■ Place the legs on Allen stirrup with the heels firmly planted on the stirrups to avoid pressure on the calves and the lateral peroneal nerves.
■ Keep the thighs parallel to the ground to avoid conflict between the thighs and the surgeon’s arms/instruments.
■ The coccyx should be readily palpable off the edge of the table.
■ The surgeon starts at the patient’s right lower side, with the assistant to his or her left side and with the scrub nurse to his or her right or in between the patient’s legs (FIG 2).
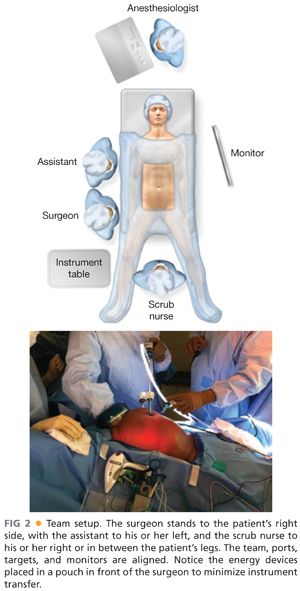
■ Align the surgeon, ports, targets, and monitors in straight lines. Place monitors in front of the surgeon and at eye level to prevent lower neck stress injuries.
■ Avoid unnecessary restrictions to potential team movement around the table. All energy device cables exit by the patient’s upper left side. All laparoscopic (gas, light cord, and camera) elements exit by the patient’s upper right side.
■ The energy instruments are placed in a plastic pouch in front of the surgeon to avoid unnecessary instrument transfer during the operation (FIG 2).
TECHNIQUES
PORT PLACEMENT AND OPERATIVE FIELD SETUP
■ Insert the GelPort through a 5- to 6-cm Pfannenstiel incision (FIG 3). This incision will be also used for specimen extraction. It provides a better cosmetic result and lowers the incidence of wound infections and incisional hernias. It also allows for more working space between the hand and the instruments. Alternatively, the GelPort can also be inserted in the epigastrium, if access to the middle colic vessels is of concern.
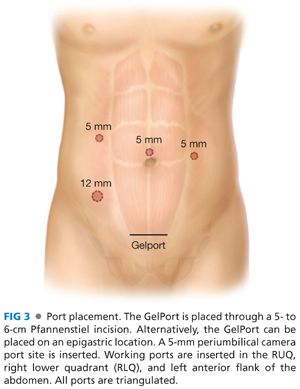
■ Ports: Insert a 5-mm working port in the right upper quadrant (RUQ), a 12-mm working port in the right lower quadrant, and a 5-mm camera port above the umbilicus. These three ports are triangulated, with the camera port at the apex of the triangle. This setup avoids conflict between the instruments and the camera and prevents disorientation (avoids “working on a mirror”). A third 5-mm working port is inserted in the left anterior flank of the abdomen for the mobilization of the right colon; it can also be valuable for the mobilization of the splenic flexure in patients with deep left upper quadrants.
OPERATIVE STEPS
■ Our HALS TAC operation is highly standardized and consists of 13 steps. After the initial point of entry, every step will expose the necessary planes of dissection for the following steps, ensuring that no truly virgin tissue planes are encountered anymore, thus greatly reducing the complexity of this operation. These steps, in order, are as follows:
■ Transection of the inferior mesenteric vein (IMV)
■ Transection of the inferior mesenteric artery (IMA)
■ Medial to lateral dissection of the descending mesocolon
■ Lateral mobilization of the sigmoid and descending colon
■ Mobilization of the splenic flexure and transverse colon
■ Mobilization of the hepatic flexure
■ Supramesocolic transection of the middle colic vessels
■ Transection of the ileocolic pedicle
■ Medial to lateral mobilization of the ascending colon
■ Lateral mobilization of the ascending colon
■ Intracorporeal distal transection
■ Extracorporeal mobilization and proximal transection
■ Intracorporeal ileorectal anastomosis
Step 1. Transection of the Inferior Mesenteric Vein
■ This is the critical “point of entry” in this operation. We favor it over starting dissection at the IMA level due to the IMV’s constancy in location, the ease of its visualization by the ligament of Treitz, and the absence of structures that can be injured around it (no iliac vessels or left ureter nearby). This will be the only time during the operation when a virgin tissue plane is entered. Every step will set up the following ones, opening the tissue planes sequentially.
■ The patient is placed on a steep Trendelenburg position with the left side up. Using the right hand, move the small bowel into the RUQ and the transverse colon and omentum into the upper abdomen. If necessary, place a laparotomy pad to hold the bowel out of the field of view, especially in obese patients. This pad can also be used to dry up the field and to clean the scope tip intracorporeally. Make sure that the circulating nurse notes the laparotomy pad in the abdomen on the white board.
■ Identify the critical anatomy: IMV, ligament of Treitz, and left colic artery (FIG 4).

■ If there are attachments between the duodenum/root of mesentery and mesocolon, transect them with laparoscopic scissors. This will allow for adequate exposure of midline structures
■ Pick up the IMV with the right hand. Dissect under (dorsal) the IMV and in front of Gerota’s fascia with endoscopic scissors, starting at the level of the ligament of Treitz and proceeding with the dissection caudally toward the IMA. The assistant provides upward countertraction with a grasper.
