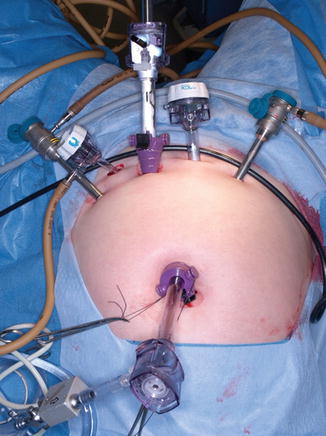
Fig. 19.1
Equipment for a robotic total hysterectomy includes foam egg crate padding to prevent slippage
19.2.2 Equipment and Robotic Column
Two monitors, being held by ceiling booms, are located at each side of the operating table at the level of the patient’s knees. The robotic tower and the tower containing electrosurgical generators and active smoke evacuators are positioned to the right or left of the patient’s feet, depending on the operating room organization.
19.2.3 Trocar Placement and Docking
We prefer the open Hasson transumbilical entry technique with a 12-mm trocar. A CO2 pneumoperitoneum is created once intraperitoneal entrance is confirmed. The robotics laparoscope is used to perform a survey of the upper abdomen and pelvis. Two 8-mm robotic trocars are placed bilaterally, 10 cm distal to and at the level of the umbilicus. An accessory 10-mm trocar is placed 3 cm cranial and equidistant between the umbilical and left lateral ports. An additional 8-mm robotic trocar is placed in the right lower quadrant at the level of the cecum (Fig. 19.2). The patient is placed in enough Trendelenburg to shift the small bowel and sigmoid out of the pelvis.


Fig. 19.2
Trocar placement for a robotic total hysterectomy
The robotic column is side-docked to the patient’s right in our operating room. An EndoWrist monopolar spatula or scissors (Intuitive Surgical Inc., Sunnyvale, CA), depending on the surgeon’s preference, is inserted through the right lateral trocar and an EndoWrist PK bipolar grasper (Intuitive Surgical Inc., Sunnyvale, CA) is inserted through the left lateral trocar. EndoWrist ProGrasp forceps (Intuitive Surgical Inc., Sunnyvale, CA) is inserted through the right lower quadrant trocar as the fourth arm, and is used for retraction.
A Thermoflator (Karl Storz, El Segundo, CA) and a high-flow insufflator at 30 L/min are used. Reusable insufflation tubes are attached to the trocar valves for passive smoke evacuation and dropped by gravity into a bottle containing saline solution.
19.2.4 Hysterectomy Technique
This section follows our technique of robotic hysterectomy and bilateral salpingo-oophorectomy [8]. The pelvic peritoneum is incised at the level of the pelvic brim laterally and parallel to the ovarian vessels to identify the ureter (Fig. 19.3). A peritoneal window is created between the ovarian vessels and the left ureter, isolating the ovarian vessels and preventing ureteral injury (Fig. 19.4). The ovarian vessels are sealed and transected by the first assistant using a vessel-sealing device. The broad ligament is opened anteriorly and posteriorly and the cardinal ligament, left (Fig. 19.5) and right (Fig. 19.6), is sealed and divided by the assistant next to the cervix. The vesicovaginal space is dissected by pulling ventrally on the bladder anteriorly, assisted by placing a vaginal manipulator in the anterior vaginal fornix. With the vesicovaginal space fully dissected, the cervicovaginal junction is then identified without (Fig. 19.7a) and with the assistance of a vaginal manipulator (Apple probe) (Fig. 19.7b). This is an important aspect of any endoscopic hysterectomy.
A colpotomy is started anteriorly at the 12 o’clock location and completed in a circumferential fashion. The uterus and adnexa are removed through the vagina, and a sterile occluding balloon, inflated with 60 mL of water, is placed in the vagina to maintain the pneumoperitoneum until the cuff is closed. The cuff is left open until the nodal dissection is completed, allowing the removal of the nodes through the vagina. When this is completed, the cuff is closed with interrupted figure-of-eight sutures or a continuous suture using 2-0 polydioxanone (Fig. 19.8), incorporating uterosacral ligaments at each angle.

