■ A preoperative carcinoembryonic antigen level is obtained.
SURGICAL MANAGEMENT
Preoperative Preparation
■ Clinical trials have shown no need for mechanical bowel preparation.
■ Intravenous cefoxitin is administered within 1 hour of skin incision.
■ Use hair clippers if needed and chlorhexidine gluconate skin preparation.
■ Preoperative time-out and briefing is performed.
Equipment and Instrumentation
■ 5-mm camera with high-resolution monitors
■ 5-mm clear ports with balloon tips. They hold ports in the abdomen and minimize their intraabdominal profile during surgery.
■ Atraumatic graspers and laparoscopic endoscopic scissors
■ A blunt tip, 5-mm energy device
■ 60-mm linear reticulating laparoscopic staplers with vascular and tan loads
■ We use the GelPort hand-assist device due to its versatility and ease of use. This device allows for the introduction/removal of the hand without losing pneumoperitoneum.
Patient Positioning and Surgical Team Setup
■ This is the single most critical determinant of success in laparoscopic colorectal surgery (FIG 2).
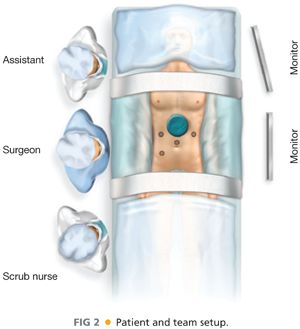
■ Place the patient on a supine position, with the arms tucked and padded (to avoid nerve/tendon injuries). The patient is taped over a towel across the chest without compromising chest expansion.
■ The surgeon starts at the patient’s right lower side with the scrub nurse to the surgeon’s right side. The assistant stands at the surgeon’s left side.
■ Align the surgeon, the ports, the targets, and the monitors in straight line. Place monitors in front of the surgeon and at eye level to prevent lower neck stress injuries.
■ Avoid unnecessary restrictions to potential team movement around the table. All energy device cables exit by the patient’s upper left side. All laparoscopic (gas, light cord, and camera) elements exit by the patient’s upper right side.
TECHNIQUES
PORT PLACEMENT AND OPERATIVE FIELD SETUP
■ Insert a GelPort through a 5- to 6-cm epigastric incision. This incision will be also used for specimen extraction, transection, and anastomosis. Placement in the epigastric area greatly facilitates dissection of the middle colic vessels through a supramesocolic approach (see step 7).
■ Insert three 5-mm working ports in the right upper, right lower, and left upper quadrants. Insert a 5-mm camera port above the umbilicus. Triangulate the ports so the camera port is at the apex of the triangle. This avoids conflict between the instruments and prevents disorientation (“working on a mirror”).
OPERATIVE STEPS
■ Our HALS transverse colectomy operation is highly standardized and it consists of nine steps:
■ Transection of the inferior mesenteric vein (IMV)
■ Medial to lateral dissection of the descending mesocolon
■ Transection of the left colic artery
■ Mobilization of the sigmoid off the pelvic inlet
■ Mobilization of the descending colon
■ Mobilization of the splenic flexure
■ Mobilization of the right colon
■ Transection of the middle colic vessels (supramesocolic approach)
■ Extracorporeal transection and anastomosis
Step 1. Transection of the Inferior Mesenteric Vein
■ This is the critical “point of entry” in this operation. At the level of the ligament of Treitz, the IMV is easy to visualize and is far from critical structures that can be injured during its dissection (no iliac vessels or left ureter nearby). This will be the only time when a true virgin tissue plane is entered. Every step will setup the following ones, opening the tissue planes sequentially.
■ The patient is placed on a steep Trendelenburg position with the left side up. Using the right hand, move the small bowel into the right upper quadrant (RUQ) and the transverse colon and omentum into the upper abdomen. If necessary, place a laparotomy pad to hold the bowel out of the field of view especially in obese patients. This pad can also be used to dry up the field and to clean the scope tip intracorporeally. Make sure that the circulating nurse notes the laparotomy pad in the abdomen on the white board.
■ Identify the critical anatomy: IMV, ligament of Treitz, and left colic artery (FIG 3).
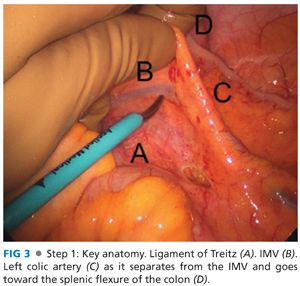
■ If there are attachments between the duodenum/root of mesentery and the mesocolon, transect them with laparoscopic scissors. This will allow for adequate exposure of midline structures.
■ Pick up the IMV with the left hand. Dissect under the IMV and in front of Gerota’s fascia with endoscopic scissors, starting at the level of the ligament of Treitz and proceeding toward the inferior mesenteric artery (IMA). The assistant provides upward traction with a grasper.
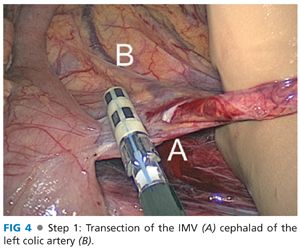
■ Transect the IMV cephalad of the left colic artery (which moves away from the IMV and toward the splenic flexure of the colon) with the 5-mm energy device (FIG 4), thus preserving intact the left-sided marginal arterial arcade and maintaining the blood supply to the descending colon segment.
Step 2. Medial to Lateral Dissection of the Descending Mesocolon
■ The surgeon’s hand and the assistant’s grasper retract the IMV/left colic pedicle at the cut edge of the descending mesocolon upwards towards the enterior abdominal wall. He or she then dissects the plane between the mesocolon and Gerota’s fascia (readily identified by the transition between the two fat planes) with a 5-mm energy device (FIG 5). We like to dissect this space by gently pushing the retroperitoneum down with the blunt tip of the 5-mm energy device.
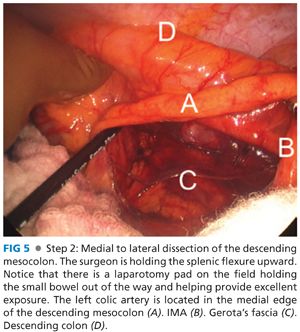
■ Dissect caudally under the IMV/left colic artery toward the takeoff of the left colic artery off the IMA. Dissect laterally until you reach the lateral abdominal wall. This will greatly facilitate step 5. Dissect superiorly between the splenic flexure and the tail of the pancreas. This will greatly facilitate step 6.
Step 3. Transection of the Left Colic Artery
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








