■ Care is taken to identify, and avoid damage to, the right gonadal vessels, the right ureter, and the duodenum.
TRANSVERSE COLON MOBILIZATION
■ The hepatic flexure is mobilized by dividing adhesions between the gallbladder and liver. Gentle traction on the hepatocolic ligament exposes the hepatocolic ligament, which is then transected with electrocautery (FIG 2).

■ The gastrocolic ligament is exposed as the assistant retracts the greater omentum superiorly while the surgeon retracts the transverse colon anteroinferiorly.
■ Diathermy is used to separate the greater omentum from the anterior leaf of the transverse mesocolon.
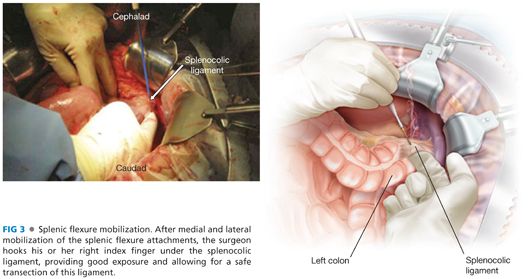
■ The splenocolic ligament is divided as close to the colon as feasible, avoiding undue traction on the spleen. The splenocolic ligament needs to be approached from both sides to facilitate ease of mobilization of the splenic flexure. Once the gastrocolic ligament has been completely transected, transection of the lateral peritoneal attachments allows for mobilization of the splenic flexure. At this point and from the right side of the table, the surgeon hooks the splenocolic ligament anteriorly with his or her right index finger, exposing the ligament adequately for the assistant to transect it using electrocautery (FIG 3).
PROXIMAL DIVISION
■ The terminal ileum is mobilized by division of surrounding adhesions proceeding with the dissection toward the root of the mesentery.
■ The ileocolic pedicle (and right colic pedicle, if present) is identified and clamped with heavy artery forceps by creating windows on either side with diathermy (FIG 4).
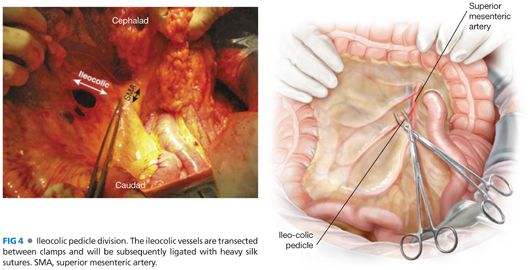
■ The pedicle is divided between the artery forceps and ligated proximally and distally with absorbable braided, size 0 ties.
■ Alternatively, if the surgeon is certain of the absence of malignancy, then the mesenteric blood supply to the proximal segment can be taken close to the bowel wall.
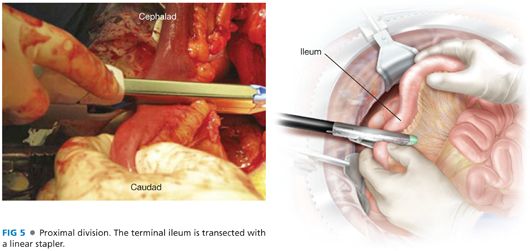
■ The terminal ileum is transected with a single firing of a linear stapler, such as gastrointestinal anastomosis (GIA) 60-3.5 stapler or GIA 60-4.8 if the ileum is thickened or inflamed (FIG 5).
■ The ascending colon mesentery is divided, proceeding from proximal to distal until the middle colic pedicle is encountered.
■ The middle colic pedicle is clamped with heavy artery forceps by creating windows on either side with diathermy.
■ The pedicle is divided between the artery forceps and ligated proximally and distally with absorbable braided, size 0 ties.
DESCENDING COLON MOBILIZATION
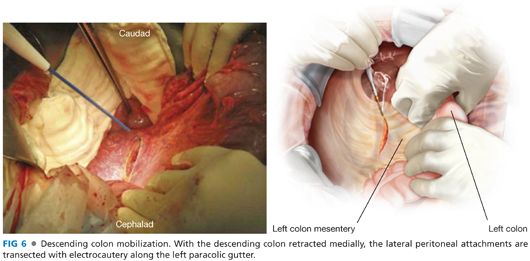
■ The descending colon is mobilized by medial traction and dissection along the left paracolic gutter using diathermy (FIG 6).
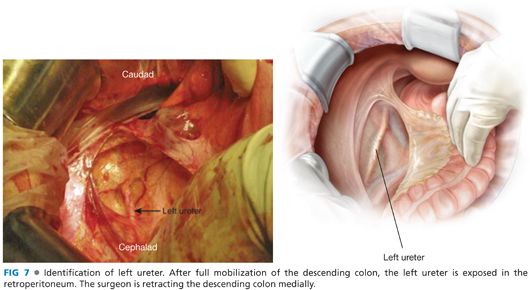
■ Care is taken to identify, and avoid damage to, the left gonadal vessels and left ureter (FIG 7).
■ Dissection is stopped at the rectosigmoid junction.
DISTAL DIVISION
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








