Fig. 6.1
A young asymptomatic man with giant cavernous hemangioma. On unenhanced CT scan, (a) the lesion is hypodense with well-defined lobulated margins. This large tumor shows a central non-enhanced area corresponding to the cystic cavity, probably necrotic (arrow). During the arterial phase, (b) there is a hyperdense peripheral nodular enhancement that progresses centrally during the portal and equilibrium phases (arrowhead, c, d). Axial and MPR coronal images (e, f) are useful to quantify the exact extension of the tumor. Due to the posterior location of the hemangioma (protected from abdominal trauma), no surgical resection was proposed
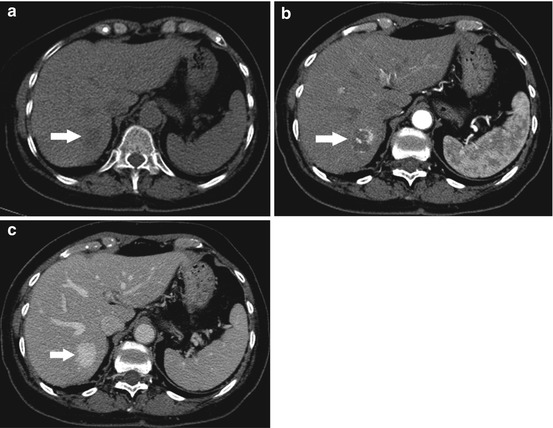
Fig. 6.2
A typical cavernous hemangioma incidentally discovered in a middle-aged man. On unenhanced CT scan, (a) the oval-shaped lesion (arrow) is homogeneously hypodense with well-define margins. In the dynamic study, this benign tumor presents the typical peripheral globular enhancement in the arterial phase (arrow, b) and gets completely filled in with the contrast media in the portal-venous phase (arrow, c). The patient underwent US follow-up
At ultrasound, hemangiomas are usually shown as well-defined, oval-shaped homogeneous hyperechoic lesions with or without posterior acoustic enhancement, even though these features are not always found together [3, 4]. Furthermore, different variations of the usual images are seen in large lesions because of thrombosis, fibrosis, hemorrhage, or calcifications, resulting in a heterogeneous or sometimes hypoechoic appearance that may require further investigation with MR or CT [4]. Power/color Doppler US is not so useful because of the extremely low flow velocities and the small size of vascular structures inside hemangiomas [3], while CEUS may show the typical peripheral nodular contrast medium enhancement and the iris-diaphragm phenomenon [5].
At MRI, the high blood/water content gives the hemangiomas a typical hypointense appearance on T1w sequences and a marked hyperintensity on T2w sequences. DCE-MRI usually shows a slow perfusion pattern with early peripheral globular enhancement that proceeds centripetally. Indeed small hemangiomas may completely and homogeneously enhance in the early arterial phase, while large hemangiomas are progressively filled in with gadolinium, leading to a persistent homogeneous hyperintensity in the delayed phase. Fibrotic or thrombotic components and calcifications inside the hemangioma result as hypointense areas on T2w images, also confirmed by focal intratumor hypointensity on post-gadolinium T1w sequences [6].
On CT, hemangiomas are sharply defined masses that are usually hypoattenuating compared with the adjacent hepatic parenchyma, if normal (i.e., nonsteatotic), on unenhanced images [7]. On unenhanced images, the vascular components of hemangiomas have the same attenuation value as the blood within blood vessels; intratumor thrombosis or fibrosis is hypoattenuating while calcium is hyperattenuating. The enhancement pattern is the same seen at MRI; the identification of globular enhancement that is isodense to the aorta is characteristic of hemangiomas [8].
Concerning follow-up of benign liver tumors we couldn’t find consensus guidelines in the literature. However we completely agree with the recently published guidelines suggested by the American College of Gastroenterology [9]. According to these guidelines follow-up imaging is not required in classical asymptomatic hemangioma. On the other hand, rapid growth of a hemangioma has been reported, justifying radiologic follow-up of patients with large lesions, particularly those in a subcapsular location.
6.1.2 Simple Hepatic Cyst
Simple cyst s are (Fig. 6.3) congenital lesions affecting 2–7 % of the population. They can be single or multiple and consist of usually small-sized (10 mm) serous contents lined by cuboidal, biliary-type epithelium with no communication with the bile ducts. Simple cysts tend to occur more frequently in the right hepatic lobe and are more prevalent in women; also complex cysts are more frequent in women [4]. Adult-onset cysts may be classified as nonparasitic, parasitic (echinococcus), or hemorrhagic (spontaneous/post-traumatic). Multiple hepatic cysts should be differentiated from autosomal dominant polycystic liver disease (APCKD) and von Hippel-Lindau syndrome [2]. Most patients are asymptomatic and the diagnosis is incidental.
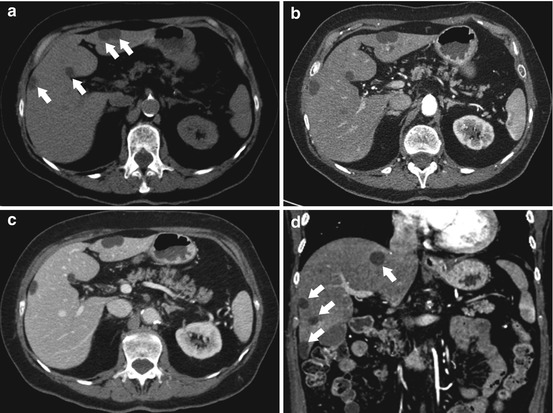
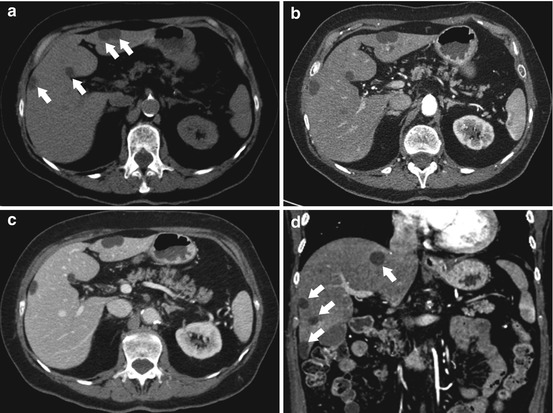
Fig. 6.3
Multiple simple hepatic cysts. The lesions were incidentally discovered during a CT angiogram in a middle-aged woman with abdominal angina due to mesenteric ischemia. They are located both at the right and left lobes (arrows) and present fluid density both on pre-contrast CT (a) and on contrast-enhanced CT (b, arterial phase; c, portal-venous phase; d, coronal arterial phase) with no significant enhancement of the walls; no evident septations or calcifications are seen, confirming the benign nature of these very common lesions
Simple cysts should be differentiated from unilocular biliary cystadenoma , as this entity has premalignant potential, and cystic metastases [8]. Features that suggest malignancy include internal mural nodules, coarse calcifications, and irregularities in the wall [10]; moreover cystadenomas are usually multilocular [1]. Ciliated hepatic foregut cyst s are located along the convex external surface of the liver, bulge the liver contour, and are usually intersegmental in location. Foregut cysts usually possess a definable enhancing wall [2].
At ultrasound hepatic cysts appear as anechoic fluid-filled spaces without clear walls and with posterior acoustic enhancement [4].
Features of cysts at MRI include T2 hyperintensity with uniform smooth round, ovoid, or slightly lobulated margins and low signal on T1w sequences with no enhancement on early and late post-gadolinium images. Variations in the appearance of cysts occur and include septations, lobulation, and elevated T1 signal due to protein or blood products, sometimes with a fluid-fluid level. Fluid-containing lesions such as cysts and hemangiomas can be easily detected and distinguished from solid benign and malignant lesions using DWI; however, this differential diagnosis can be performed also with conventional MRI [8].
On CT hepatic cysts appear as homogeneous and hypoattenuating (water density <20 HU) lesions on basal scan, with no enhancement of their walls or content after intravenous administration of contrast material. They have typically well-defined borders without perceptible walls [8].
