Spigelian Hernia
Eric G. Sheu
Douglas S. Smink
David C. Brooks
Spigelian hernias are rare abdominal wall hernias. Approximately, 1,000 cases have been reported in the literature, and their incidence is estimated to be <2% of all abdominal wall hernias. The hernia is named after Adriaan van der Spieghel, the Belgian anatomist who first described the semilunar line in 1645. It was, however, a Flemish anatomist Josef Klinkosch who identified the hernia in 1764 as a defect in the semilunar line and named it after van der Spieghel.
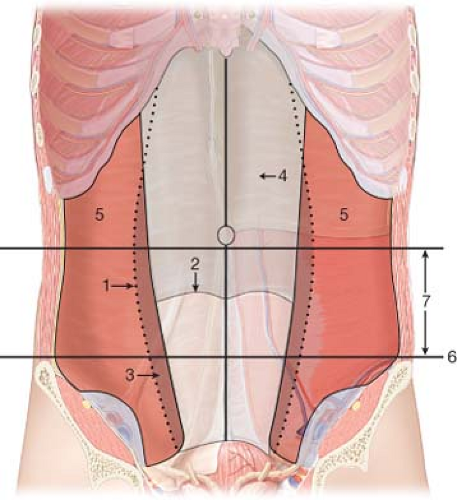
These hernias occur through the spigelian aponeurosis, which is composed of the aponeurosis of the transverse abdominal muscle that lies between the lateral edge of the rectus muscle and the linea semilunaris (Fig. 35.1). The spigelian aponeurosis extends both above and below the arcuate line of Douglas. However, the vast majority of spigelian hernias occur within the 6 cm segments of the aponeurosis that lie immediately cranial to the anterior superior iliac spine. In this so-called “spigelian belt,” the lack of a posterior rectus sheath and the parallel orientation of the transversus and internal oblique aponeuroses predisposes the spigelian aponeurosis to the development of a hernia.
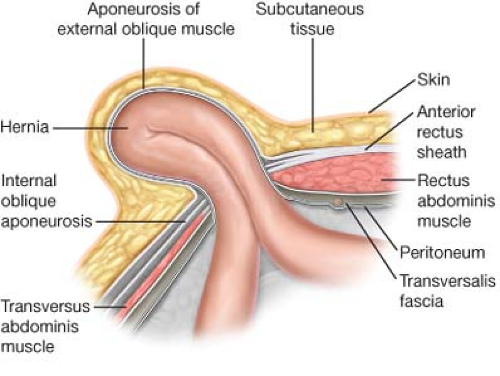
The external oblique fascia is often intact over the hernia, so that on physical examination, an abdominal wall bulge or defect can often not be detected (Fig. 35.2). Because of the difficulty of physical examination, patients presenting with symptomatic hernias are often misdiagnosed—for example, symptoms of a left-sided spigelian hernia can be mistaken for diverticulitis. Ultrasound can identify the defect in the semilunar line or the hernia sac itself. CT is the current gold standard of imaging diagnosis and can characterize the hernia defect and contents (Fig. 35.3). However, CT is not a 100% sensitive—six false negative CT scans (out of 19) were reported in a case series using older generation CT scanners. It is generally felt that modern high resolution CT scanners have higher sensitivity, but no published data on the topic exists.
A high proportion of patients with spigelian hernias will present with incarceration. Given this fact, all diagnosed spigelian hernias should undergo operative repair. Contraindications are identical to those for any intraabdominal operation and are not specific to spigelian hernia repair: For example, recent MI, severe coagulopathy, and other medical co-morbidities prohibiting a general anesthetic.
Preoperative evaluation focuses on diagnosing and characterizing the hernia and determining the optimal operative approach for repair. Spigelian hernias are well suited for laparoscopic repair, either via a transabdominal intraperitoneal approach or a total extraperitoneal approach (TEP).
Limited data is available to truly support the superiority of one approach over the other. Some reports have suggested that TEP repair results in shorter hospital stays and improved pain control. The TEP approach retains the mechanical advantage of an underlay repair, where increased abdominal pressure serves to promote mesh adherence to the abdominal wall but avoids the potential complications associated with intraperitoneal mesh. We therefore recommend the total extraperitoneal laparoscopic approach for elective repair of spigelian hernias.
Laparoscopic transabdominal repair is indicated when intraperitoneal pathology requires concomitant evaluation or intervention. Open repair should be considered in the emergency setting, in the presence of cardiopulmonary disease contraindicating laparoscopy, or in the cases of large, incarcerated hernias.
Open Repair
The patient is placed in the supine position with arms extended. An incision is made overlying the hernia and carried down to the external oblique. The external oblique fascia is divided in the direction of the fibers, and the hernia sac is identified (Fig. 35.4). The hernia sac is dissected down to edges of the fascial defect, the contents are reduced, and the sac itself is either reduced or ligated and divided. Once the boundaries of the hernia are defined, an appropriate size mesh is selected and fixed within the extraperitoneal space with non-absorbable sutures. The transversus abdominis may be closed primarily over the mesh if this can be accomplished without tension. The external oblique is re-approximated, and the skin and soft tissue are closed in layers.
Intraperitoneal Laparoscopic Repair
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree