■ Elements of prior surgical history that may present intraoperative difficulties such as previous stomach, pancreas, or colonic operations, and prior antecolic or retrocolic bowel bypass reconstructions, must be elicited. Prior operative reports should be obtained and reviewed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ All patients should ideally undergo both abdominal–pelvic cross-sectional imaging as well as endoscopic examination with possible biopsies.
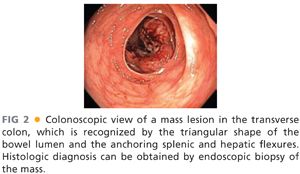
■ Endoscopic examination of the colon should be undertaken preoperatively to confirm the location and the focality of the pathology within the transverse colon (FIG 2).
■ Endoscopically, the transverse colon can be recognized by the triangular shape of the bowel lumen as well as by the anchoring landmarks of the splenic and hepatic flexures.
■ If there is any doubt as to whether the lesion will be able to be localized with confidence intraoperatively, then the lesion should be marked with endoscopic tattooing.
■ If there is any concern for involvement of adjacent organs, such as the stomach, an esophagogastroscopy should also be performed.3
■ Cross-sectional imaging of the abdomen is performed through computed tomography (CT) or magnetic resonance imaging (MRI) scans. Imaging characteristics may supplement histologic data and aid in the differential diagnosis. In addition, percutaneous biopsy may be needed.
■ In cases of malignant disease, imaging will help differentiate between colonic and noncolonic origin of the disease.
■ Presence of distant metastatic disease and evidence of direct local invasion to adjacent organs should be assessed and appropriate intraoperative management plans should be made.
■ Finally, any abnormal-appearing adenopathy along vessels other than the middle colic vascular should be specifically assessed in order to determine whether the particular malignancy would be better managed through an extended right or extended left colectomy rather than a transverse colectomy.
SURGICAL MANAGEMENT
■ Thorough preoperative preparation, confirming that the diagnosis is correct, the indication is appropriate, and that possible intraoperative findings have been anticipated and planned for, is the basis for successful intraoperative management and the speedy postoperative recovery.
Preoperative Planning
■ The operative surgeon should thoroughly review the patient’s history and diagnostic workup to minimize any unexpected and unplanned for intraoperative finding.
■ Diagnostic biopsy and histologic results should be verified. A malignant diagnosis should be particularly noted in order to help determine the extent of the bowel resection and lymphadenectomy.
■ Documentation from preoperative endoscopy should be reviewed, particularly if the operative surgeon did not perform the procedure. The presence and location of a marking tattoo should be confirmed.
■ Preoperative imaging is used to help anticipate any involvement of the adjacent organs and the possible need for en bloc resection intraoperatively. Any need for additional technical assistance from other surgeons should be planned for.
■ In cases of perforation and anticipated significant intraperitoneal contamination that may render bowel anastomosis unsafe, plans should be made for ostomy marking and education preoperatively.
■ Preoperative bowel preparation, whether antimicrobial and mechanical, mechanical only, or no preparation, is a highly variable practice and is left to the discretion of the practicing surgeon.
■ Prophylactic intravenous antibiotics with coverage against gram-positive, gram-negative, and anaerobic flora of the skin and gut are typically administered prior to incision and continued for the first 24 hours.
■ Prophylaxis against deep venous thrombosis is typically administered prior to incision and during the hospital stay.
Positioning
■ Patients are usually placed in a supine position. If there is any possibility of extending the resection to the left colon or any possible need for intraoperative endoscopy, consideration should be given for placing the patient in lithotomy position.
TECHNIQUES
INCISION AND ABDOMINAL EXPLORATION
■ A midline incision extending from the epigastrium to below the umbilicus is made.
■ The abdominal cavity is explored for the presence of other pathology not identified by preoperative imaging. In cases of malignant disease, peritoneal lining, omentum, and hepatic and bowel surfaces are inspected and palpated for any evidence of metastatic disease. In women, the pelvic organs, including the ovaries, should be inspected. Any suspicious nodule should be biopsied for pathologic assessment as findings may affect the decision of proceeding to the remaining of the procedure.
OMENTUM DISSECTION AND EXPOSURE OF THE LESSER SAC
■ The relationship between the transverse colon pathology and the lesser sac is assessed.
■ Exposure to the lesser sac is gained in one of two ways, depending on whether omentectomy is performed or not.
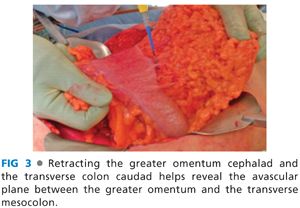
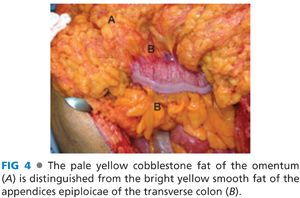
■ If disease pathology does not necessitate en bloc omentectomy or if there is desire to preserve as much of the omentum as possible, then greater omentum is retracted cephalad and the transverse colon is retracted caudad. This reveals the avascular plane between the greater omentum and the transverse mesocolon (FIG 3). The pale yellow omental fat is distinguished from the fat of the appendices epiploicae of the transverse colon (FIG 4). As this plane is dissected, the greater omentum is freed from the transverse colon and mesocolon and entrance into the lesser sac is gained. This can be confirmed by visualization of the posterior wall of the stomach dorsally and of the anterior surfaces of the duodenum, pancreas, and transverse mesocolon ventrally.
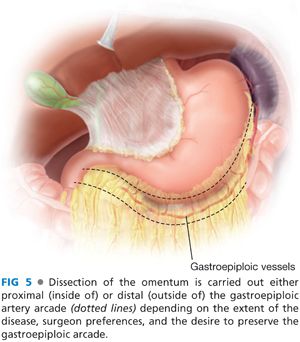
■ If the disease pathology necessitates en bloc resection of part or all of the omentum, then the gastrocolic ligament should be divided. The gastroepiploic artery arcade is identified along the greater curvature of the stomach. Dissection of the omentum is carried out either proximal (inside of) or distal (outside of) the arcade depending on the extent of the disease, the surgeon preference, and the desire to preserve the gastroepiploic arcade (FIG 5). The deeper avascular plane of the lesser sac, deep to the omentum but superficial to the transverse mesocolon, is entered. The omentum is thus isolated and divided between clamps.
MOBILIZATION OF THE HEPATIC FLEXURE AND THE SPLENIC FLEXURE
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