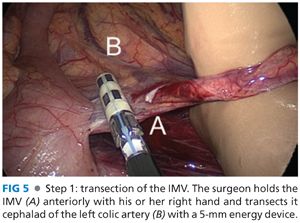
■ Transect the IMV (FIG 5) cephalad of left colic artery, which moves away from the IMV and toward the splenic flexure of the colon, with the 5-mm energy device.
Step 2. Transection of the Inferior Mesenteric Artery
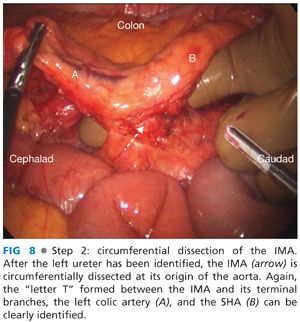
■ Identify the critical anatomy: the “letter T” formed between the IMA and its left colic and superior hemorrhoidal artery (SHA) terminal branches (FIG 6).
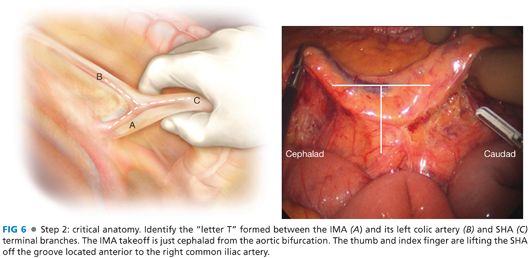
■ Using the right hand, the aorta is identified and tracked down to the level of its bifurcation. The IMA will originate 1 to 2 cm proximal to this level.
■ Holding the SHA up with the right hand, dissect the plane along the palpable groove between the SHA and the left iliac artery using laparoscopic scissors. A wide incision is made in the peritoneum dorsal to the SHA; the wider the incision, the easier the SHA can be elevated to obtain better exposure. After scoring the peritoneum under the SHA, use a 5-mm energy device to dissect by gently pushing the retroperitoneal tissues downward (dorsally) along the avascular plane located between the mesodescending colon, anteriorly, and the retroperitoneum, posteriorly. This avascular plane can be identified by the transition between the two distinctive fat planes of the mesocolon and Gerota’s fascia.
■ Preserve the sympathetic nerve trunk intact in the retroperitoneum. This avoids autonomic dysfunction postoperatively.
■ Identify the left ureter (FIG 7), located in front of the left iliac artery and psoas muscle and medial to the gonadal vessels, before transecting anything. If you are directly on the psoas muscle, chances are that you left the left ureter attached to the dorsal surface of the mesocolon; bring it down into the retroperitoneum gently using blunt dissection with the energy device.
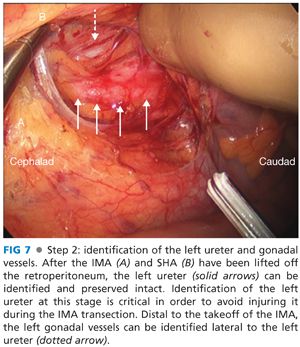
■ If you cannot identify the ureter, try dissecting superior to inferior, starting from the IMV plane of dissection and moving caudally behind the IMA. If you still cannot find it, perform a lateral to medial mobilization of the sigmoid colon toward the midline. In this latter scenario, you will encounter the left gonadal vessels first, lateral to the left ureter.
■ Dissect with your thumb and index finger around and behind the IMA and again visualize the letter “T” formed between the IMA, the left colic artery, and the SHA (FIG 8).
■ With the left ureter safely preserved in the retroperitoneum, transect the IMA at its origin with a vascular load stapler (FIG 9) or energy device. This ensures excellent lymph node harvest and allows great exposure for the following step.

Step 3. Medial to Lateral Dissection of the Descending Mesocolon
■ The surgeon’s right hand and the assistant’s grasper hold the descending mesocolon up, creating a working space between the mesocolon and the retroperitoneum (FIG 10). The plane between the mesocolon and Gerota’s fascia, readily identified by the transition between the two fat planes, is dissected bluntly in a downward direction toward the retroperitoneum with the 5-mm energy device.
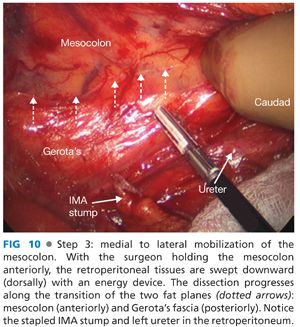
■ Dissect laterally until you reach the lateral abdominal wall, caudally toward the pelvic inlet, and cephalad until you separate the splenic flexure from the tail of the pancreas. Completing this step will greatly facilitate performance of steps 4 and 5.
Step 4. Lateral Mobilization of the Sigmoid and Descending Colon
■ The surgeon pulls the sigmoid colon medially, exposing the lateral sigmoid colon attachments (FIG 11A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








