
■ In the case of rectal prolapse, defecography exam preoperatively can provide additional information about the extent of sigmoid colon intussusception and the presence of an enterocele or rectocele (FIG 3).

■ Full colonoscopy should be performed preoperatively to assess the proximal colon and to tattoo the colon proximally and distally to neoplastic lesions (FIG 4).

SURGICAL MANAGEMENT
Preoperative Planning
■ Although the use of a full mechanical bowel preparation continues to be debated, at a minimum the sigmoid and rectum should be cleansed of stool using enemas the night before and morning of surgery in order to drive an anastomotic stapler through the rectum for reattachment. If a complete mechanical bowel preparation is undertaken, oral antibiotics should be included.
■ Although use of laparoscopy has reduced risk of wound infections among patients undergoing colon surgery, risk of deep-space organ infections remains. Broad-spectrum intravenous antibiotics should be given within 30 minutes prior to the abdominal incision. Intraoperatively, antibiotic redosing should be discussed by the surgeon and anesthesiologist for any operation that lasts 4 hours or longer.
■ Risk of deep venous thrombosis is increased among patients with a diagnosis or cancer or inflammatory bowel disease, patients who undergo abdominal or pelvic surgery, and those who have prolonged operations. Patients who undergo laparoscopic sigmoid colectomy fulfill several of these criteria and therefore are at substantially increased risk of venous thrombosis. To reduce this risk, sequential compression devices should be applied to bilateral lower extremities and initiated preinduction, when they are most effective at countering the effects of periinduction venous pooling. After induction, 5,000 units of heparin should be delivered subcutaneously.
Patient Positioning
■ After endotracheal general anesthesia has been induced, the patient is placed in a split-leg or dorsal lithotomy position and secured in a beanbag, with careful attention to padding the extremities, tucking the right arm at the side, and lowering the thighs to be parallel to the floor if possible. If the hips are flexed, the thighs are higher than the abdomen and can hinder the laparoscopic dissection (FIG 5).
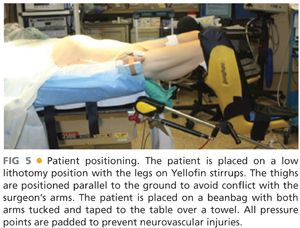
■ Tape the patient across the chest over a towel to secure him or her to the operating room (OR) table.
■ A urinary catheter is placed to decompress the bladder and assist with monitoring urine output during the operation. If the normal anatomic location of the left ureter has been compromised by previous surgery or by an inflammatory condition such as diverticulitis, which can shorten the mesentery and pull the ureter medially, then placement of a ureteral stent or a lighted ureteral stent should be considered.
■ An orogastric tube is placed to decompress the stomach.
■ If the mechanical bowel preparation or preoperative enemas are inadequate, the surgeon should perform a rigid sigmoidoscopy to clear the rectum of stool after endotracheal general anesthesia has been induced.
■ Most hospitals in the United States now require a robust time-out that includes a verbal statement of the patient’s identification, diagnosis, medications and allergies, the planned procedure, and positioning, as well as the names and roles of the operating team and a list of necessary equipment and potential problems.
TECHNIQUES
PORT PLACEMENT AND OPERATING TEAM SETUP
■ The surgeon stands to the patient’s right side, with the scrub nurse next to him or her. The assistant stands to the left side of the table (FIG 6). Two monitors, facing the surgeon and the assistant, are used.

■ A 12-mm umbilical incision is created sharply and extended to the level of the fascia. The fascia is elevated with 2-0 Vicryl tacking sutures and then opened sharply. The Hasson port is then placed within the peritoneal cavity and tacking sutures are pulled up and clamped. This will be used as the camera port.
■ Insufflation with carbon dioxide (CO2) at high flow is initiated to an appropriate pressure of approximately 14 mmHg.
■ After inspection of the abdominal cavity with the laparoscope, three additional 5-mm working ports are placed under visualization in the right upper, right lower, and left lower quadrants of the abdomen (FIG 7).

INFERIOR MESENTERIC ARTERY TRANSECTION
■ The sigmoid colon is inspected and, if necessary, adhesions are lysed. The omentum and small intestine are retracted into the right upper quadrant and the operating table is rotated into Trendelenburg and right side down positions as needed for bowel retraction.
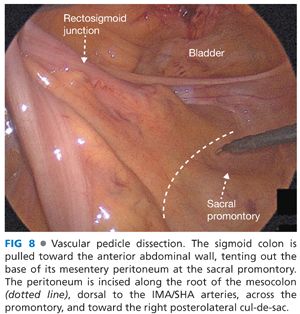
■ The sigmoid colon is grasped broadly with a bowel grasper and elevated toward the anterior abdominal wall to expose the sacral promontory and the medial peritoneal fold (FIG 8). The peritoneum is incised below (dorsal) the inferior mesenteric artery (IMA) and its terminal branch, the superior hemorrhoidal artery (SHA).
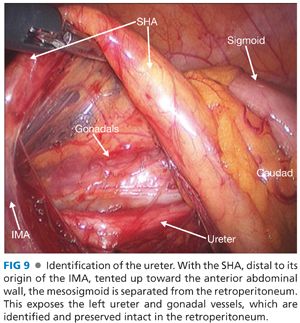
■ The dissection is continued from medial to lateral, beginning the separation of the mesocolon and the retroperitoneum, exposing the left ureter and gonadal vessels, which are identified and preserved intact in the retroperitoneum (FIG 9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