6.1.3 Biliary Cystadenoma
Cystadenoma is the most commonly encountered primary cystic neoplasms of the liver, usually found incidentally on abdominal imaging. Cystadenomas can be differentiated from simple cysts based on the appearance at US or recurrence after surgery. At US they appear as hypoechoic lesions with irregular walls, septations, and coarse calcifications, features not present in simple cysts [8]. On CT and at MRI, cystadenomas may present some contrast enhancement of the wall or septations [1, 10]. As cystadenoma may potentially have a malignant degeneration evolving to cystadenocarcinoma, it is typically surgically resected requiring liver resection (indeed, when treated through unroofing like simple cysts, recurrence rates are high); imaging is not able to differentiate benign from malignant lesions, and biopsy is usually not indicated since unreliable [8]. Hepatic cystadenomas should be differentiated from cystic metastases, large simple or complicated hepatic cysts, complex abscesses, echinococcal cysts, and intrahepatic bilomas or hematomas.
6.1.4 Angiomyolipoma
Angiomyolipoma is a rare benign, unencapsulated mesenchymal tumor that is composed of varying proportions of three elements: smooth muscle cells, thick-walled blood vessels, and mature adipose tissue [1]. US, CT, and MRI typically demonstrate the fat component and prominent central vessels. At US, angiomyolipoma may be highly echogenic and indistinguishable from a hemangioma, unless it presents sound attenuation, speed propagation artifacts, or refraction artifacts [11]. On CT it has been reported to consist of two parts: a peripheral angiomyomatous component with soft tissue attenuation and a fatty hypoattenuating component [11]. MRI characteristics vary depending on the proportion of intratumoral fat: frequently, angiomyolipoma has a high fat content, with high signal intensity on T1-weighted images and a significant drop in signal intensity on fat-suppressed images, while areas of microscopic fat infiltration demonstrate diffuse loss of signal on out-of-phase sequences [6, 11]. On T2-weighted sequences, hepatic angiomyolipoma is homogeneously or heterogeneously hyperintense [1]. On contrast-enhanced CT and MR studies, it usually demonstrates early intense contrast enhancement that peaks later than that of a hepatocellular carcinoma [11, 12].
6.2 Hepatocellular Lesions
6.2.1 Focal Nodular Hyperplasia (FNH)
Focal nodular hyperplasia (FNH) is the second most common benign hepatic lesion following hemangioma; it is typical in young females, usually asymptomatic [13]. FNH (Figs. 6.4 and 6.5) consists of unencapsulated hepatocyte nodules circumscribed by fibrous septa (containing mononuclear inflammatory cells) that coalesce into a central or eccentric vascular structure resembling a stellate scar [1]; however, a central scar may not be visualized in up to 50 % of cases, particularly in lesions less than 3 cm in diameter [1, 14]. Approximately 20 % are multiple and association with cavernous hemangiomas is frequent [1]. Bile ductules are present at the junction of the fibrous septa and hepatocytes; however, they do not connect to the intrahepatic bile ducts [1]. Hemorrhage is very uncommon and malignant degeneration is not reported [15].
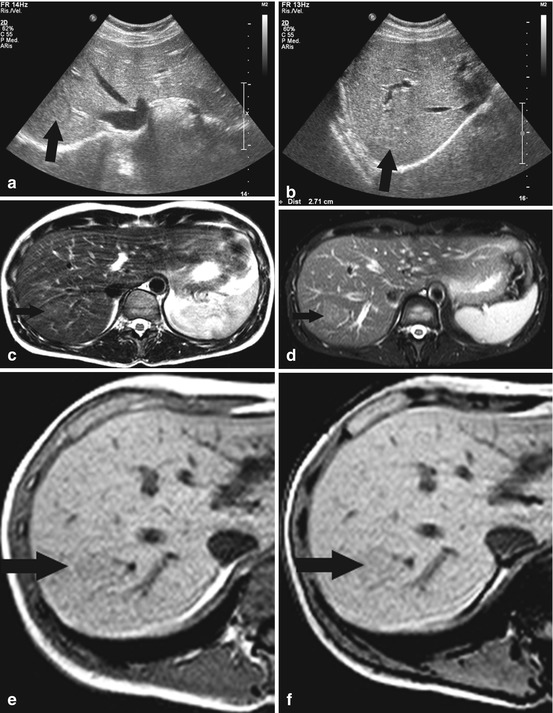
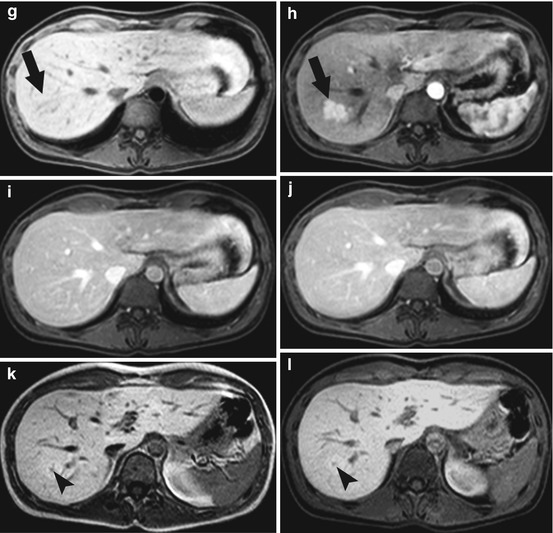
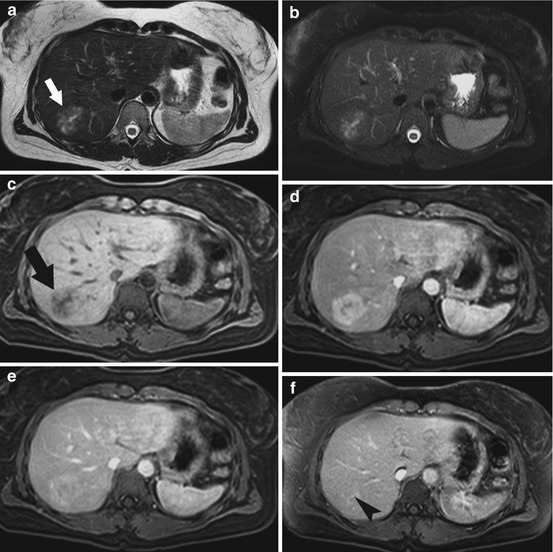
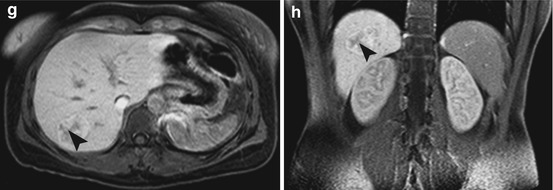
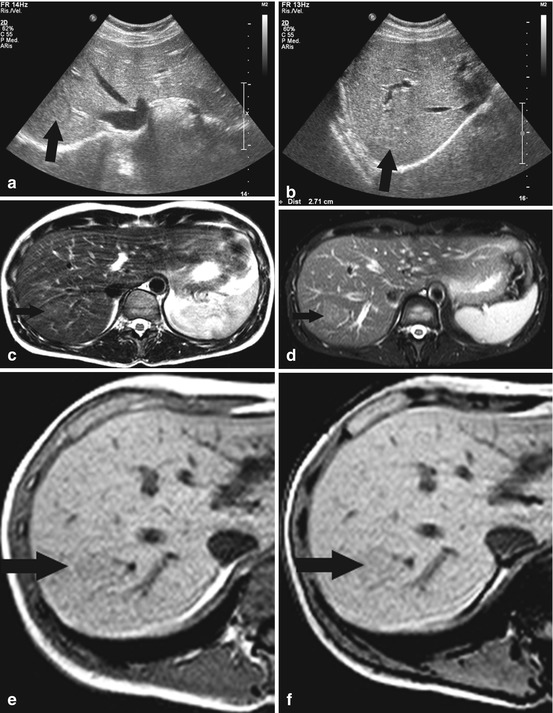
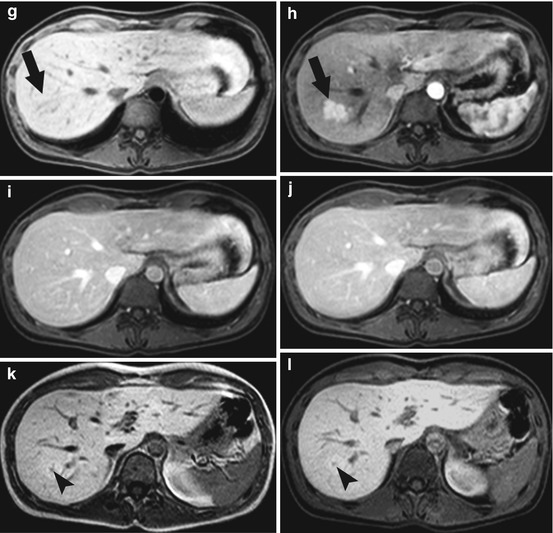
Fig. 6.4
A young woman with asymptomatic focal nodular hyperplasia. The lesion was incidentally detected at US (arrows, a, b) where it appears as a well-defined isoechoic nodule surrounded by a hypoechoic halo, probably representing the compressed surrounding hepatic parenchyma. To better characterize the nodule, the patient underwent CE-MRI with hepatocyte-specific contrast agent (Gd-BOPTA). Unenhanced axial T2-weighted and STIR images (c, d) reveal a slightly hyperintense liver lesion in the right liver lobe (arrow); the tumor is slightly hypointense on T1-weighted images (arrow, e) with