Suprapubic Hernia
John T. Paige
The term “suprapubic” hernia was first defined by el Mairy and refers to an abdominal wall defect arising within 4 cm of the symphysis pubis. Also known as “parapubic” hernias, the repair of suprapubic hernias are a technical challenge due to their close proximity to bone, nerves, and blood vessels in the pelvis. Suprapubic hernias are a subset of incisional hernias, often developing after gynecologic, urologic, and general surgical procedures in which division of the lower abdominal wall fascia near the symphysis pubis is required for adequate exposure. Fortunately, they are relatively infrequent. The incisional hernia rate in patients undergoing a low transverse Pfannenstiel incision only ranges from 0.04% to 2.1%. Even among centers specializing in the laparoscopic repair of suprapubic hernias, their rates range from 11.6% to 32.8% of the total number of incisional hernias encountered. Such facts, however, emphasize the difficulty in treating enough of these hernias to develop expertise in their repair.
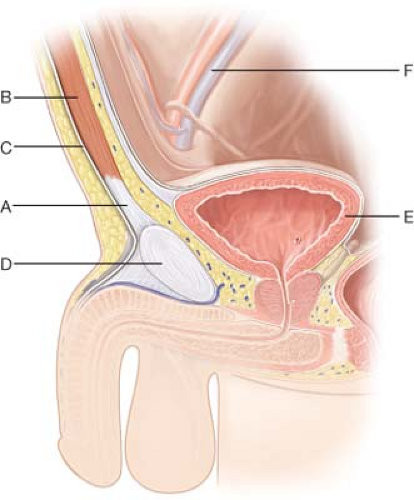
Suprapubic hernias develop as a result of disruption of the musculotendinous insertion of the abdominal oblique aponeurosis, rectus abdominis musculature, and rectus sheath into the symphysis pubis (Figs. 34.1 and 34.2). Typically, these defects form secondary to inadequate purchase of tissue during closure of a low midline incision near the symphysis pubis. The resultant midline deformity can then extend laterally along the pubis. Thus, repair is indicated in the presence of a defect, especially if the patient is symptomatic (see Preoperative Planning).
Minimally invasive repair is the preferred therapy for suprapubic hernias. First described by Hirasa et al. in 2001, it has been refined over the decade. Contraindications to suprapubic hernia, therefore, are the same as those for any laparoscopic incisional hernia. Severe chronic obstructive pulmonary disease, uncorrectable bleeding dyscrasia or coagulopathy, and frozen abdomen are some examples of conditions that might preclude a successful laparoscopic approach.
The first step in preoperative planning is to obtain a thorough history and physical examination. Patients presenting with suprapubic hernias can complain of symptoms similar to those found in the presence of inguinal hernias. Pain, heaviness, or a dragging sensation may be present in the suprapubic region with or without abdominal wall
bulging. An antecedent history of prior lower abdominal surgery is invariably present and can be confirmed on physical examination by the presence of low midline, Pfannenstiel, Maylard, or Cherney incisions (Tables 34.1 and 34.2). Often, patients have had multiple abdominopelvic procedures, and, hence, a careful determination of prior operations is essential. Additionally, review of operative notes related to prior incisional hernia repairs is recommended in order to determine the presence, location, and type of any mesh used. Review of co-morbid conditions, especially those that might preclude a minimally invasive approach (see Indications/Contraindications), is also important.
bulging. An antecedent history of prior lower abdominal surgery is invariably present and can be confirmed on physical examination by the presence of low midline, Pfannenstiel, Maylard, or Cherney incisions (Tables 34.1 and 34.2). Often, patients have had multiple abdominopelvic procedures, and, hence, a careful determination of prior operations is essential. Additionally, review of operative notes related to prior incisional hernia repairs is recommended in order to determine the presence, location, and type of any mesh used. Review of co-morbid conditions, especially those that might preclude a minimally invasive approach (see Indications/Contraindications), is also important.
Physical examination should emphasize delineation of the size, extent, and borders of the hernia defect. In certain patients, such as those who are obese, such determination can be a challenge. Computed tomography (CT) of the abdomen and pelvis is useful in such circumstances, since it can give information related to the relation of the inferior edge of the hernia to the symphysis pubis. Additionally, it can lend insight into hernia size and its exact contents. CT is also recommended in patients who have mesh present from a prior incisional hernia repair, since it helps identify its location in
relation to the current defect. Ultrasonography has been employed as well to help determine the size of suprapubic defects. Finally, appropriate preoperative laboratory analysis and medical/cardiac clearance is undertaken based on patient condition, risk factors, and co-morbidities.
relation to the current defect. Ultrasonography has been employed as well to help determine the size of suprapubic defects. Finally, appropriate preoperative laboratory analysis and medical/cardiac clearance is undertaken based on patient condition, risk factors, and co-morbidities.
