■ Low-risk T1 disease—Definitive therapy for rectal cancer should be reserved only for patients with low-risk T1 disease. This is also the current position of the National Comprehensive Cancer Network (NCCN).
■ High-risk T1 or any T2 disease with combination therapy—Patients with high-risk T1 or any T2 disease who undergo TEM with curative intent should ideally be treated in a clinical trial setting with either preoperative or postoperative chemoradiation. Given that TEM is not the standard of care in this setting, the risks and benefits of TEM versus radical resection need to be carefully discussed with the patient and appropriate consent obtained and documented.
■ Lesions of any stage, technically amenable to TEM, in patients who refuse radical resection, appropriate discussion and consent must be documented
■ Lesions of any stage, technically amenable to TEM, for palliative purposes
■ Other less common indications that have been reported include rectal carcinoids, endometriomas, angiodysplasia, rectal ulcers, rectal strictures, and other benign pathologies. Just as with rectal adenocarcinoma, the decision to perform TEM in these settings should be based on sound clinical judgment.
Anatomic Considerations
■ TEM is ideally suited for lesions whose entire extent falls within 5 to 15 cm from the anal verge.
■ The technical “sweet spot” for TEM is between 6 and 10 cm (midrectum), beyond which the surgeon has to contend with instrument limitations, diminished visualization and exposure, and the potential for peritoneal entry.
■ TEM has been described for lesions proximal to 15 cm. However, peritoneal entry is much more likely with full-thickness excision in this setting, and extensive expertise is required to perform an adequate and safe suture repair.
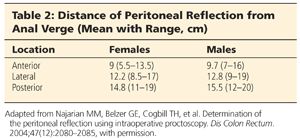
■ The likelihood of peritoneal entry is dependent on the circumferential location of the lesion (Table 2). For example, the mean distance to the peritoneal reflection anteriorly in men is at 9.7 cm, compared to 15.5 cm posteriorly. Dissection in the posterior midline can also result in entry into the intraabdominal colonic mesentery, without frank intraperitoneal entry.3
■ Lesions distal to 5 cm are usually covered in part or completely by the transanal access device. These lesions are more suited for conventional TAE.
■ There is no absolute contraindication based on the total circumferential extent of the lesion, and complete circumferential excisions have been described. However, excision of lesions that occupy more than 40% of the circumference is technically much more challenging, may be associated with more advanced lesions, and can lead to compromised margins. Sound judgment and careful patient selection are required.
Preoperative Preparation
■ The key to the technical success of the TEM operation is adequate visualization and exposure. As a result, preoperative mechanical bowel preparation is invaluable. We ask our patients to have a normal lunch and take a clear liquid diet with adequate hydration thereafter and nothing by mouth after midnight. We prefer a mechanical bowel preparation with two bottles of magnesium citrate in the afternoon the day before surgery, with a Fleet enema the night before and the morning of the procedure.
■ In addition, we administered one dose of IV cefoxitin antibiotic within 1 hour of initiation of surgery.
■ Appropriate informed consent should be obtained. In addition to the possibility of the more common complications, the consent should also address the following:
■ The likelihood of technical success of the procedure
■ The potential need for reoperation based on pathologic findings (either repeat TEM or radical resection)
■ Oncologic outcomes in comparison to radical resection, particularly local recurrence
■ The likelihood of peritoneal entry for upper rectal lesions. For upper rectal lesions where peritoneal entry is a significant possibility, we routinely consent for possible laparoscopy and/or laparotomy with primary repair or radical resection.
Positioning
■ Appropriate patient positioning is critical to the technical success of the procedure. Every effort should be made to position the patient such that the lesion is down at the 6 o’clock position.
■ For posterior lesions, we prefer a high lithotomy position (FIG 1A).
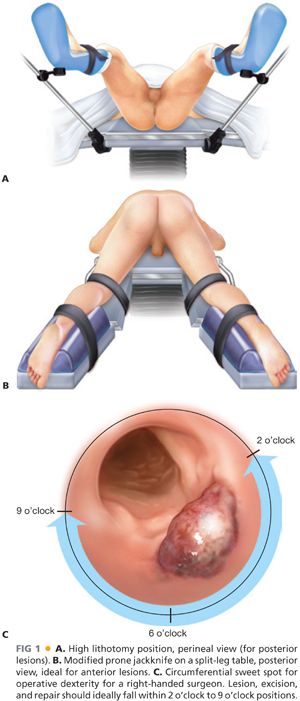
■ For anterior lesions, we prefer to place the patient in prone jackknife position on a split-leg table, with the surgeon positioned between the legs (FIG 1B).
■ For lateral lesions, we place the patient in either one of the aforementioned positions and rotate the table to turn the lesion to 6 o’clock as much as possible. If the lesion cannot be placed completely down, then we have found that it is easier to perform the excision, as well as the repair, when the lesion is oriented toward the dominant hand of the surgeon. The “circumferential sweet spot” for a right-handed surgeon in our experience is presented in FIG 1C.
Equipment
■ Multiple transanal access platforms have been used and are appropriate for TEM. The standard procedure described by Buess et al.2 uses the operating transanal proctoscope by Wolf. Other transanal access platforms that have been used have incorporated equipment for single-incision laparoscopic surgery. These platforms have now gained U.S. Food and Drug Administration (FDA) approval for transanal access. Although we have used a number of these systems, our preferred transanal access platform is currently the GelPOINT Path system manufactured by Applied Medical.
■ We routinely use both standard and articulating laparoscopic instruments designed for single-incision laparoscopic surgery. In a typical case, we often use a 5-mm scope operated by the assistant, a standard Maryland grasper in the left surgeon’s hand for grasping and retraction, and an articulating hook cautery or harmonic scalpel in the right surgeon’s hand for excision. For repair, we use a standard laparoscopic needle driver.
■ Our preferred energy sources are monopolar cautery and ultrasonic shears such as a harmonic scalpel.
TECHNIQUES
■ The patient is placed under general endotracheal anesthesia, a Foley catheter is routinely inserted, and the patient is appropriately positioned.
■ A minimal sterile preparation of the perineum is performed, and the patient is draped in standard fashion.
■ We perform an intersphincteric block with 1% lidocaine with epinephrine.
■ The transanal access port is heavily lubricated, folded in and grasped from inside the port with a ring clamp (FIG 2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








