with this method is that air is compressible, and the pressures recorded may be somewhat lower than the true values.
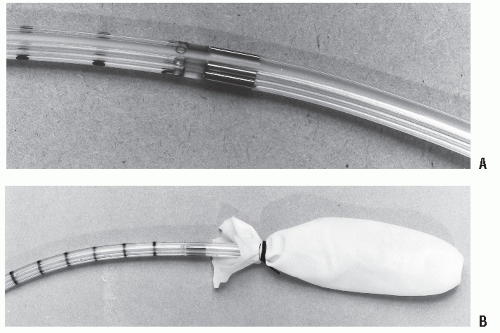
are multiuse catheters with a life span of 1 to 2 years, depending on the number of evaluations performed. Satisfactory cleansing is therefore a priority. This can be accomplished by using activated dialdehyde solution (Cidex; Johnson & Johnson Medical, Inc., Arlington, TX). Proper facilities for the use of this chemical, especially adequate ventilation, are required.
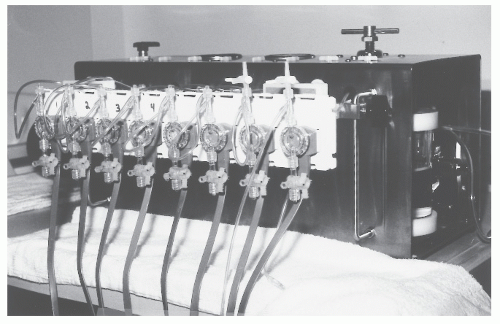 FIGURE 7-3. Eight-channel hydraulic capillary infusion system. (Courtesy of Arndorfer, Inc., Greendale, Wl.) |
TABLE 7-1 Manometry Catheters | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 7-2 Capillary Infusion Systems | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
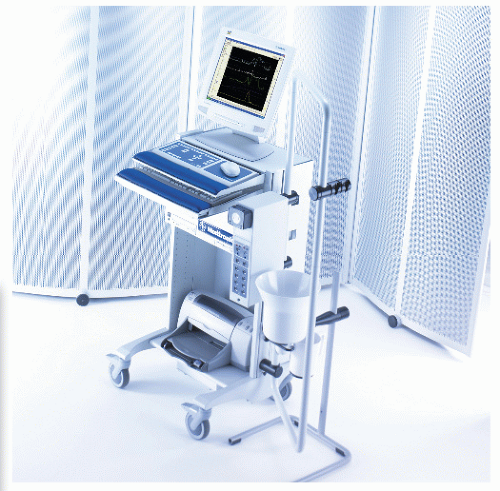
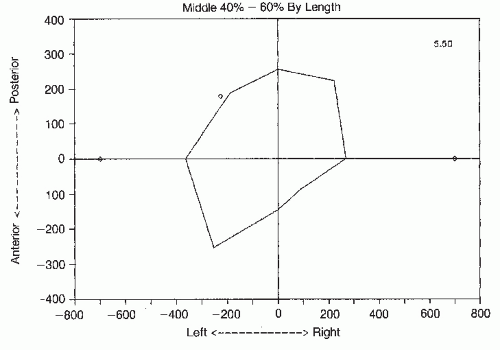
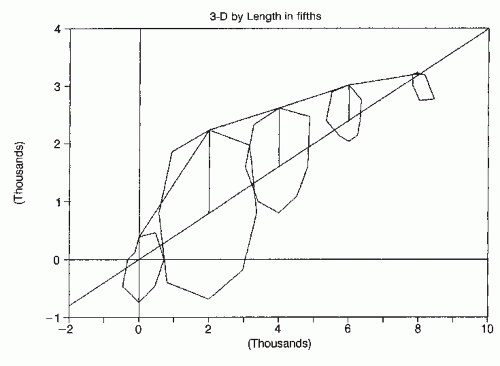
collection for a number of reasons (Figure 7-5). For example, menu-driven software programs can be specially created that contain fixed protocols with instructions and prompts for performing various manometric investigations.36,145,146 Software may also contain the mathematical algorithms for calculating pressure changes. Now, more complex programs are being created that automatically calculate many manometric parameters. Three-dimensional reconstruction of the pressure profile of the anal sphincter can demonstrate sphincter asymmetry and the presence of defects (Figures 7-6,7-7 and 7-8). Several systems now have the capability of integrating and displaying dynamic radiologic investigations with simultaneous motility studies. In addition, computers can also operate accessory equipment, such as probe withdrawal motors, and are excellent for storing data so that tests can be recalled and reviewed. Several manufacturers provide integrated hardware and software systems, some of which can also be used in combination with solid-state catheters (Table 7-3)
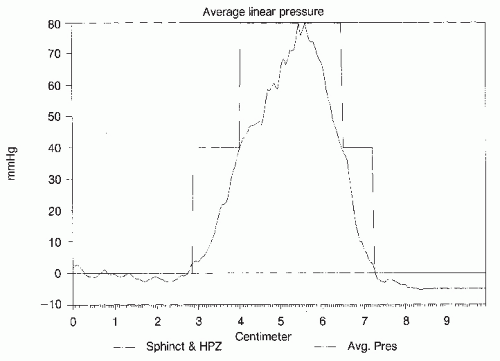
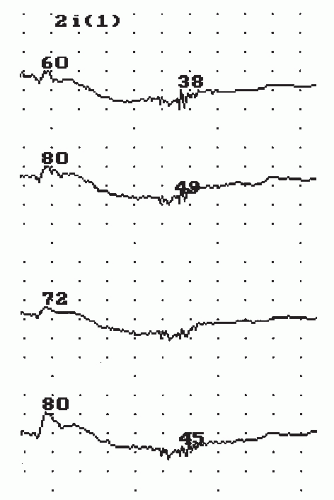