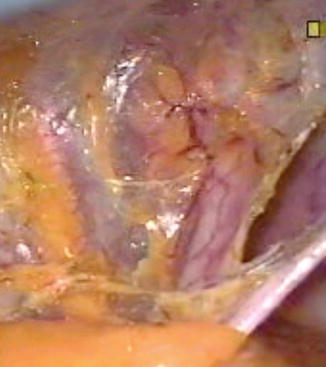
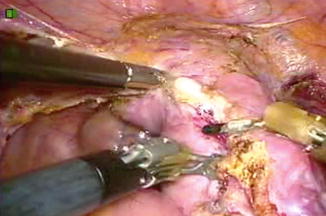
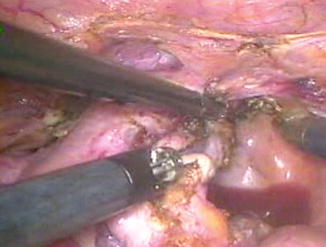
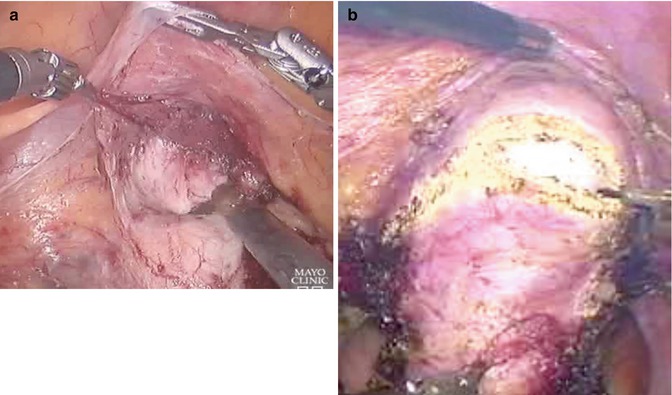


Fig. 19.3
The pelvic peritoneum is incised to identify the ureter
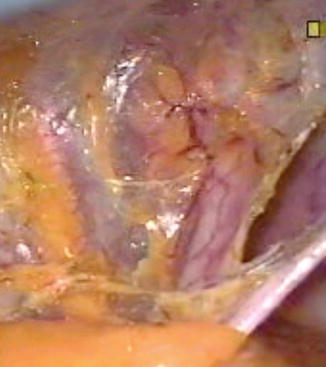
Fig. 19.4
To prevent ureteral injury, a peritoneal window is created between the infundibulopelvic (IP) ligament and the left ureter
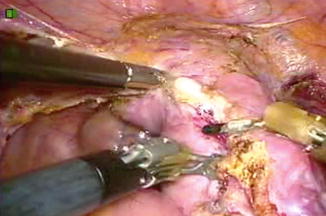
Fig. 19.5
The left cardinal ligament is sealed and divided
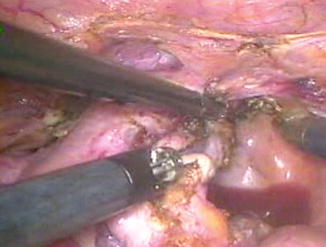
Fig. 19.6
The right cardinal ligament is sealed and divided
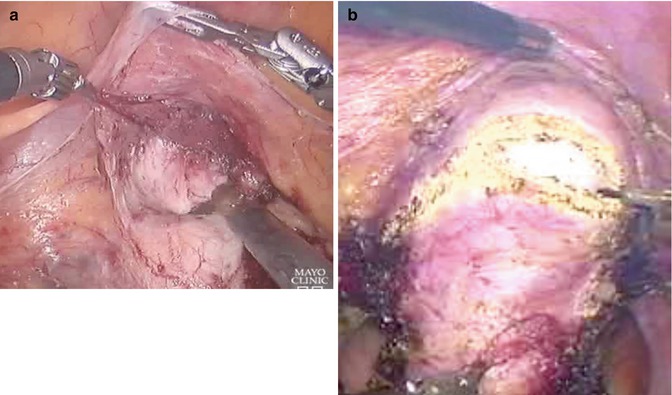
Fig. 19.7
The cervicovaginal junction is then identified without a vaginal manipulator (a) and with the assistance of a manipulator (Apple probe) (b)

Fig. 19.8
After the colpotomy, the cuff is closed with interrupted figure-of-eight sutures or a continuous suture using 2-0 polydioxanone
19.2.5 Pelvic Lymphadenectomy Technique
A pelvic lymphadenectomy is performed by dissecting the paravesical space (Fig. 19.9) and occasionally the pararectal space (Fig. 19.10). The anatomic borders of the paravesical space are medially, the superior vesical artery; laterally, the external iliac artery; anteriorly, the pubic ramus; and posteriorly, the parametrium. The dissection is carried down to the levator ani, being careful to identify the obturator nerve. The margins of the pararectal space are medially, the ureter; laterally, the internal iliac artery; anteriorly, the parametrium; and inferiorly, the levator muscle. The superior margin of the pelvic lymphadenectomy is the bifurcation of the common iliac arteries (Fig. 19.11) and the distal margin is the inguinal ligament. The external iliac nodes overlying and lateral to the external iliac vessels are removed (Fig. 19.12), followed by the superficial lateral common iliacs (Fig. 19.11), and the internal iliac and obturator nodes (Fig. 19.13). The common iliac artery and vein, the external iliac and internal iliac arteries, the anterior bifurcation vessels of the internal iliac artery and the obturator nerve, should be clearly visible at the completion of the pelvic lymphadenectomy (Fig. 19.14). The nodes are sent for intraoperative frozen section. If the pelvic nodes are positive or tumor extends to the cervical stroma, the remaining nodal groups of the internal iliac artery and the deep lateral and medial common iliac nodes are removed.
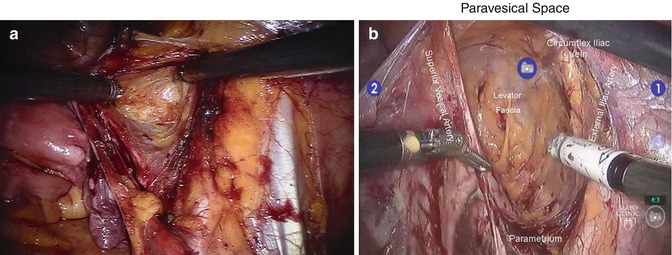
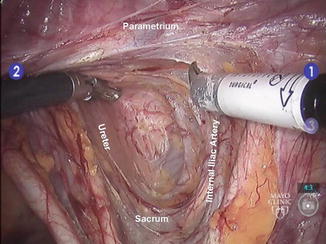

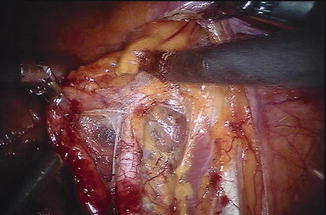
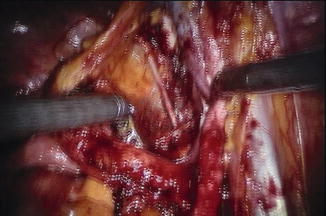
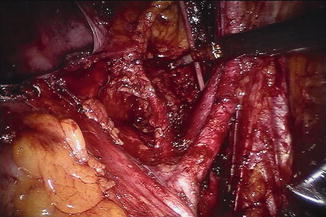
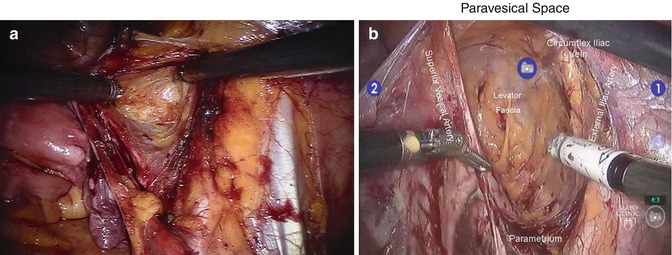
Fig. 19.9
(a, b) Pelvic lymphadenectomy is performed by dissecting the paravesical space
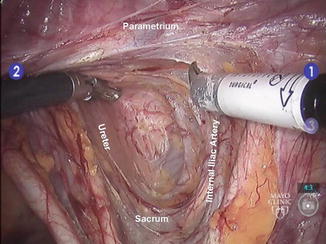
Fig. 19.10
Pelvic lymphadenectomy occasionally involves dissecting the pararectal space

Fig. 19.11
Lateral common iliac arteries. The bifurcation of these arteries is the superior margin of the pelvic lymphadenectomy
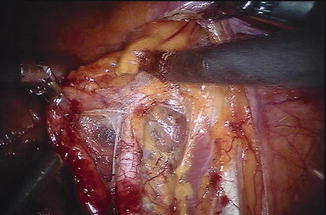
Fig. 19.12
The external iliac nodes overlying and lateral to the external iliac vessels are removed
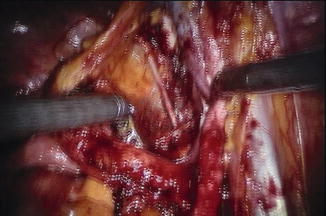
Fig. 19.13
Obturator nodes
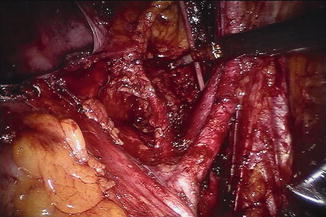
Fig. 19.14
At the completion of the pelvic lymphadenectomy, the common iliac artery and vein, the external iliac and internal iliac arteries, the anterior bifurcation vessels of the internal iliac artery, and the obturator nerve should be clearly visible
19.2.6 Aortic Lymphadenectomy
Indications for aortic lymphadenectomy include myometrial invasion greater than 50 %, lymphovascular invasion, and positive pelvic nodes. In the presence of indications for aortic lymphadenectomy, the robotic column is undocked after completion of the pelvic operation, and three additional trocars are placed in the lower pelvis. A 12-mm trocar is inserted two or three fingerbreadths suprapubically and one or two fingerbreadths to the left of the midline. Two accessory trocars are placed 2 cm caudally and equidistant to the right and left of the 12-mm trocar (Fig. 19.15). The operating table is rotated 180°, so that the patient’s head is now where her feet were located before and vice versa. (This rotation requires a longer intravenous line, longer endotracheal tubing, and cessation of assisted ventilation for about 30 s.)
The robotic column is then advanced to the patient’s head or side-docked to the right shoulder. An EndoWrist monopolar spatula or scissors (Intuitive Surgical Inc., Sunnyvale, CA) is placed through the left robotic trocar and attached to the right robotic arm. An EndoWrist PK bipolar grasper (Intuitive Surgical Inc., Sunnyvale, CA) is placed through the right lower quadrant robotic trocar and attached to the left robotic arm. The assistant sits or stands between the patient’s legs and uses a fan retractor with the left hand to retract the duodenum and pancreas ventrally while the right hand is used for a vessel-sealing device, suction-irrigation, and lateral retraction of the sigmoid mesentery.
A small incision is made on the peritoneum overlying the mid portion of the right common iliac artery and extended to the aortic bifurcation (Fig. 19.16). The left renal vein is identified and the duodenum and pancreas are retracted ventrally by the assistant, with a fan retractor (Fig. 19.17). The right aortic nodes over the vena cava and aorta are excised first, as well as the interaortic nodes if there is a separation between those two vessels (Fig. 19.18). The dissection is extended cranially until no nodal tissue is present, usually slightly above the right gonadal vein entrance site into the vena cava. The inframesenteric left aortic lymph nodes are exposed by extending the peritoneal incision about 5 cm from the aortic bifurcation caudally and overlying the left common iliac artery (Fig. 19.18). The sigmoid mesentery is retracted laterally by the assistant. The left inframesenteric nodes are removed from the bifurcation of the aorta to the inferior mesenteric artery.
The infrarenal nodal area is exposed by dividing the inferior mesenteric artery with a vessel sealing device at its origin from the aorta and by lateral retraction of the left colon mesentery by the assistant (Fig. 19.19). The infrarenal nodes are removed from the stump of the inferior mesenteric artery to the left renal vein, and medial to the left ovarian vein (Fig. 19.20). A second lumbar vein is found passing through this nodal group in about one-third of patients, originating in the lumbar spine and draining directly to the left renal vein or, less frequently, to the left gonadal vein.