique
The operative team for laparoscopic cholecystectomy generally consists of a surgeon, assistant surgeon, scrub nurse, circulating nurse, and anesthesiologist. Patients are asked to void immediately prior to entering the operating room. Prophylactic antibiotics are not routinely administered to patients with uncomplicated gallstone disease, including biliary pain.66 Patients with potential infectious complications of gallstones, including acute cholecystitis and cholangitis, and patients with long-standing symptoms or advanced age should receive antibiotics if these agents were not already started before surgery.67 Sequential compression stockings are used to reduce the risk of lower extremity thromboembolism.
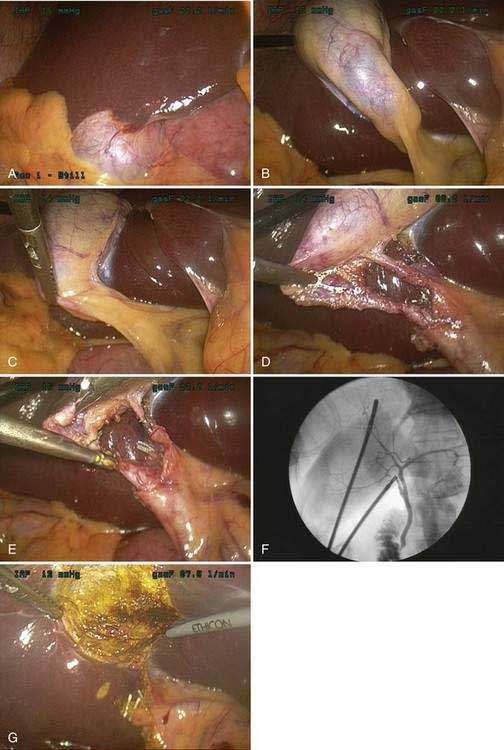
The current technique of laparoscopic cholecystectomy is best described as “the critical view” approach,68 as summarized in Figure 66-4. In this approach, the entire hepatocystic triangle is dissected, exposing the cystic duct and artery, infundibulum of the gallbladder, and junction of the gallbladder and cystic duct before a cholangiogram is performed or the cystic duct and artery are divided. The assistant retracts the gallbladder fundus cephalad, anterior to the liver, and the infundibulum laterally. The surgeon, operating through the epigastric port, identifies and dissects the cystic duct and artery circumferentially. Special care must be taken to identify the junction of the cystic duct and gallbladder, to ensure that the bile duct has not been isolated inadvertently. Cholangiography is performed via cannulation of the cystic duct. If the cholangiogram shows normal anatomy and no evidence of choledocholithiasis, the cholangiocatheter is removed and the cystic duct and artery are divided between small metal clips. The gallbladder is then dissected out of the liver bed and delivered through the umbilical incision. Care is taken to avoid perforation of the gallbladder during its dissection from the liver because the spillage of gallstones and bile has been shown to increase the risk of postoperative fever and intra-abdominal abscess formation.69 The operation concludes with evacuation of the pneumoperitoneum and closure of the incisions.
Rationale for Cholangiography
Cholangiography during laparoscopic cholecystectomy has two main purposes. First, the cholangiogram may detect unsuspected bile duct stones. Second, the cholangiogram confirms the surgeon’s impression of the anatomy of the bile ducts. In the era before laparoscopic cholecystectomy, the value of routine cholangiography during cholecystectomy was debated, with some surgeons arguing in favor of its selective use.70 Routine cholangiography has been criticized because of its relatively low yield, failure to identify all retained stones, occasional false-positive results, cost, and risk. Nevertheless, 8% to 16% of all patients with cholelithiasis harbor bile duct stones. Routine use of operative cholangiography detects unsuspected bile duct stones in about 5% of patients who undergo cholecystectomy and detects anatomic ductal abnormalities in 12%.71 During laparoscopic cholecystectomy, the two-dimensional video image and inability to palpate structures of the porta hepatitis make identification of the cystic duct–bile duct junction problematic. Cholangiography plays an especially important role in delineating bile duct anatomy prior to division of any important structures. Large population studies from Australia and Sweden have demonstrated the importance of routine intraoperative cholangiography in decreasing the frequency of major bile duct injuries.72,73 The rate of bile duct injury during laparoscopic cholecystectomy when routine cholangiography is performed is 0.2% to 0.4%, compared with 0.4% to 0.6% when cholangiography is not performed routinely.72–74 Routine cholangiography is cost effective when the cost associated with bile duct injuries is considered.75 In addition, routine cholangiography permits earlier identification of intraoperative bile duct injuries, if they occur,76 and thereby improves the rate of repair.
Results
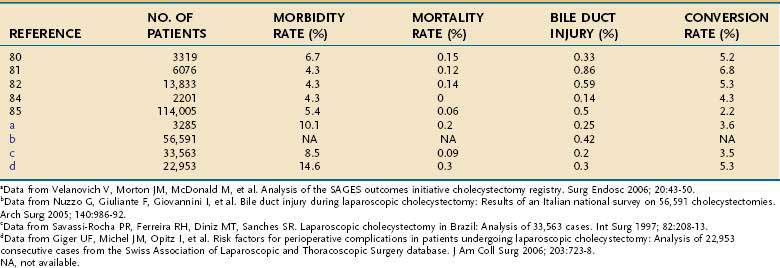
Several large series have now described the experience with laparoscopic cholecystectomy (Table 66-4).76–87 A review of the experience with laparoscopic cholecystectomy in the United States showed an operative mortality rate of 0.06%. Internationally, operative mortality rates have ranged from 0% to 0.15%. Conversion to an open procedure was required in 2.2% in the United States and 3.6% to 8.2% of patients internationally, generally because of inflammation that precludes safe dissection of the porta hepatis. Major morbidity occurred in approximately 5% of patients, and bile duct injuries occurred in 0.14% to 0.5% of patients. Operating time ranged from one to two hours. Initially, most patients were observed overnight after laparoscopic cholecystectomy, but same-day discharge has become standard for elective cases. Most patients return to full activities, including work, within one week.
