Bariatric surgery has become an increasingly important method for management of medically complicated obesity. In patients who have undergone bariatric surgery, up to 87% with type 2 diabetes mellitus develop improvement or resolution of their disease postoperatively. Bariatric surgery can reduce the number of absorbed calories through performance of either a restrictive or a malabsorptive procedure. Patients who have undergone bariatric surgery require indefinite, regular follow-up care by physicians who need to follow laboratory parameters of macronutrient as well as micronutrient malnutrition. Physicians who care for patients after bariatric surgery need to be familiar with common postoperative syndromes that result from specific nutrient deficiencies.
In the majority of patients with medically complicated obesity (commonly termed “morbid obesity”), it is difficult to effectively treat obesity by the combination of a pharmacologic agent, dietary changes, and exercise. Surgery to reduce and control weight has therefore become an important technique. After undergoing bariatric surgery, both macronutrient (such as protein) and micronutrient deficiencies are common. The type of bariatric surgery is important in understanding the potential risk of developing postoperative nutritional disorders. The rising risk of developing nutritional disorders following different types of bariatric surgery is: laparoscopic adjustable gastric banding < vertical sleeve gastrectomy < divided Roux-en-Y gastric bypass < bilio-pancreatic diversion.
In the performance of a laparoscopic adjustable gastric banding, the surgical dissection is designed to make a small pouch below the gastroesophageal junction but to keep the band above the peritoneal reflection of the lesser sac with a tunnel made through the retro-gastric attachments. The band is introduced and the tunnel aids in prevention of band migration. Band adjustment is deferred at the time of surgery and the injection reservoir is attached by tubing to the band and is implanted on the anterior rectus sheath. There are few long-term studies of the nutritional consequences of this surgery. As in any intervention that induces weight loss, vitamin D deficiency must be periodically excluded.
In the surgical construction of a restrictive vertical sleeve gastrectomy (gastric sleeve resection), multiple staplers are used to produce a tubular gastric pouch through resection of 60% to 80% of the stomach along the greater curvature. For greater weight loss, this procedure can be combined with a second malabsorptive procedure, the duodenal switch. In a duodenal switch, the duodenum is transected 5 cm distal to the pylorus and the distal duodenal segment (stump) is oversewn. The small intestine is then transected approximately one-third of its length to the ileocecal valve; the distal transected segment is used to produce an anastomosis to proximal duodenum, while the proximal transected segment is used to produce an entero-enteric anastomosis 75 to 100 cm proximal to the ileocecal valve.
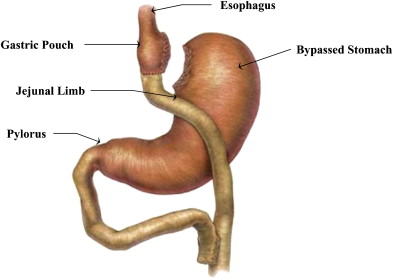
The most commonly performed bariatric surgical procedure in the United States is the divided Roux-en-Y gastric bypass ( Fig. 1 ). This procedure combines restriction of food intake, due to the small size of the gastric pouch (≤30 mL) and constriction at the gastrojejunal anastomosis (10–13 mm diameter), with malabsorption induced by bypass of the duodenum and proximal jejunum. In an extended gastric bypass, the entero-enteric anastomosis is formed 120 cm or less from the ileocecal valve. Classic studies of the Roux-en-Y reconstruction performed by Chey and colleagues demonstrated malabsorption of both fat and nitrogen. Malabsorption of fat and protein was correctable by providing exogenous pancreatic enzymes. However, these findings were not clinically significant in this group of patients (who had undergone surgical therapy for ulcer disease) because the patients were able to increase their daily caloric intake. The findings emphasize the importance in performance of the Roux-en-Y gastric bypass of restriction of food intake by combining a small gastric pouch with constriction at the gastrojejunal anastomosis.
The major feature of a bilio-pancreatic diversion in a duodenal switch or in an extended Roux-en-Y gastric bypass is that the entero-enteric anastomosis is formed 120 cm or less from the ileocecal valve to induce a significant malabsorption. The distance from the entero-enteric anastomosis to the ileocecal valve is called the “common channel.” The malabsorptive disorder induced by a short common channel (≤120 cm) is in part due to bile salt malabsorption with, consequently, secondary steathorrhea. Bilio-pancreatic diversion induces more severe deficiencies of fat-soluble vitamins as well as essential fatty acid deficiencies.
Metabolic consequences of bariatric surgery
Metabolic Syndrome
The medical management of patients who have developed metabolic syndrome is a major health care issue in the United States. The complexity of this chronic disorder leads to joint patient management by multiple medical specialists. The prevalence of metabolic syndrome has risen, and there is a direct relationship to the increase in prevalence of medically complicated obesity.
The potential for bariatric surgery to be used as a primary therapy for metabolic syndrome has been a focus in clinical studies. In a study from the Mayo Clinic of patients who underwent Roux-en-Y gastric bypass compared with patients treated with a medical management program, metabolic syndrome was defined by standard components: increased blood triglycerides, low high-density lipoprotein, hypertension, hyperglycemia, and obesity. After a mean follow-up of 3.4 years, patients treated with a medical management program had only a significant decrease in high-density lipoprotein levels, whereas patients who had undergone bariatric surgery were found to have significant declines in all components of the metabolic syndrome. With the use of a medical management program, there was only a 12% decline in the number of patients with metabolic syndrome, whereas in patients who underwent bariatric surgery there was a 66% decline. This study provides strong evidence for the superiority of Roux-en-Y gastric bypass for the long-term management of patients with the metabolic syndrome.
Regulation of Insulin Secretion
The next major question regarding the metabolic consequences of bariatric surgery is centered on the mechanisms by which bariatric surgery improves control of diabetes mellitus. Understanding these mechanisms could improve clinical decision making in the process of recommending a specific bariatric surgical procedure to an individual patient.
It has been known for many years that patients who underwent Roux-en-Y gastric bypass had major improvements in their hyperglycemia even before major weight loss had occurred. The potential role of gut endocrine peptides that alter insulin secretion by the pancreas has been considered. Incretins are insulinotrophic gut-derived hormones. Major incretins in the gut-pancreas axis include glucose-dependent insulinotrophic polypeptide (GIP), which is released from the duodenum and proximal jejunum in response to intake of glucose and fat, and glucagons-like peptide-1 (GLP-1), which is produced by posttranslational processing of preproglucagon. Endocrine cells in the gut that secrete preproglucagon are the same endocrine cells that secrete peptide YY, which the authors have shown are present in highest concentrations in the ileum and colon. Both GIP and GLP-1 affect pancreatic β-cell function.
Studies of incretin secretion after bariatric surgery support increased insulin secretion induced by nutrient-mediated secretion of incretins in patients who have undergone Roux-en-Y gastric bypass, whereas a normalization of insulin resistance has been observed after bilio-pancreatic diversion, a more malabsorptive bariatric procedure. However, a recent study did compare Roux-en-Y gastric bypass surgery with sleeve gastrectomy. This study identified increased postprandial insulin and GLP-1 levels after both bariatric surgical procedures, and both bariatric procedures had similar insulin and GLP-1 secretion after 3 months. These findings suggest that bypass of the proximal small intestine in patients who undergo Roux-en-Y gastric bypass is not the sole mechanism to explain altered secretion of incretins.
There have also been studies that compare Roux-en-Y gastric bypass with adjustable gastric banding. These studies have supported the role of increased postprandial secretion of the incretin, GLP-1, at up to 1 year after Roux-en-Y gastric bypass but not after adjustable gastric banding. Improved fasting glucose control in patients after adjustable gastric banding seems to be related to weight loss and increased insulin levels, with no apparent relationship to incretin levels.
Control of Hyperglycemia
The use of bariatric surgery for treatment of diabetes mellitus includes at least 2 major clinical issues. The first major issue is whether bariatric surgery is a first-line treatment for medically complicated obesity in those patients who have poor control of hyperglycemia. The second, which is now being examined, is whether bariatric surgery might prevent or reverse development of complications of diabetes mellitus in patients who have adequate therapy thus preventing hyperglycemia.
