FINNEY STRICTUREPLASTY
■ For strictures 10 to 25 cm in length, a Heineke-Mikulicz strictureplasty creates excessive tension, so the Finney strictureplasty is preferred. A Finney strictureplasty should not be performed in a strictured segment that is longer than 25 cm, however, because this may risk a blind loop syndrome.
■ The strictured area of bowel is isolated as previously described and the bowel is placed in a U shape with the midpoint of the stricture as the apex in order to simulate the finished strictureplasty and guide the bowel incision.
■ The bowel is incised on the antimesenteric border beginning in normal bowel 2 to 3 cm from the stricture. This incision is then carried through the stricture using electrocautery. As the incision reaches the apex of the U shape, it should take a gradual course toward the mesenteric border as this allows for better tissue apposition. The incision finishes in 2 to 3 cm of normal bowel after having been brought back to the antimesenteric border.
■ Interrupted, full-thickness 3-0 polyglactin sutures are used as marking sutures to approximate normal bowel edges at the base of the strictureplasty and are also used to fix the diseased bowel at the apex. Continuous 3-0 polyglactin suture is then used to close the posterior wall followed by the anterior wall of the strictureplasty. Interrupted sutures may also be used to reinforce the continuous suture at various points and maintain tissue apposition4 (FIG 2).

SIDE-TO-SIDE ISOPERISTALTIC STRICTUREPLASTY
■ For extensive stricturing Crohn’s disease not amenable to strictureplasty of isolated segments, the side-to-side isoperistaltic strictureplasty can be performed.
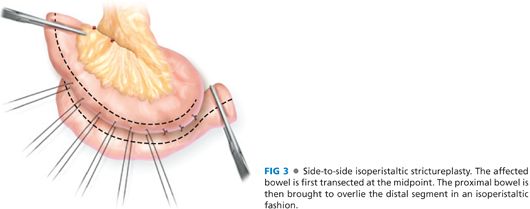
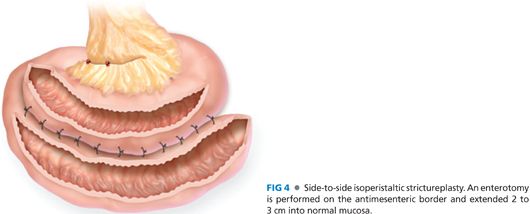
■ The affected bowel is first transected at the midpoint. The proximal bowel is then brought to overlie the distal segment in an isoperistaltic fashion (FIG 3). An enterotomy is performed on the antimesenteric border and extended 2 to 3 cm into normal mucosa (FIG 4).
■ The transected ends of bowel are spatulated in order to avoid creation of blind stumps.
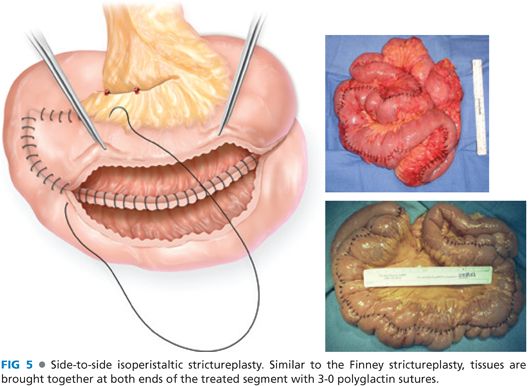
■ Similar to the Finney strictureplasty, tissues are brought together at both ends of the treated segment with interrupted 3-0 polyglactin sutures. The posterior layer is closed with a running 3-0 polyglactin suture followed by closure of the anterior layer (FIG 5).
SMALL BOWEL BYPASS
Gastrojejunal Bypass
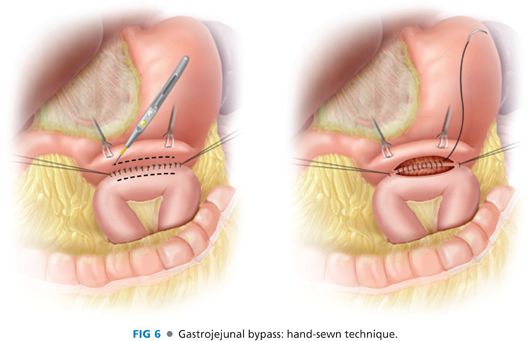
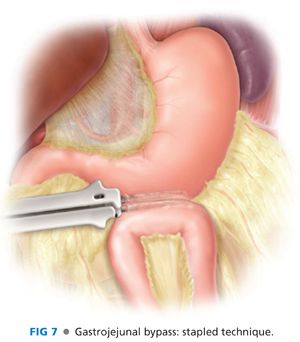
■ Gastrojejunostomy is performed by bringing the most proximal loop of jejunum that easily reaches the greater curvature of the stomach. The anastomosis can be done using either a hand-sewn (FIG 6) or stapled technique (FIG 7). It can also be done antecolic or retrocolic. The antecolic approach avoids dissection through the transverse colon mesentery and also keeps the anastomosis away from the retroperitoneum.
Duodenojejunal Bypass
■ A longitudinal enterotomy in the proximal jejunum is made in an area that is free of disease. A Foley catheter is inserted and passed proximally through the duodenal sweep and filled with varying amounts of water to assess for duodenal stricture. If there is a stricture isolated to the third and fourth portions of the duodenum and it is determined that there is healthy, patent bowel in the first and second portion, then a bypass may be performed. A longitudinal duodenotomy is performed in the healthy portion of the duodenum. 3-0 polyglactin sutures are placed to approximate the jejunal enterotomy to the duodenotomy.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