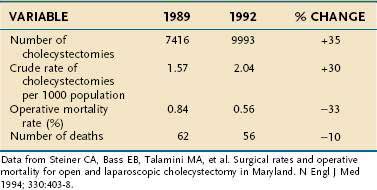
No randomized, prospective trials have compared the results of laparoscopic cholecystectomy with those of open cholecystectomy in the United States, nor are any likely. Patient enthusiasm for the laparoscopic approach and the rapid acceptance of the procedure by surgeons have made direct, controlled comparison of the two procedures difficult. Nonrandomized data from the United States and small, randomized trials from other countries support the contention that the laparoscopic approach is superior to the open approach.59,88–92 In these analyses, the main benefits of the laparoscopic approach have included a shortened hospital stay, decreased pain, reduced disability, and reduced costs. Population studies have shown a substantial decline in cholecystectomy-related mortality rates following the introduction of the laparoscopic technique (Table 66-5).93
Table 66-5 Cholecystectomy-Related Mortality in Maryland before (1989) and after (1992) the Introduction of Laparoscopic Cholecystectomy
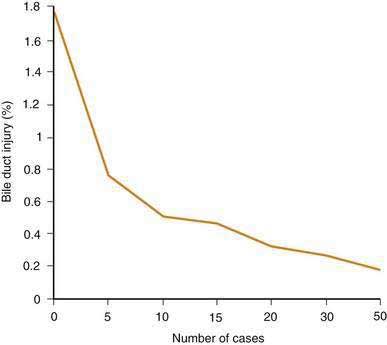
Against the perceived benefits of laparoscopic cholecystectomy over the open approach is concern about unacceptably high complication rates, especially for bile duct injury. Although the exact frequency of bile duct injury around the world is not known, two lines of evidence suggest that the rate has declined. First, regional studies have demonstrated a decrease in the rate of bile duct injury as overall experience with laparoscopic cholecystectomy has increased (Fig. 66-5).94 Curiously, however, the frequency of bile duct injury does not continue to fall with increasing experience of the individual surgeon, but rather plateaus.95–97 Although duct injuries are more common early in an individual surgeon’s experience, they still occur in the hands of seasoned surgeons, albeit at a lower rate. As overall experience has increased, the rate of bile duct injury for laparoscopic cholecystectomy has approximated that seen with open cholecystectomy. Second, the number of patients with bile duct injury treated at tertiary referral medical centers has declined since the early days of laparoscopic cholecystectomy.98 Introduction of laparoscopic cholecystectomy in the United States was rapid and may have exceeded the capability of the medical educational system to train all practitioners adequately. The initial relatively high rates of bile duct injury have been ascribed to a “learning curve.” This experience is a cautionary example for other new technologies that may be introduced into medical practice.
Concern has been raised about the increased use of laparoscopic cholecystectomy for gallstone disease when compared with historical rates for open cholecystectomy. In a defined health maintenance organization population in Pennsylvania, the rate of cholecystectomy increased from 1.35 per 1000 enrollees in 1988, just before the introduction of the laparoscopic approach, to 2.15 per 1000 enrollees in 1992, just after its introduction.99 No significant changes in the rates of herniorrhaphy or appendectomy were observed. Similarly, statewide data from Maryland have shown that the rate of cholecystectomy rose from 1.69 per 1000 residents in 1987 to 1989 to 2.17 per 1000 residents in 1992,93 and Scottish nationwide data have shown a 20% increase in the age-standardized rate of cholecystectomy.100 The reasons for the increases in use are not yet clear. The consensus of experts in the field is that selection of patients for cholecystectomy should not be altered by the availability of the laparoscopic approach.
INDICATIONS FOR TREATMENT
ASYMPTOMATIC GALLSTONES
Decisions regarding the management of the patient with asymptomatic gallstones must be predicated on knowledge of the natural history of the condition, as discussed in Chapter 65. In general, patients with asymptomatic gallstones should be reassured that life-threatening complications are uncommon and that symptoms related to the stones develop in only a minority of patients.101–105 In the event that an asymptomatic patient becomes symptomatic, the initial presentation is most often with uncomplicated biliary pain. In fact, most patients in whom complications of gallstones develop have antecedent biliary pain.106 Decision analysis calculations suggest that the risks of cholecystectomy approximate the potential benefit in preventing future serious sequelae of gallstones.107 These calculations were based on historical data regarding the outcome of open cholecystectomy; the rate of serious sequelae of gallstones was determined from long-term follow-up of a group of male faculty members at a major mid-western university. Whether these data are applicable to the more common female patient considering laparoscopic cholecystectomy today is not known. Nevertheless, the strategy of prophylactic cholecystectomy in all asymptomatic patients probably has no major advantage over the recommendation that cholecystectomy be limited to symptomatic patients.108,109 In addition, studies that have analyzed health-related quality of life do not support cholecystectomy for asymptomatic patients.110
In certain subgroups, the benefits of prophylactic cholecystectomy for asymptomatic gallstones may outweigh the risks. American Indians, for example, appear to have a rate of gallstone-associated gallbladder cancer high enough to justify prophylactic cholecystectomy.110 In morbidly obese persons as well as recipients of heart and lung transplants, complications of gallstone disease carry high morbidity rate, and prophylactic cholecystectomy may be indicated.111–113
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree