The disease of obesity has continued to increase in the United States. Obesity is defined as a body mass index (BMI) greater than 30 kg/m 2 . In 1991, the National Institute of Health Consensus Panel on Gastric Surgery for Severe Obesity defined the population who would most likely benefit from bariatric surgery. These same criteria continue to be used today to determine which patients should undergo metabolic and weight loss surgery. These recommendations include patients who have a BMI greater than 35 kg/m 2 with significant comorbid conditions such as diabetes, hypertension, or obstructive sleep apnea; and patients who have a BMI greater than 40 kg/m 2 with or without any significant comorbid conditions because they have a significant increased risk for developing these conditions.
The disease of obesity has continued to increase in the United States. Obesity is defined as a body mass index (BMI) greater than 30 kg/m 2 . In 1991, the National Institute of Health Consensus Panel on Gastric Surgery for Severe Obesity defined the population who would most likely benefit from bariatric surgery. These same criteria continue to be used today to determine which patients should undergo metabolic and weight loss surgery. These recommendations include patients who have a BMI greater than 35 kg/m 2 with significant comorbid conditions such as diabetes, hypertension, or obstructive sleep apnea; and patients who have a BMI greater than 40 kg/m 2 with or without any significant comorbid conditions because they have a significant increased risk for developing these conditions.
Over the past 20 years the rate of obesity has shown a dramatic increase. The most recent statistics show that 32 states now have obesity rates greater than 25% of the adult population. Six states have obesity rates greater than 30% of the adult population and only one state, Colorado, has an obesity rate less than 20%. This means that 72 million American adults have a body mass index (BMI) of 30 kg/m 2 or greater. A closer evaluation of the statistics shows that a significant BMI shift has occurred so that the entire adult population is heavier. More worrisome is that the heaviest people have become much heavier over the past 20 years. Furthermore, disparities clearly exist among racial and ethnic populations, with a disproportionately high number of non-Hispanic black and Mexican American women in the morbid obesity range.
No significant improvements have occurred in the dietary approach to long-term weight loss over the past few years. Several dietary medications are still available; however, the success rate of dieting with behavioral changes alone and in combination with medications continues to be in the single digits.
Bariatric surgery has gained widespread acceptance. Evidence continues to show that it is the only treatment currently available with significant cure rates for diseases such as diabetes, hypertension, and heart failure, and myriad other comorbid conditions associated with obesity. Increasing evidence shows significant risk reduction for many cancers associated with obesity within 1 year of the significant weight loss associated with metabolic surgery.
Although bariatric surgery has been performed for more than 40 years, in 1995 Pories and colleagues showed that the procedure provided durable weight loss of more than 100 pounds, significant improvement in comorbidities, including diabetes, and a decrease in overall mortality among 608 patients who underwent gastric bypass over 14 years. Since that seminal report, surgery began to gain more acceptance as a viable treatment option.
In 1994, Clark and Wittgrove showed that gastric bypass could be performed safely laparoscopically and now most gastric bypasses and nearly all gastric banding procedures are performed using this technique. Finally, the nationwide acceptance of centers of excellence credentialed by the American College of Surgeons and the Surgical Review Corporation, where high volumes of surgery are performed by experienced surgeons, has proven that surgical risk and complications can be kept to an acceptably minimal level.
In a recent study, the LABS consortium reviewed 30-day outcomes from 10 centers for 4610 surgical procedures: 3412 gastric bypass and 1198 laparoscopic adjustable gastric bandings. The combined 30-day mortality was 0.3%, with a major complication rate of only 4.3%.
Lastly, although bariatric surgery has a higher risk than the nonoperative treatments of obesity, the definition of success is more stringently applied. For the nonoperative treatment of obesity, a 10% excess body weight loss maintained for 1 year is considered successful; this would be equal to a 220-pound patient, whose ideal weight is 120 pounds, losing 10 pounds and maintaining that weight loss for 1 year. The likelihood of this success is approximately 5%, with a 95% rate of failure. The definition of success for bariatric surgery is a loss of at least 50% of the excess body weight. Pooled data show a 54% to 67% excess body weight loss, depending on the type of surgery, that is maintained over a 10-year period with no evidence of loss of effect.
This article reviews the weight loss surgery options, beginning with the common operations performed currently, and then briefly discussing operations that are no longer performed.
Operations commonly performed currently
Roux-en-Y Gastric Bypass
Roux-en-Y gastric bypass is the most commonly performed bariatric operation in the United States ( Fig. 1 ). It is considered the gold standard operation to which all other operations are compared. It can be performed in a laparoscopic or the traditional open technique. This procedure considered restrictive and malabsorptive. The restrictive component to this operation entails creating a 20- to 30-mL gastric pouch just below the gastroesophageal junction. This pouch is either partitioned from the lower portion of the stomach or, more commonly, completely divided away from the lower, remnant stomach. The jejunum is then divided 30 to 50 cm distal to the ligament of Treitz, and the distal side of this division brought into the upper abdomen and anastomosed to the gastric pouch. This anastomosis can be performed with staplers or by simple sewing techniques. The proximal jejunal limb, which carries gastric secretions and biliopancreatic secretions, is then anastomosed back to the jejunum 75 to 150 cm from the gastrojejunal anastomosis. This technique provides the malabsorptive component of the operation by preventing the mixing of food and digestive enzymes as food or drink traverses the Roux limb.
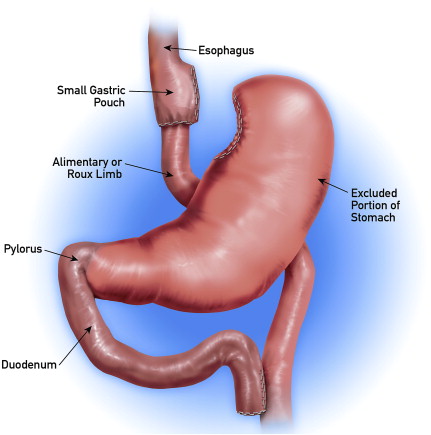
Because the laparoscopic approach has become the most common method of gastric bypass and completely divides the gastric pouch away from the distal, remnant stomach, the complication of staple-line dehiscence or gastro–gastric fistula will likely become far less common. The complete separation of the distal remnant stomach makes it much more difficult to access using an endoscopic technique. In addition, benefits of the laparoscopic approach include shorter hospitalization, decreased pain, and significant reduction in the rate of abdominal wall hernia.
Results and Outcomes
Roux-en-Y gastric bypass is a very effective operation, and the authors routinely see 50% excess body weight loss in the first 6 months after surgery. An approximately 75% excess body weight loss is common over the first 18 months, with an approximately 10% weight regain by the fourth or fifth year postoperatively.
As for comorbidity resolution, in a meta-analysis involving 136 studies with 22,000 patients, Buchwald and colleagues showed improvement in fasting blood glucose and hemoglobin A1C in 83% of patients, improvement of hyperlipidemia in 87% of patients, resolution of hypertension in 67.5% patients, and resolution or improvement of sleep apnea in 94% of patients.
Although the overall complication rate has been reported to be as high as 24%, it involves a significant portion of minor complications, such as early postoperative dehydration and nausea. The rate of major complications, such as deep vein thrombosis, pulmonary embolism, and bleeding requiring a transfusion or readmission to the hospital, is approximately 9%. The mortality rate for gastric bypass has been reported to be between 0.5% and 2% in all studies. The most common long-term complications include internal hernias and marginal ulceration at the gastrojejunal anastamosis. Postoperative nutritional deficiencies depend on several factors, such preoperative nutritional status, ability to modify eating behavior, and compliance with prescribed vitamin and mineral supplementation. Nutritional deficiencies are discussed in more detail in the article by Koch and colleagues appearing elsewhere in this issue.
Laparoscopic adjustable gastric banding
The adjustable gastric band was first developed by Kuzmak in the early 1980s. It was a later refined to include a saline-filled bladder within a band that encircles the upper portion of the stomach in a belt-like fashion. The saline-filled bladder is attached to tubing that runs to a reservoir in the subcutaneous tissue. The bladder is adjusted through accessing the reservoir ( Fig. 2 ). The band that encircles the stomach creates a small proximal gastric pouch, which can hold 2 to 3 ounces of solid food. The outflow through the band is adjusted through adding saline through the subcutaneous reservoir. The band therefore limits intake by causing a rapid feeling of satiety with relatively small meals.
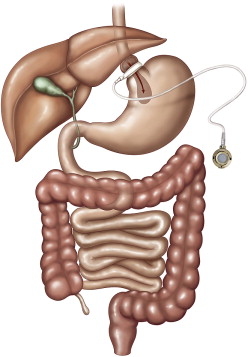
A decrease in appetite is also commonly reported, and is noticed by almost all patients when the band is appropriately adjusted. Patients who have well-adjusted bands frequently report no hunger until early afternoon or even later. They also routinely eat only two meals per day that are relatively small volume in size.
Result and Outcomes
The laparoscopic adjustable gastric band has the lowest complication rate of all bariatric operations, with a 12% rate of late complications, such as gastric prolapse, erosion, or infection; a 5% 30-day postoperative morbidity rate; and a 0.05% mortality rate.
The most common long-term complication after laparoscopic adjustable gastric banding is gastric prolapse/band slippage, with band erosion or other infectious complications seen more rarely. Gastric prolapse consists of herniation of the stomach up through the band, resulting in a larger gastric pouch, malpositioning of the band, and eventual partial or complete occlusion of the band. Band erosion into the gastric lumen is a rare complication.
Patients who have laparoscopic adjustable gastric banding can expect to lose more than 50% of their extra body weight over 3 years. Longer-term studies show that weight loss with laparoscopic adjustable band is durable, with an 83% success rate for maintaining 50% loss of extra body weight for at least 5 years or more.
Comorbidity resolution is slightly lower with laparoscopic banding than with gastric bypass. Individual studies show up to 80% resolution or significant improvement of diabetes after laparoscopic adjustable gastric band. However, the meta-analysis by Buchwald and colleagues showed resolution or significant improvement of diabetes in 47.9% of patients compared with 83.7% of patients who underwent gastric bypass. O’Brien and colleagues found that patients experienced a 74% improvement or resolution of dyslipidemia, 94% resolution of obstructive sleep apnea, 55% resolution of hypertension, and 76% resolution of gastroesophageal reflux disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






