■ Rectal protocol magnetic resonance imaging (MRI) is increasingly used in rectal cancer staging due to its ability to assess, in addition to T and N stages, potential adjacent organ involvement and the relationship with the mesorectal margin (FIG 2). However, MRI, like ERUS, is challenged in trying to differentiate between T1 and T2 stages due to the limited resolution in delineating the layers of the rectal wall.

■ If the patient has a malignant lesion that is unfavorable (≥T3 or N+) at any level in the rectum or a favorable cancer in the distal one-third of the rectum (0.5 to 6.0 cm above the anorectal ring), neoadjuvant chemoradiation is recommended. Surgical decision making is based on the evaluation of the tumor at 8 to 12 weeks after completion of neoadjuvant chemoradiation in order to maximize the effect of tumor downstaging.
■ Table 1 summarizes the ideal TEM candidates as well as the absolute contraindications for TEM. In general, local excision is the preferred option for patients with adenoma, or cancer with favorable features (≤3 cm in diameter; T1, grade I or II, and no venous or lymphatic invasion; and no evidence of lymph node metastasis) after chemoradiation. An ideal patient for local excision has a tumor that is small, mobile, located in the distal rectum, and posteriorly based.
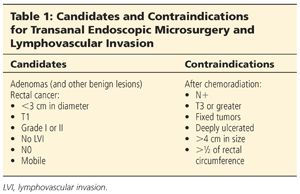
■ Contraindications for patients to undergo a TEM procedure after completion of neoadjuvant radiation include lymph node involvement, T3 or greater cancer after neoadjuvant chemoradiation, or tumors that remain fixed, deeply ulcerated, or have adjacent visceral organ involvement. In general, a maximum size of 4 cm is considered the limit for TEM after chemoradiation. Tumors greater than 3 to 4 cm in size can be challenging to excise transanally after neoadjuvant therapy due to the difficulty in closing the large defect that might be greater than one-half the circumference of the rectal wall.
SURGICAL MANAGEMENT
Preoperative Planning
■ Patient preparation for TEM is the same for benign or malignant lesions.
■ The patient will undergo standard bowel preparation.
■ Standard preoperative antibiotics are administered.
■ It is important to have a conversation with the patient preoperatively to discuss the potential need for laparoscopy or laparotomy and a possible diverting stoma.
Patient Positioning
■ The positioning of the patient depends on the tumor location. In general, the patient is positioned so that the tumor is in the dependent position during the procedure.
■ The tumor should be at the center of the operating rectoscope throughout the procedure; the bevel of the TEM scope should face down at the tumor. This is essential as the optics reside in the upper portion of the operating proctoscope, limiting the reach of the instruments to the bottom 180 to 210 degrees of the lumen. Therefore, patient positioning becomes very important.
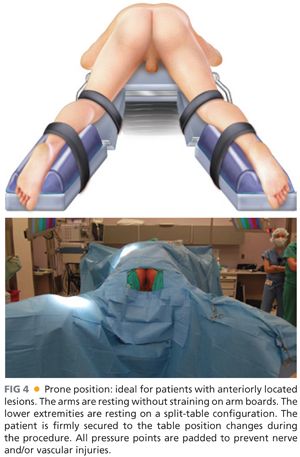
■ Patients with posterior lesions are placed in the modified lithotomy position (FIG 3). Patients with anterior lesions are placed in the prone position (FIG 4). Patients with left or right lateral lesions are placed in the left or right decubitus position, respectfully.

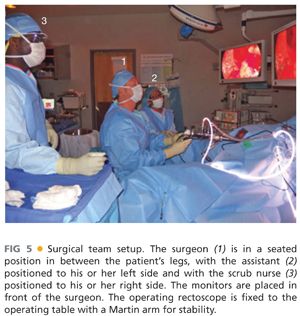
Operating Team Setup
■ The surgeon should be in a seated position in between the patient’s legs (FIG 5). The assistant should be seated to the left of the surgeon. The scrub nurse is to be positioned opposite the endosurgical unit. The monitors are placed in front of the surgeon.
TECHNIQUES
TRANSANAL ENDOSCOPIC MICROSURGERY SETUP
■ All of the instruments that we use during the TEM procedure are from the Richard Wolf TEM Instrument System. Some of the instruments used to do the dissection are displayed in FIG 6. However, similar instruments and equipment are offered by Karl Storz and others use standard laparoscopic instruments.

■ The operating rectoscope has a rectoscope tube that is 4 cm in diameter (FIG 7A). There are three different lengths of shafts (with their correspondent obturators; FIG 7B) that can be used during the surgery, depending how far the tumor is from the anal sphincter. The rectoscope tube is attached to the adapter and working insert (FIG 7B) and is then fixed to the operating table with a Martin arm (FIG 5).
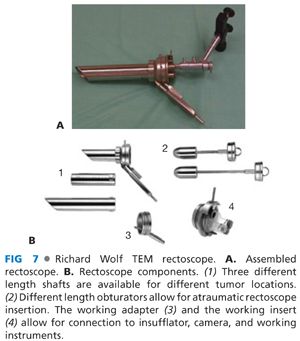
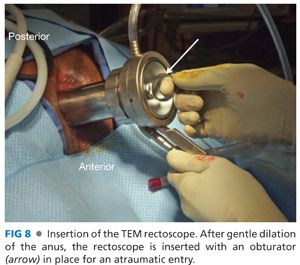
■ Once the patient is prepped and draped, the anus is gently dilated and the rectoscope (with the obturator) is inserted into the patient’s anus (FIG 8). There is a 20-cm shaft with an oblique edge for higher lesions, a 12-cm shaft with an oblique edge for masses lower in the rectum, and a 13.7-cm shaft with a flat edge for lesions that extend into the anus (FIG 7B). The flat-edged shaft is ideal for very low lesions, as it allows access without losing insufflation extending down to the upper anus. The obturator can be removed and the working faceplate is secured.
■ The light source is then connected and the rectum is insufflated. At this point, the TEM is functioning as a large rigid proctoscope. The scope can then be adjusted so that the lesion is positioned in the center of view at the 6 o’clock position (FIG 9). This assures that the positioning is ideal and that the surgeon will have proper reach with the instruments.

■ After the ideal view of the lesion is found, the TEM scope is then secured to a Martin arm (FIG 5), and this arm is connected to the operating table. The application of the Martin arm is one of the most important aspects of the operation, as the arm is frequently repositioned to keep the lesion in the lower middle of the field, as explained earlier. It is essential to make certain that each of the three joints on the Martin arm is not maximally angled so as to maintain flexibility of positioning. If they are maximally flexed, the arm needs to be adjusted.
■ All of the rubber sleeves and caps can then be lubricated with mineral oil to reduce the chances of drying and cracking. If the caps tear, it will lead to air leaking and loss of rectal distention. After lubrication, the sleeves and caps are placed into the ports on the faceplate.
■ Lastly, the four pieces of tubing can be placed into their respective ports in the apparatus (FIG 10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








