■ Anal fissures seen in Crohn’s disease and tuberculosis are frequently painless.
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Diagnosis is made by visual inspection. Unless findings suggest a specific cause or the appearance and/or location is unusual, further studies are not required.
■ In selected cases, flexible sigmoidoscopy or colonoscopy may be indicated.
SURGICAL MANAGEMENT
■ The majority of anal fissures will resolve with medical management and will not require surgery.
■ Medical management includes the following:
■ Aggressive prevention of constipation
■ Increase fiber and decrease fat in the diet
■ Fiber supplementation
■ Increase water intake
■ Use of moist pads (flushable baby wipes) for wiping and anal hygiene
■ Avoiding straining or prolonged sitting on the toilet
■ Soaking in a warm bath (also called a sitz bath), 10 to 20 minutes several times a day, to promote the relaxation of the anal muscles
■ These conservative measures lead to healing of the anal fissure in a few weeks to a few months in 80% to 90% of patients. However, when these conservative measures alone are not successful, pharmacologic intervention can also be instituted. This includes the following:
■ Topical nitrates ointment: Examples include nitroglycerin ointment 0.4% (Rectiv) and glyceryl trinitrate ointment (Rectogesic). Although effective, they are dose dependent. Disabling headaches are common at higher doses, making patient compliance with the treatment unreliable.
■ Topical calcium channel blockers, including nifedipine or diltiazem ointment, are as effective as nitrate ointments but with significantly less side effects. Examples include topical nifedipine 0.3% with lidocaine 1.5% ointment and diltiazem 2% ointment.
■ Combination of medical therapies may offer up to 98% cure rates.
■ A combined surgical and pharmacologic treatment, administered by colorectal surgeons, is periodic direct injection of botulinum toxin (Botox) into the anal sphincter to relax it. Oftentimes, these injections prove less and less potent with each application. With patients spending thousands of dollars and not achieving a permanent cure, they oftentimes elect to have surgery.
■ When conservative medical therapy fails, surgery is considered.
Preoperative Planning
■ Mechanical bowel preparation is not necessary.
■ Fleet enemas are prescribed for the night before and the morning of surgery to clear the rectal vault.
■ Intravenous cefoxitin is administered within 1 hour of skin incision.
■ A preoperative time-out and briefing is conducted with the entire surgical team in attendance.
■ An anal block with bupivacaine extended-release liposome injection is associated with both pain relief for 72 hours and a 45% reduction in total opioid consumption at 72 hours.
Positioning
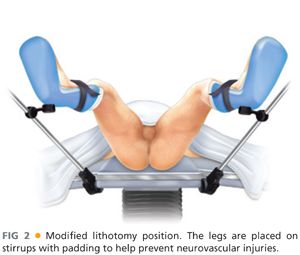
■ The patient is placed supine on a modified lithotomy position with the legs on padded stirrups to prevent neurovascular injuries to the calves (FIG 2).
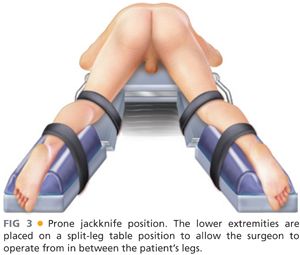
■ Alternatively, the patient can be placed in a prone jackknife position on a split-leg table, with the surgeon positioned between the legs (FIG 3). The buttocks are spread apart with tape.
■ The author prefers to perform these procedures under general anesthesia.
■ Using headlights is critical for good visualization.
TECHNIQUES
CLOSED LATERAL INTERNAL SPHINCTEROTOMY (TRANSCUTANEOUS)
■ Using lubrication, perform a gentle anal dilation with two fingers.
■ An anoscope is used to confirm the presence of the anal fissure.
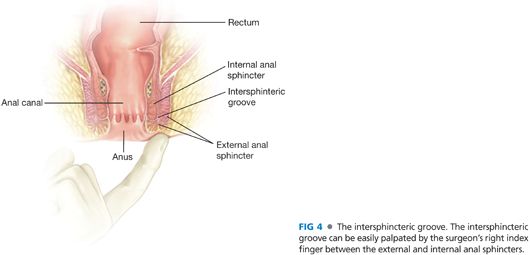
■ With the patient on a modified lithotomy position and palpating with the tip of your right index finger, identify the anal intersphincteric groove (FIG 4). The intersphincteric groove is a distinct groove in the anal canal, forming the lower border of the pecten analis, marking the change between the subcutaneous part of the external anal sphincter and the border of the internal anal sphincter.
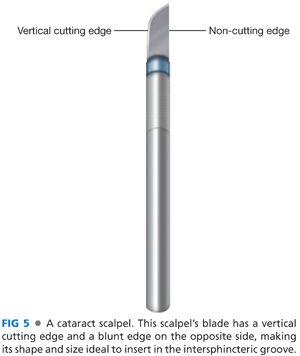
■ For the closed internal lateral sphincterotomy, the author prefers to use a cataract scalpel due to the vertical plane of the cutting edge of the blade (FIG 5), as opposed to the oblique plane of the cutting edge of a no. 11 blade. This makes it easier to cut the internal sphincter more evenly as the scalpel is withdrawn from the intersphincteric groove.
■ Place your left index finger in the anal canal. In cases of HIV or hepatitis B/C infection, insert an anal speculum instead of inserting your own finger as a precaution to avoid potential transmission of communicable disease in case of inadvertent injury to your index finger during the sphincterotomy.
■ Using a no. 11 blade scalpel on your right hand, create a small opening on the skin overlying the intersphincteric groove on the patient’s left lateral side. Performing the closed lateral internal sphincterotomy on the anal canal’s left lateral side is easier for a right-handed surgeon to perform (scalpel in your dominant hand).
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








