Chapter 76E Transjugular intrahepatic portosystemic shunting
Indications and technique
Indications
Variceal Bleeding
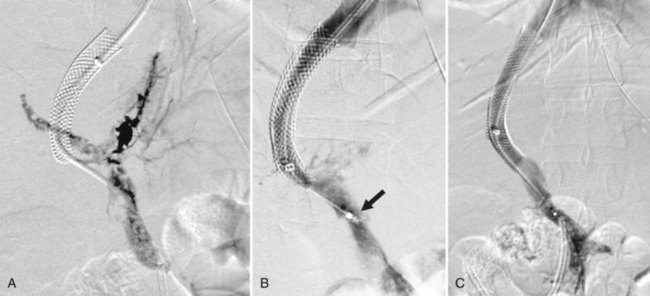
Bleeding gastroesophageal varices not controlled by medical or endoscopic means was the original indication for which TIPS was devised, and this is still the primary indication. TIPS can routinely decompress the portal system to drop the portosystemic gradient (PSG) and will lead to immediate cessation of bleeding in 95% of patients (Fig. 76E.1). A number of randomized trials have compared TIPS to best medical management (Cabrera et al, 1996; Cello et al, 1997; Garcia-Villarreal et al, 1999; Gulberg et al, 2002b; Jalan et al, 1997; Merli et al, 1998; Pomier-Layrargues et al, 2001; Rössle et al, 1997; Sanyal et al, 1997; Sauer et al, 1997). These have demonstrated that TIPS provides better long-term control of variceal bleeding. In these studies, recurrent bleeding occurred in 18% to 56% of patients in the sclerotherapy cohorts versus only 9% to 23% of patients in the TIPS arms. Not only were these differences statistically significant for the primary outcome, the crossover rate from endoscopy to TIPS was 5% to 28%, but only 0% to 7% of the TIPS patients crossed over to endoscopic treatment.
Better stratification of patients might also have yielded different results, as evidenced by one randomized trial (Monescillo et al, 2004) that stratified patients according to early measurement of their hepatic venous pressure gradient (HVPG) and then randomized high-risk patients (HVPG >20 mm Hg) to medical management or early TIPS placement. Not only did the TIPS group have fewer episodes of recurrent bleeding, both the in-hospital and 1 year mortality rates (11% and 38%) were significantly lower than in the non-TIPS cohort (38% and 65%).
One caveat regarding many of the randomized trials is that most were done using bare metal stents to create the shunt. Thus, within 6 to 12 months, the majority of the shunts in the TIPS group had stenosed. The current standard of care is to use stent grafts (polytetrafluoroethylene-covered stents) for TIPS procedures. These newer stent grafts have much improved patency and yield even better control of variceal bleeding than the bare metal TIPS (Angeloni et al, 2004; Angermayr et al, 2003; Bureau et al, 2007; Tripathi et al, 2006). Although more studies need to be done with stent grafts, at least one randomized trial (Garcia-Pagan et al, 2010) showed significantly better 1-year survival for TIPS performed with these improved stents compared with medical management (86% vs. 60%, P < .01).
The main downfall to TIPS is the development of new hepatic encephalopathy or exacerbation of existing encephalopathy, which occurs in 20% to 31% of cases (Boyer & Haskal, 2010). It is for this reason that TIPS is still recommended only after failure of medical management and not as front-line therapy for variceal bleeding. Interestingly, despite improved patency, the stent-graft TIPS has actually been associated with a lower incidence of encephalopathy compared with bare-stent TIPS (Bureau et al, 2007; Tripathi et al, 2006). This is another reason why the randomized trials comparing TIPS to medical management need to be repeated with the newer stent grafts.
Gastric Varices and Gastropathy
Gastric varices are also frequently seen in patients with portal hypertension and are actually associated with a higher rate of hemorrhage-related mortality compared with bleeding from esophageal varices (Garcia-Tsao & Bosch, 2010). TIPS can also provide good control of bleeding related to this condition, although the efficacy compared to endoscopic management is less clear. One large retrospective study comparing TIPS to endoscopic cyanoacrylate injection failed to demonstrate a benefit for TIPS in either control of bleeding or survival (Procaccini et al, 2009). However, another trial (Lo et al, 2007) that randomized patients to either TIPS or variceal obliteration with endoscopic cyanoacrylate injection showed that rebleeding was significantly less frequent in the TIPS group (11% vs. 38%, P = .014).
TIPS has also been used to treat portal hypertensive gastropathy, but data are sparse, and no randomized trials have evaluated the use of TIPS for this condition. Some investigators believe that TIPS is less effective for this condition, and several studies have a shown a poor correlation between HVPG and the presence or severity of gastropathy (Bellis et al, 2007; Shimizu et al, 2002). Given that the function of TIPS is to reduce portal pressure, this lack of correlation between the severity of gastropathy and portal pressures may account for the more variable results seen with TIPS in this condition.
