■ For malignant cases, a complete oncologic workup is mandatory. A multidisciplinary approach involving surgeon and medical oncologist is preferable. Lymph node and distant organ involvement are evaluated with the CT scan of the abdomen and pelvis and positron emission tomography (PET) scan. Patients with lower tumors in the rectosigmoid junction may need magnetic resonance imaging (MRI) to evaluate tumor local progression into the pelvis and lymph node status.
SURGICAL MANAGEMENT
Preoperative Planning
■ Bowel preparation is traditionally achieved through a polyethylene glycol–based laxative solution and oral antibiotics. This practice has recently been called into question. An accepted alternative is the use of a modified bowel preparation with preoperative enema to clear out the distal stool.
■ In the operating room and under anesthesia, rigid proctosigmoidoscopy is recommended to ensure the level of the lesion is above the rectum and to ensure that the bowel is clean of fecal matter.
■ For noncontaminated cases, prophylactic antibiotics are administered according to the Surgical Care Improvement Project (SCIP) measures.
■ If the cases involve active infection such as those with recurrent diverticulitis or perforation, broad-spectrum antimicrobials with gram-negative and anaerobe bacterial coverage are chosen.
Positioning
■ The patient is placed in a modified lithotomy position with both arms tucked at the patient’s side. The patient is secured with adhesive tape over the chest, without compromising chest expansion (FIG 2). Antislip rubber pads may be used to further secure the patient to the operating room table. It is imperative to ensure proper and secured positioning, as later in the procedure, Trendelenburg position will be required.
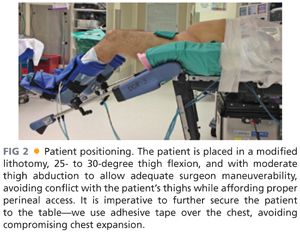
■ The optimal modified lithotomy position is achieved with a 25- to 30-degree thigh flexion and with moderate thigh abduction (FIG 2). This positioning allows adequate surgeon maneuverability, avoiding conflict with the patient’s thighs while affording proper perineal access.
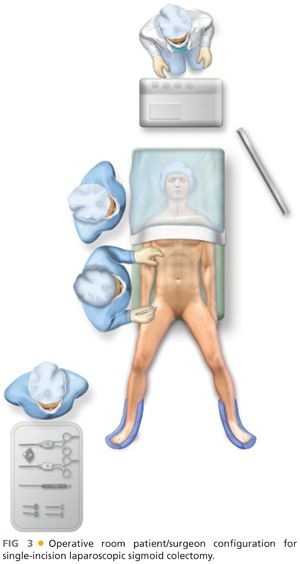
■ For abdominal entry, laparoscopic exploration, and lysis of adhesions, the patient is in supine position. In this portion of the procedure, the surgeon and assistant are located on the right and left side, respectively.
■ Thereafter, the patient is placed in Trendelenburg position with the left side elevated. The surgeon and assistant are located on the right side of the patient with the laparoscopic monitor on the left (FIG 3).
TECHNIQUES
INCISION AND PORT PLACEMENT
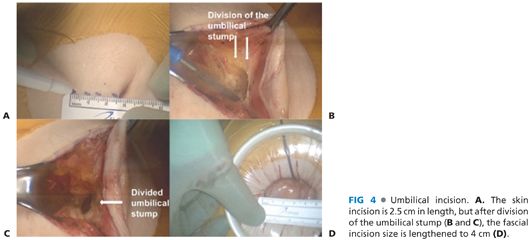
■ Typically, a 2.5-cm vertical umbilical skin incision is performed (FIG 4). The umbilical stump is divided, affording fascial lengthening to 4 cm without modifying the skin incision (FIG 4). Following entry into the abdominal cavity, the single-port device is placed.
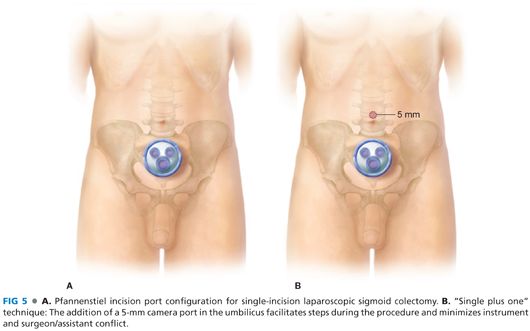
■ An alternative approach is the abdominal entry using a 4-cm Pfannenstiel incision (FIG 5). This modification improves cosmetic outcomes while decreasing wound infection and hernia rates. This approach is challenging, as the instruments are in close proximity with the target operative field, limiting maneuverability. Thus, when this approach is used, we favor a single plus one technique using a Pfannenstiel incision with an additional 5-mm incision for the camera in order to avoid instrument conflict (FIG 5).
■ Prior to port placement, a surgical sponge may be introduced into the abdominal cavity to facilitate retraction later in the procedure.
■ Port placement varies depending on the single-port device used. Once the port is placed, pneumoperitoneum is created and the laparoscopic camera and instruments are introduced.
■ A 30-degree camera and traditional straight laparoscopic instruments are used. Alternatively, articulated instruments may be employed.
■ In order to afford maximal operative reach and to avoid internal and external instrument conflict, bariatric and standard length instruments may be used simultaneously. Moreover, a right-angle light cord adaptor may be used to further decrease conflict.
EXPLORATION AND LYSIS OF ADHESIONS
■ The abdominal cavity is thoroughly examined to assess the disease process and, in oncologic cases, to evaluate the presence of metastatic disease.
■ If required, lysis of adhesions may be safely performed laparoscopically.
DEVELOPMENT OF THE PRESACRAL PLANE
■ With the patient in Trendelenburg position and the left side elevated, the small bowel loops are retracted superiorly and to the right to expose the target operative field. The surgical sponge facilitates small bowel retraction.
■ The sigmoid and rectosigmoid junction are identified and retracted anteriorly and laterally (FIG 6).
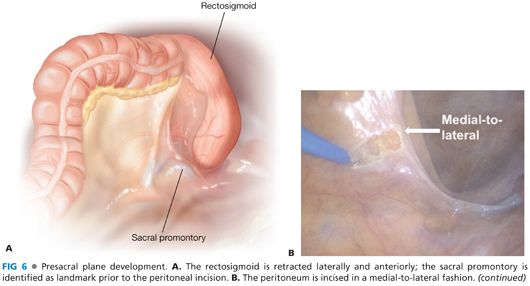
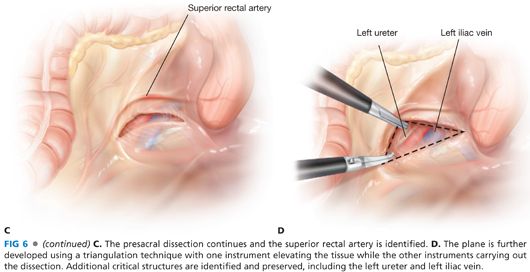
■ The sacral promontory is identified and the peritoneum is incised medially with either a monopolar or bipolar energy device (FIG 6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