no significant dropout of the MR signal on “opposite-phase” acquisitions (arrow, f). An intense and homogeneous enhancement is seen during the arterial phase (arrow, g, basal; arrow, h, arterial) after contrast administration, with no significant washout in the portal-venous and equilibrium phases. In these phases, the tumor returns isointense to the surrounding gradually enhancing parenchyma (i, j). Late hepatobiliary T1-weighted images (k), also acquired with fat saturation technique (l), confirm the benign nature of the lesion, composed of functioning hepatocytes that uptake and normally dismiss the hepatocyte-specific contrast agent. In this case, the typical central scar is just detectable as a hypointense component in the hepatobiliary phase imaging (arrowhead). Contrast-enhanced MR provided solid criteria for the diagnosis of FNH and neither biopsy nor surgical resection was indicated; this patient underwent just a periodical US follow-up
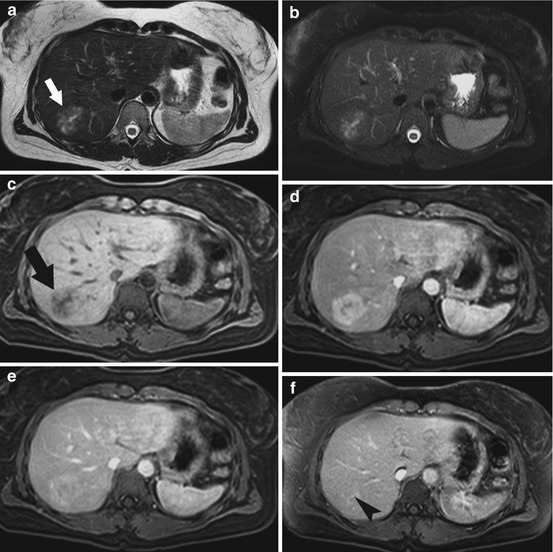
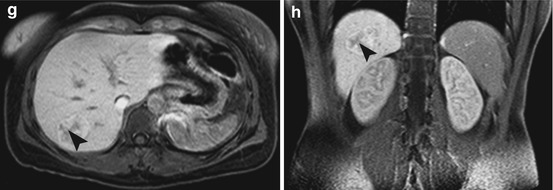
Fig. 6.5




A typical FNH with prominent central scar in a young woman. The incidentally discovered mass is slightly hyperintense on T2-weighted imaging with and without fat signal suppression (white arrow, a, b) with a more hyperintense star-shaped central scar. On the dynamic study with a hepatocyte-specific contrast agent, the (black arrow in the basal T1w image, c) tumor presents avid enhancement (d) that homogenizes to that of the normal liver in the portal-venous phase (e). The scar, initially hypointense on T1-weighted images with fat suppression (c), gets progressively filled in with the contrast agent and becomes hyperintense (arrowhead, f) about 5 min after its administration, probably due to the slow accumulation of gadolinium in the hypovascular interstitium. On the hepatobiliary phase, (g, h) the lesion results heterogeneously hyperintense with a hypointense central scar (arrowhead). The woman underwent periodic US surveillance
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