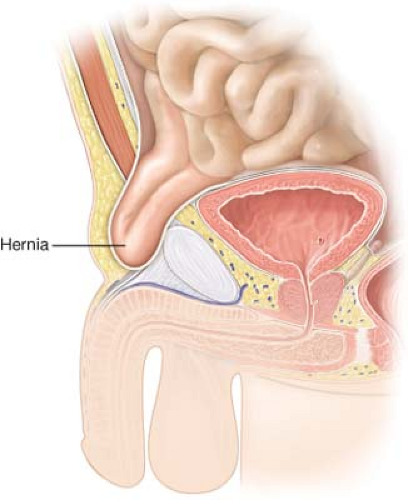 Figure 34.2 Pathophysiology. With disruption of the musculotendinous insertion of the lower abdominal wall muscles near the symphysis pubis, herniation of intraabdominal and pelvic contents occurs. |
Table 34.1 Type of Previous Surgery in Patients Presenting with Suprapubic Hernia | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Although open tension-free repair using mesh coverage has been described, current therapy for suprapubic hernias involve a minimally invasive approach similar to that used for other anterior abdominal wall incisional hernia repairs. This approach is based on the principles of the open retro-rectus tension-free repairs using wide mesh coverage developed by both Rives and Stoppa. Key components include adequate circumferential dissection of the hernia defect with proper underlay mesh placement and fixation to ensure a 4 to 5 cm overlap of the hernia defect in all directions. A step-by-step description of the laparoscopic technique follows.
Patient Positioning and Preparation
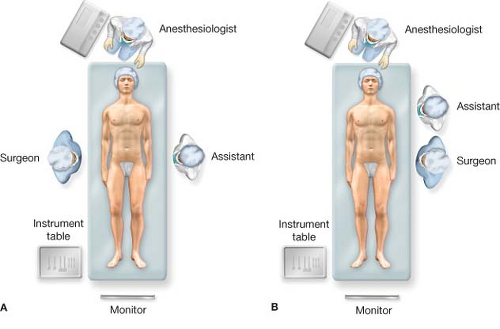
The patient is placed in the supine position on the operative table (Fig. 34.3). Sequential compression devices are placed on the bilateral lower extremities. Following induction of general anesthesia and secure placement of an endotracheal tube, an orogastric tube is placed. In addition, a triple lumen Foley catheter is inserted into the bladder to assist with dissection in the suprapubic region (see Dissection). Both arms are tucked and padded unless precluded by the patient’s body habitus. In obese patients, additional padding is required to elevate the tucked arm to avoid traction on the brachial plexus. Monitors are positioned at the foot of the bed. Often, a single one is sufficient. With arms tucked, the assistant can position him/herself opposite or alongside the surgeon for the procedure. On the basis of port placement, the surgeon can position him/herself on either side of the operating room table (see Port Placement). The pubis hair is clipped to assist with access to this region, and surgical preparation is undertaken from the nipples to the mid-thighs and lateral to the table on both sides using chlorhexidine except for the genitalia for which a betadine scrub is used. An iodine-impregnated drape can also be applied to the abdomen for added antimicrobial effect. Prophylactic antibiotics are administered prior to incision.
Access
Abdominal access is typically obtained above the umbilicus in a location away from prior incisions. A Veress needle is placed in the left hypochondrium. with creation
of pneumoperitoneum after verification of its location with syringe aspiration and gravity testing using a column of saline. Pneumoperitoneum is established to approximately 15 mm Hg pressure. Next, a 5 or 12 mm bladeless trocar is introduced into the abdominal cavity using a zero-degree laparoscope for direct visualization. Alternatively, the abdomen can be entered via an open cutdown technique with direct placement of a 10 or 12 mm trocar. It should be placed away from prior incision sites if possible.
of pneumoperitoneum after verification of its location with syringe aspiration and gravity testing using a column of saline. Pneumoperitoneum is established to approximately 15 mm Hg pressure. Next, a 5 or 12 mm bladeless trocar is introduced into the abdominal cavity using a zero-degree laparoscope for direct visualization. Alternatively, the abdomen can be entered via an open cutdown technique with direct placement of a 10 or 12 mm trocar. It should be placed away from prior incision sites if possible.
Table 34.2 Scar Location in Patients Presenting with Suprapubic Hernia | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|