In studies of patients who have undergone bariatric surgery, 87% of patients with type 2 diabetes mellitus develop improvement or resolution of their disease postoperatively. The greatest weight loss and resolution of diabetes mellitus has been seen in patients who have undergone bilio-pancreatic diversion or Roux-en-Y gastric bypass, whereas after adjustable gastric banding a smaller percentage of patients have resolution of diabetes mellitus. Suggested explanations for this marked clinical improvement after Roux-en-Y gastric bypass include increased insulin secretion in the immediate postoperative period, but decreased peripheral insulin sensitivity 6 months after bariatric surgery. Other investigators have favored weight loss as being the major factor in the development of remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass although, as previously mentioned, it is a common clinical observation that patients have a significant decline in their therapy requirements for diabetes mellitus immediately after Roux-en-Y gastric bypass.
Patients can develop improved control of hyperglycemia after adjustable gastric banding, a restrictive bariatric surgical procedure. It has been reported that patients after adjustable gastric banding have reduced peripheral insulin resistance 6 months after surgery, with no changes in insulin secretion. In a separate study, 73% of patients who underwent adjustable gastric banding achieved remission of type 2 diabetes mellitus at 2 years, compared with only 13% in a separate control group of patients who were treated with conventional diabetes care with a focus on weight loss by lifestyle changes. In this study, it was suggested that remission of type 2 diabetes mellitus was related to weight loss in those patients who underwent adjustable gastric banding.
Hyperinsulinemic Hypoglycemia
A small group of patients present with complaints of dizziness, syncope, or near-syncope following Roux-en-Y gastric bypass surgery. A diagnosis of hypoglycemia must be considered, but may be difficult to identify. Recent work has supported the presence of hyperinsulinemia in response to oral glucose in Roux-en-Y gastric bypass, both in patients who are symptomatic as well as in those who are asymptomatic. This finding supports the notion that hyperinsulinemia is the result of Roux-en-Y gastric bypass.
Standard medical management has included dietary recommendations for restriction of intake of simple sugars. Patients have been instructed to carry a supplement with high simple sugar content with them for intake if a symptom develops. A select group of high-risk patients in the United States have undergone pancreatectomy with successful management of this disorder. Medical managements of this disorder with the use of diazoxide or with a combination of verapamil and acarbose have been described in case reports.
Macronutrients
Protein Deficiency
In weight reduction protocols, postoperative bariatric patients are instructed to maintain intake of 60 to 70 g of protein daily. Although it can occur after Roux-en-Y gastric bypass, significant protein malabsorption is most likely after a bilio-pancreatic diversion, in which protein malabsorption increases the risk of developing protein malnutrition.
Monitoring of patients can be difficult. It has been shown that serum albumin concentrations cannot discriminate between well and undernourished patients. In patients who present with hypoalbuminemia, it is important to consider inflammatory processes such as small intestinal bacterial overgrowth as the source. In monitoring a patient’s response to nutritional therapy, a shorter half-life protein such as prealbumin may be followed over time.
Hair loss is a common early clinical manifestation of postoperative protein malnutrition (alopecia can also occur during zinc deficiency). Long-term manifestations of protein malnutrition can include muscle mass wasting and edema; a protein deficiency similar to Kwashiorkor has been described after Roux-en-Y gastric bypass.
Macronutrients
Protein Deficiency
In weight reduction protocols, postoperative bariatric patients are instructed to maintain intake of 60 to 70 g of protein daily. Although it can occur after Roux-en-Y gastric bypass, significant protein malabsorption is most likely after a bilio-pancreatic diversion, in which protein malabsorption increases the risk of developing protein malnutrition.
Monitoring of patients can be difficult. It has been shown that serum albumin concentrations cannot discriminate between well and undernourished patients. In patients who present with hypoalbuminemia, it is important to consider inflammatory processes such as small intestinal bacterial overgrowth as the source. In monitoring a patient’s response to nutritional therapy, a shorter half-life protein such as prealbumin may be followed over time.
Hair loss is a common early clinical manifestation of postoperative protein malnutrition (alopecia can also occur during zinc deficiency). Long-term manifestations of protein malnutrition can include muscle mass wasting and edema; a protein deficiency similar to Kwashiorkor has been described after Roux-en-Y gastric bypass.
Micronutrients
Micronutrients that are essential dietary factors are those nutrients that cannot be synthesized by humans. Specific micronutrients are required in micro- or milligram quantities in a diverse array of biochemical pathways and metabolic processes. These micronutrients include water-soluble and fat-soluble vitamins, and trace elements. Vitamins are subdivided into 2 groups, fat-soluble vitamins (vitamins A, D, E, and K) and water-soluble vitamins.
A significant deficiency of an essential micronutrient can induce a clinical syndrome. One recent survey has reported an increased risk during the first 1 year after bariatric surgery of development of vitamin A, vitamin D, and thiamine deficiency. A second recent survey has reported that the prevalence 1 year after bariatric surgery of elevated homocysteine levels is 29%, low ferritin is 15%, low vitamin B12 is 11%, low red blood cell folate is 12%, and vitamin D deficiency is 57%. A twice-daily chewable multivitamin is recommended after a malabsorptive, bariatric surgery ( Box 1 ), and a once-daily chewable multivitamin is recommended after laparoscopic adjustable gastric banding or a vertical sleeve gastrectomy. Daily calcium supplements are recommended for all patients after bariatric surgery (see Box 1 ).
- 1.
MULTIVITAMIN with MINERALS: 1 chewable tablet, daily to twice a day
- 2.
CALCIUM SUPPLEMENTS: chewable tablets, 1.2 g elemental calcium, daily
Specific deficiencies
- 3.
THIAMINE: 100 mg tablet, twice daily or THIAMINE: 100–250 mg intramuscular, monthly
- 4.
NIACIN: 500 mg orally, 3 times daily
- 5.
FOLIC ACID: 1–5 mg orally, daily
- 6.
VITAMIN B12: 1000 μg, intramuscular, monthly or SUBLINGUAL VITAMIN B12: 500 μg tablet once daily
- 7.
VITAMIN A: 10,000 IU orally, daily
- 8.
VITAMIN D (ergocalciferol): 50,000 IU with a meal once weekly (up to 12 weeks) followed by VITAMIN D3 (cholecalciferol): 1000 IU with a meal twice daily
- 9.
VITAMIN E: 800–1200 IU orally, daily
- 10.
VITAMIN K: 5–20 mg orally, daily
- 11.
IRON: iron/vitamin C complex, 1 tablet daily before a meal, iron elixir (through a straw), or parenteral iron
- 12.
ZINC SULFATE: 220 mg capsule, daily to every other day
- 13.
COPPER GLUCONATE: 2 mg capsule, daily to every other day
Fat-soluble vitamins
Vitamin A
Vitamin A complex includes retinols, β-carotenes, and carotenoids. The human liver generally stores a 1-year supply of vitamin A. When ingested in high doses either acutely or chronically, vitamin A may cause toxic manifestations, including headache, vomiting, diplopia, alopecia, dryness of the mucous membranes, bone abnormalities, and liver damage. Signs of toxicity usually appear with sustained daily intakes exceeding 15,000 IU. As an alternative supplement, signs of toxicity have not been observed while receiving β-carotene, the pre-vitamin A analogue.
Vitamin A deficiency after bariatric surgery is most commonly seen in patients who have undergone a bilio-pancreatic diversion, duodenal switch, or extended Roux-en-Y gastric bypass. In these procedures, the mechanism of deficiency is most likely related to fat-soluble vitamin malabsorption induced by bile acid deficiency. In addition, individuals with zinc deficiency have impaired protein synthesis that may alter retinol transport from the liver to other organs. Common manifestations of vitamin A deficiency include nocturnal visual difficulty, dry skin, dry hair, and pruritus. Other potential manifestations include decreased visual acuity and reduced resistance to infections. Treatment of vitamin A deficiency includes supplemental vitamin A, 10,000 IU daily by mouth (see Box 1 ) as well as cotherapy for any existing iron deficiency, because vitamin A deficiency may persist in the presence of iron deficiency.