Ectopic Varices
The effective portal decompression achieved by TIPS has led to expansion of the indication to include bleeding from ectopic varices, which most often arise in enteric stomas and are caused by portal hypertension transmitted to the peripheral tributaries of the mesenteric veins. Several small series have described successful treatment of varices in these locations by decompression with TIPS (Spier et al, 2008; Kochar et al, 2008; Han et al, 2007; Vidal et al, 2006; Macedo et al, 2005; Alkari et al, 2005; Vangeli et al, 2004; Ryu et al, 2000). The rebleeding rate in this indication is higher than expected after decompression of the portal system, which has led several authors (Kochar et al, 2008; Vangeli et al, 2004) to suggest that the ectopic varices should also be embolized at the time of TIPS.
Ascites
Although TIPS was designed to treat variceal bleeding, early investigators recognized that the procedure also led to a reduction or resolution of ascites in many patients. A number of randomized controlled trials have compared TIPS to large-volume paracentesis (LVP) (Ginés et al, 2002; Lebrec et al, 1996; Rössle et al, 2000; Salerno et al, 2004; Sanyal et al, 2003). A meta-analysis of these trials (Deltenre et al, 2005) showed that at 4 and 12 months, ascites was controlled in 66% and 55% of the TIPS patients, respectively, compared with 24% and 19% for the LVP patients. Despite the improved control of ascites, survival was higher, but not statistically better, in the TIPS groups. Another meta-analysis of the data did show a slight survival benefit for the TIPS patients (Salerno et al, 2007). Again, these studies were all done with bare metallic stents, and because survival is better after TIPS with stent grafts, these studies bear repeating with the current technology. Data from trials of stent grafts show improved control of ascites compared to bare-stent TIPS. Jung and colleagues (2009) reported ascites control at 1 year in 64% of TIPS procedures performed with the Viatorr device (W.L. Gore, Flagstaff, AZ) versus only 33% in patients with bare metal stents.
Patients with intractable ascites tend to be a sicker population, and despite successful decompression of the portal system, survival in this cohort is likely to be lower compared with those who have had TIPS done for variceal hemorrhage (Wallace et al, 2004); however, TIPS can still lead to significant improvement in quality of life (Gulberg et al, 2002a). One caveat is that the physiologic effect is not always immediate, and some patients do not show resolution of ascites for 2 to 3 months after the TIPS; another is that the clinical response does not appear to be as good when TIPS is used to treat recurrent ascites in patients after liver transplantation. One small retrospective study (Saad et al, 2010) reported a clinical success rate of only 16% in patients after transplant.
Hepatic Hydrothorax
Based on the success with managing ascites, TIPS has also been applied to hepatic hydrothorax, which occurs in 5% to 10% of cirrhotic patients and can lead to significant shortness of breath and inability to perform normal daily activities. Similar to ascites, TIPS is not used for primary therapy but instead is reserved for patients who are refractory to medical management. Patients requiring multiple thoracenteses or chest tubes can benefit from TIPS, with a beneficial response reported in 74% to 79% of patients undergoing the procedure (Dhanasekaran et al, 2010; Gordon et al, 1997; Spencer et al, 2002). Of those who respond, about two thirds have complete resolution of the hydrothorax, and the remainder experience partial resolution of the effusion but are symptomatically improved, with either decreased or resolved dyspnea. In our experience (Spencer et al, 2002), the patients who showed no clinical response to TIPS were all critically ill with elements of multiorgan failure, and 30-day mortality was 83%. Thus TIPS is unlikely to be helpful as a last-ditch effort to improve pulmonary function in severely ill patients on mechanical ventilation.
Budd-Chiari Syndrome
Since the early 1990s, TIPS has also been used to relieve the portal hypertension and hepatic congestion associated with Budd-Chiari syndrome (Ochs et al, 1993). The results obtained depend on the patient’s physiologic status. Several studies (Khuroo et al, 2005; Blum et al, 1995) have shown that a more fulminant presentation correlates with decreased survival; however, patients with a more chronic form of Budd-Chiari syndrome have fairly good results with TIPS. The largest series of TIPS done for Budd-Chiari syndrome included 124 patients (Garcia-Pagan et al, 2008b). The 1- and 10-year transplant-free survival rates were 88% and 69%. This was significantly better than expected for this patient population and has led to a change in the guidelines so that TIPS is now a recommended treatment in patients who fail anticoagulation therapy (Boyer & Haskal, 2010). This study also demonstrated that patients with a greater degree of hepatic dysfunction did not benefit as much as those with better preserved hepatic function.
Portal Vein Occlusion
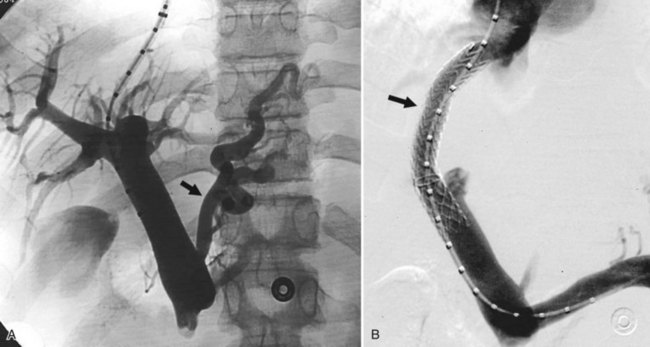
Portal vein (PV) occlusion is one indication for TIPS that sometimes arises even in patients without severe cirrhosis. The benefit of TIPS is that it provides a pathway into the portal system for introduction of mechanical thrombolytic devices (Fig. 76E.2) and also provides outflow to help maintain flow once portal patency is reestablished. TIPS has also been shown to be beneficial in treating portal hypertensive complications in patients with portal thrombosis who are awaiting liver transplantation (Bauer et al, 2006). The technical success rate for establishing a shunt and maintaining patency of the portal system is 70% to 100% (Bilbao et al, 2004; Radosevich et al, 1993), with the technical failures a result of the inability to traverse the portal occlusion. Clinical success—that is, termination of hemorrhage—was achieved in all patients in whom a TIPS was successfully created. This approach needs to be carefully considered in consult with a liver transplant surgeon and transplant hepatologist in transplant candidates, because TIPS placement in this setting can compromise access to the proximal PV, which has the potential to influence the outcome of liver replacement.
Preoperative Decompression
A relatively new application of TIPS has been for preoperative portal decompression in patients who need to undergo major intraabdominal, nonhepatic operations (see Chapter 70B; Azoulay et al, 2001; Gil et al, 2004; Schlenker et al, 2009). For patients with severe portal hypertension that requires colonic resection, the operative mortality can be quite high. Portal hypertension poses a risk in terms of dilated collateral veins, increased risk of operative bleeding, and the possibility of portal hypertension–related ascites, causing infectious complications or incisional ascites leakage postoperatively. In the reports of TIPS for this indication, the operations were carried out without excessive bleeding or ascitic complications.
One unresolved question concerns how much time to allow between the TIPS and the operation to ensure optimal decompression of the dilated collateral veins. Although waiting a few weeks after portal decompression seems prudent, one group reported safely operating 2 days after TIPS (Theruvath & Adams, 2010). Given that TIPS can cause complications of its own, it should not be utilized casually for preoperative decompression.
Contraindications
When medical and endoscopic methods have failed to control massive variceal hemorrhage, TIPS may be the only potentially lifesaving option. Thus most of the contraindications typically cited are only relative contraindications; however, if the indication for TIPS is nonemergent, these contraindications assume greater importance. Right heart failure is one of the most significant contraindications, because TIPS can precipitate acute death from total heart failure (Peron et al, 2000), but this complication has been reported so infrequently that it is impossible to define an absolute threshold for right heart pressures above which TIPS should not be performed.
Various authors have proposed schemes to decide prospectively who should be treated with TIPS (Harrod-Kim et al, 2006; Malinchoc et al, 2000; Montgomery et al, 2005; Pan et al, 2008). Of these, the MELD score tends to correlate best with 1-year survival (Chalasani et al, 2000). Different MELD scores have been proposed as the cutoff above which patients should not undergo TIPS, but these figures must be weighed against the risk inherent in the patient’s condition. In situations of life-threatening variceal hemorrhage, TIPS can often be life saving, even in a patient with a high MELD score.
Cavernous transformation is generally considered a contraindication, because it greatly increases the difficulty of gaining access to the portal system. Furthermore, even if a portal branch is accessed, it may be impossible to negotiate across the main PV occlusion to a portion of the portal system that is patent. Cases have been described in which a TIPS was created to a dilated periportal collateral with successful decompression of the portal hypertension (Brountzos et al, 2004; Wils, et al, 2009). Detailed preprocedure cross-sectional imaging can be useful to assess for the presence of a large, dominant collateral that can act as a target for the shunt.
Polycystic liver disease has been listed as an absolute contraindication because of potential intracystic hemorrhage, although successful TIPS in polycystic livers has been reported by us and others (Bahramipour et al, 2000; Shin & Darcy, 2001; Sze et al, 2006); some of these were even done with bare metallic stents without significant bleeding despite needle entry into the cyst cavity during creation of the parenchymal tract. The reason for the lack of intracystic hemorrhage would appear to be that the shunt provides a low-resistance pathway to the right atrium, and there is little reason for blood to flow into the contained space of a cyst. Although technically challenging, evidence is insufficient to suggest that polycystic liver disease should continue to be listed as a contraindication.