sphincter.175 Three basic patterns are observed. Slow waves are the most frequently encountered. These vary in frequency from 10 to 20 cycles/minute with an amplitude from just above physiologic baseline noise to 15 mm Hg (Figure 7-9).146 They can most often be observed in the region between the proximal border of the sphincter and the area of the maximal average resting pressure.36,130 The clinical significance of these waves is unknown.
TABLE 7-3 Manometry Systems | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||
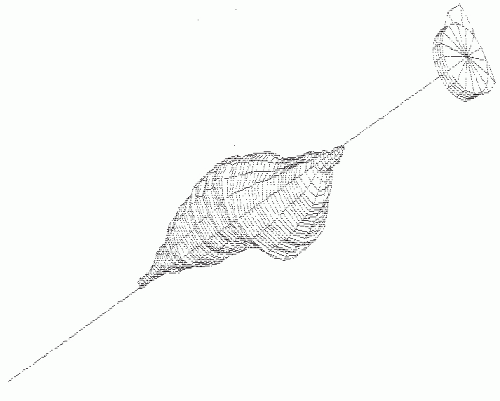 FIGURE 7-8. Three-dimensional reconstruction of same patient illustrated in Figure 7-7 using computer-aided design program. (Courtesy of John A. Coller, MD.) |
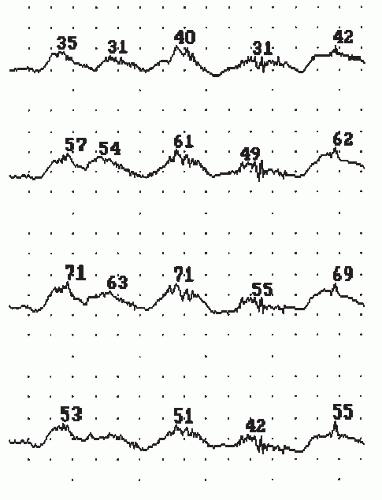 FIGURE 7-9. Slow waves noted in the region of the high-pressure zone. (Polygram software; courtesy of Synectics Medical, Irving, TX.) |
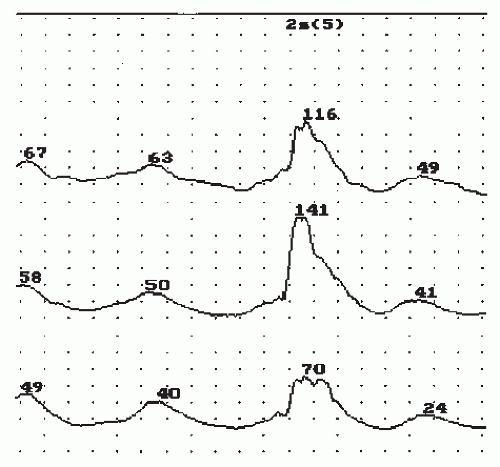 FIGURE 7-10. Intermediate waves in a patient following colonic pouch-anal anastomosis. (Polygram software; courtesy of Synectics Medical, Irving, TX.) |
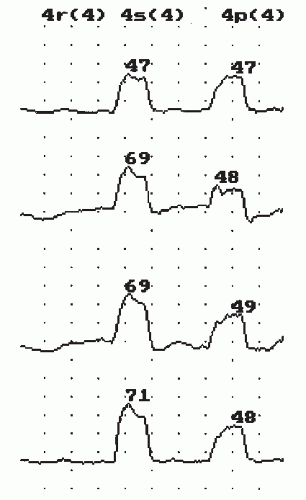 FIGURE 7-11. Rest, squeeze, and push phases of station pull-through manometry recorded at 4 cm from the anal verge. (Polygram software; courtesy of Synectics Medical, Irving, TX.) |
rate of approximately 1 mL/second. The first sensation perceived by the patient is noted as the minimal sensory volume, and the mean intraballoon pressure is noted. Thereafter, balloon filling is continued until the maximum tolerable volume is reached, and again the intraballoon pressure is noted. Using these values, rectal compliance can be calculated from the formula V/P.84 Thus, with a large balloon volume and only a small increase in rectal pressure, the rectum is considered very compliant. In patients suffering from ulcerative colitis, Crohn’s proctitis, or radiation proctitis, the rectum may be poorly compliant in that a small increase in volume will result in a large increase in pressure. When one uses this technique, it is important to know the compliance of the balloon at various stages of insufflation so that it can be subtracted from the pressure measured via the intraballoon ports. Latex balloons may deform along the longitudinal axis with increased infusion of water. This may give a false impression of high rectal compliance.109 As a consequence, some clinicians prefer to use barostat equipment to calculate this parameter, using a noncompliant balloon that does not deform with increasing pressure.