Vitamin D
It is important to simultaneously consider the potential for vitamin D deficiency and calcium malabsorption because vitamin D deficiency activates a metabolic cascade resulting in hypocalcemia, secondary hyperparathyroidism, and subsequently osteoporosis and osteomalacia. Isolated serum calcium measurement is not an adequate marker of calcium metabolism. Patients may present clinically with complaints of bony pain, back pain, or aching of the limbs.
Multiple explanations have been proposed for vitamin D deficiency. First, it has been reported that a large percentage of patients with medically complicated obesity have vitamin D deficiency. In addition, vitamin D malabsorption results from bile salt deficiency, especially in those patients who have undergone a bilio-pancreatic diversion during bariatric surgery. Patients who have a rapid weight loss phase from any cause require additional vitamin D. Finally, preliminary studies suggest that small intestinal bacterial overgrowth interferes with vitamin D absorption.
In preliminary studies, bariatric surgery patients maintain normal serum calcium by decreasing urinary calcium secretion. Urine calcium secretion can, however, be altered by concomitant use of diuretics. It is therefore important to monitor total 25-hydroxyvitamin D levels, 24-hour urinary calcium, and serum alkaline phosphatase at least every 6 months postoperatively. Parathyroid hormone determination and dual energy x-ray absorptiometry scan should be considered in patients who have prolonged or difficult to treat vitamin D deficiency and elevation of the bone fraction of serum alkaline phosphatase. A patient with an elevation of the parathyroid hormone level requires additional supplementation with vitamin D and calcium.
It is recommended that all patients after bariatric surgery use daily supplements to include at least 1.2 g daily of elemental calcium and 800 international units of vitamin D (see Box 1 ). Patients with low serum levels of 25-hydroxyvitamin D are treated initially with 50,000 IU of vitamin D (ergocalciferol) orally once per week for 6 to 8 weeks (see Box 1 ). A recheck of 25-hydroxyvitamin D level after 8 weeks is recommended to confirm repletion. The reported dose for treatment of rickets is at least 600,000 IU. Treatment of up to 150,000 IU taken 4 times, during 1 day of treatment has been described, although the authors generally provide 50,000 IU taken daily with a meal for 12 days, because of anecdotal reports of liver test abnormalities associated with high-dose oral vitamin D.
Vitamin E
Vitamin E consists of tocopherols and tocotrienols. This fat-soluble vitamin, once absorbed, is located in cell membranes where it is thought to be active in preventing lipid peroxidation. Most adults seem to tolerate doses of vitamin E alone up to 1000 mg per day (0.67 mg of vitamin E is 1 IU) without gross signs or biochemical evidence of toxicity.
Deficiency of vitamin E should be considered in individuals who have visual symptoms (retinopathy), nonspecific neurologic symptoms (ataxia, loss of vibration and position sensation, muscle weakness, or ptosis), or hemolytic anemia. Treatment of vitamin E deficiency should include oral vitamin E 800 to 1200 IU daily (see Box 1 ).
Vitamin K
Vitamin K is the name given to a group of compounds, all of which contain the 2-methyl-1,4-naphthoquinone moiety. These compounds are essential for the formation of prothrombin, and 5 factors (factors VII, IX, and X, and proteins C and S) that are involved in regulation of blood clotting. Under normal conditions, vitamin K is moderately (40%–70%) well absorbed from the jejunum and ileum, but very poorly absorbed in the colon.
Absorption of vitamin K and other lipid-soluble vitamins depends on the normal flow of bile and pancreatic secretion, and is enhanced by dietary fat. The total body pool of vitamin K is small and its turnover is rapid. Most of the daily requirements for vitamin K is provided through its biosynthesis by the intestinal flora. Deficiency of vitamin K leads to increase risk of bleeding disorders. Replacement of vitamin K can be obtained either with an oral form (5–20 mg daily) (see Box 1 ) or with parenteral delivery of the vitamin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