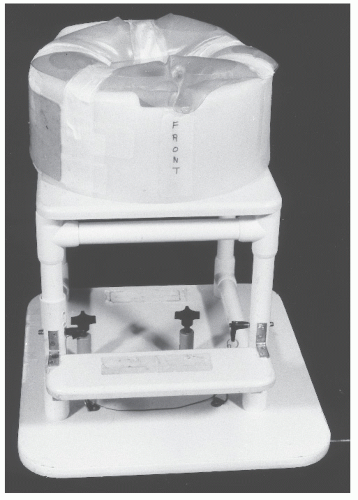
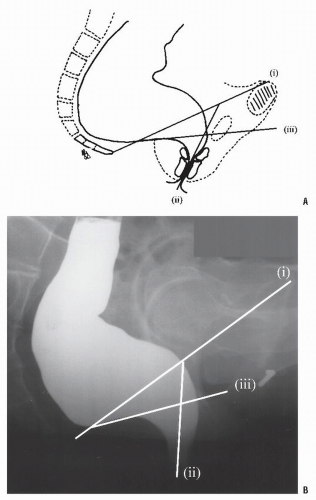
own modifications. With the pelvis examined in profile, x-rays must pass through much tissue, thereby creating considerable absorption of the beam. Movement of the beam caudally, in order to examine anal movement during evacuation or to delineate rectoanal intussusception further, causes x-rays to pass through subcutaneous fat or air. This loss of tissue density and its resultant lack of absorption cause an excessive “flare” or “blooming,” significantly detracting from the quality of the image. Various methods have been developed to address this problem, including the use of one or more water-filled rubber rings,10 specifically designed Perspex water-filled commodes,11 different thickness of leaded plexiglass,134 and the use of carefully positioned copper or lead plates.17
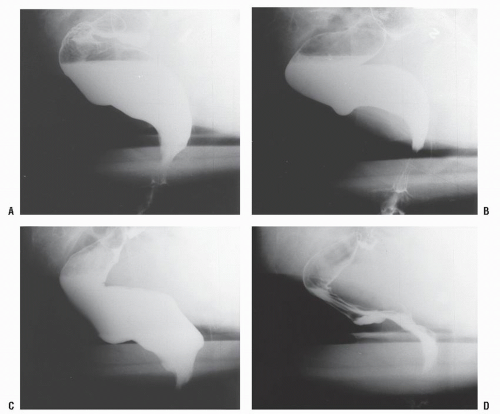
At the commencement of the video, the patients are asked to squeeze, to relax, and then to try to commence evacuation. As elimination starts, a further still picture is taken. Following evacuation, the recording is recommenced while the patient squeezes and pushes in order to check for the presence of an intussusception or nonemptying rectocele. A single still image of the evacuated rectum at rest is also obtained (Figure 7-15B).
is the angle formed by the axis of the posterior rectal wall and the axis formed by the anal canal; it is usually 70 to 140 degrees at rest.59,110 This angle becomes more acute during the squeeze phase (75 to 90 degrees) and becomes more obtuse during evacuation (100 to 180 degrees at maximum strain).86 Some investigators have reported greater anorectal angles in men,153 but most clinicians believe that it is not affected by gender.48 The wide variation in observed normal values is probably due to differences in interpretation.49,59 It has even been suggested that a normal range is impossible to define.153 Therefore, the change in angle seen during the squeeze and push phases is more important than the actual measurement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree